Dermatofibrosarcoma protuberans (DFSP) is the most common skin sarcoma. With a slow growth, it has an intermediate malignancy due to its low metastatic potential, but with high infiltrative capacity and local recurrence. Surgery continues to be the main treatment for both primary and recurrent DFSP, and Mohs micrographic surgery or its modified ‘slow Mohs’ variant are considered the techniques of choice.
We present the case of a 69-year-old male patient who had been referred to us due to a 40-year-old skin lesion in the left iliac fossa with progressive growth. The lesion was previously biopsied, but no conclusive diagnosis had been reached.
Examination revealed a brown, indurated, papilliform plaque with poorly defined edges and an ulcerated nodule on the surface that extended from the left iliac fossa to the pubis, measuring approximately 17 × 11 cm. No lymphadenopathies, masses, enlarged organs or other suspicious lesions were palpable.
Magnetic resonance imaging (MRI) revealed a 13 cm plaque with an area of maximum infiltration of 5 cm (to the left of the midline), which was in contact with the anterior rectus in the lower abdominal wall. The computed tomography scan showed no metastases in other organs.
The pathology results of the incisional biopsy reported DFSP, with a frequent myxoid pattern (CD34 +, S100−).
Treatment was started with imatinib to reduce the tumor. Eleven months later, the MRI ruled out involvement of the anterior rectum, and treatment was completed with Mohs micrographic surgery.
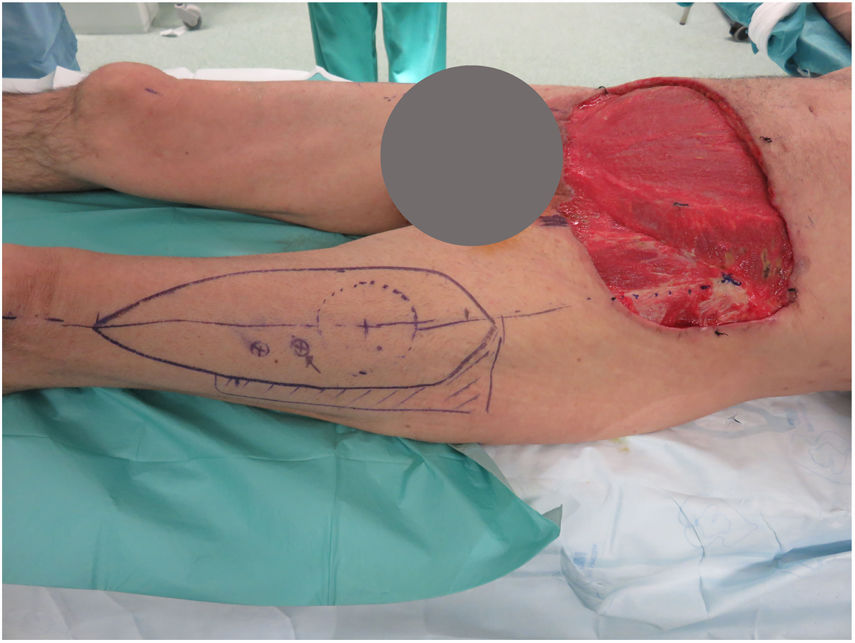
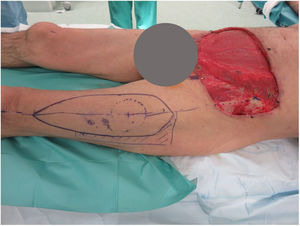
Five sessions of deferred Mohs were conducted, resulting in an defect below the navel measuring 24 × 40 cm to the root of the penis and 4 cm below the inguinal ligament, which included the left external oblique and pre-rectal fascia (Fig. 1). It was reconstructed by means of abdominoplasty (pulling down the upper abdominal wall), with a remaining defect of 24 × 8 cm, which was covered with a pedicled anterolateral flap of the left thigh (based on 2 perforators), including the fascia lata for reinforcement of the abdominal wall (Fig. 2).
In the immediate postoperative period, a small area of necrosis was observed in the distal area of the flap. We re-operated, performing debridement and coverage with a Limberg-type flap, with no new complications.
Two years later, the patient does not have local recurrences or evidence of distant disease.
DFSP is a locally aggressive fibrohistiocytic skin tumor with low metastatic potential. Clinically, it usually presents as a single, asymptomatic, erythematous-purplish, brown or pink plaque that evolves by slowly increasing in size and developing nodules. Initially, it is located on the skin but may later invade the fascia, muscle or bone. Its most frequent location is the trunk, followed by the extremities and, finally, the head and neck.1,2
The fundamental pillar of treatment consists of a multidisciplinary approach (oncological surgeons, plastic surgeons, dermatologists, pathologists, oncologists) focused on correct surgical resection. Resection with wide margins (2−4 cm) has a 20% recurrence rate due to eccentric growth in the form of ‘tentacles or pseudopods’. For this reason, Mohs micrographic surgery or its modified variant ‘slow Mohs’ is considered the technique of choice, since it studies 100% of the margins. In this manner, complete resection is achieved, preserving as much healthy tissue as possible, providing a recurrence rate of around 1%.3 The 3-year recurrence rate is 50%, and the 5-year rate is 75%.4 The series reviewed in the literature estimate a 10-year survival rate of 99.1%.5 Neoadjuvant or adjuvant treatment usually consists of radiation therapy or imatinib. 80%–90% of DFSP are characterized by translocation t (17; 22), which generates a chimeric product (fusion gene) COLIAI-PDGFβ that results in an overproduction of PDGFβ by tumor cells. Imatinib is an oral tyrosine kinase inhibitor specific for PDGF that can benefit patients with an unresectable locally advanced lesion, or those with metastatic disease.6
When the resection of a DFSP is located in the abdominal wall, and the resulting defect is large and complex, reconstruction can be quite a surgical challenge. According to their location and depth, defects are classified as superficial (skin and subcutaneous) or deep (myofascial). There are several reconstructive methods, from direct closure to grafts or flaps that may or may not be associated with mesh. The flaps can be regional (rectus abdominis, external oblique) or distant, both pedicled and free (anterolateral thigh, rectus femoris, tensor fasciae latae).7
In our experience, the anterolateral thigh (ALT) flap, described by Song in 1984, is a useful tool in complex reconstructions in the lower abdomen. It is a versatile flap (with fasciocutaneous, adipocutaneous or musculocutaneous types), used as a free flap in head and limb reconstruction, and pedunculated in abdominoperineal reconstruction. Its vascularization depends on the septo- or musculocutaneous perforators of the descending branch of the lateral circumflex femoral artery. The advantages of this flap compared to other reconstructive techniques are that it provides a large amount of skin with a reliable pedicle, dissection is easy and morbidity of the donor area is low, often with direct closure.8,9
Please cite this article as: Garrido Ríos S, Bustos Martínez G, Olaizola Zubicarai MI, Fernández de Misa Cabrera R, Garrido Ríos AA. Dermatofibrosarcoma protuberans en pared abdominal inferior. Reconstrucción con colgajo anterolateral de muslo. Cir Esp. 2020;98:630–632.