The aim of this study was to evaluate the strategy and efficacy of a hyperglycemia treatment program supervised by Endocrinology.
MethodsAll patients with type 2 diabetes hospitalized at the vascular surgery department over a 12 month period were retrospectively reviewed. Clinical characteristics and hyperglycemia treatment during hospitalization, at discharge and 2–6 month after discharge were collected. Glycemic control was assessed using capillary blood glucose profiles and HbA1c at admission and 2–6 months post-discharge.
ResultsA total of 140 hospitalizations of 123 patients were included. The protocol to choose the insulin regimen was applied in 96.4% of patients (22.8% correction dose, 23.6% basal-correction dose and 50% basal-bolus-correction dose [BBC]). Patients with BBC had higher HbA1c (7.7±1.5% vs. 6.7±0.8%; P<.001) and mean glycemia on the first day of hospitalization (184.4±59.2 vs. 140.5±31.4mg/dl; P<.001). Mean blood glucose was reduced to 162.1±41.8mg/dl in the middle and 160.8±43.3mg/dl in the last 24h of hospitalization in patients with BBC (P=.007), but did not change in the remaining patients. In 22.1% patients with treatment changes performed at discharge, HbA1c decreased from 8.2±1.6 to 6.8±1.6% at 2–6 months post-discharge (P=.019).
ConclusionsThe hyperglycemia treatment protocol applied by an endocrinologist in the hospital, allows the identification of the appropriate therapy and the improvement of the glycemic control during hospitalization and discharge, supporting its efficacy in clinical practice.
El objetivo de este estudio fue evaluar las estrategias terapéuticas utilizadas y la eficacia de un programa de tratamiento de la hiperglucemia supervisado por Endocrinología.
MétodosEstudio retrospectivo de todos los pacientes con diabetes tipo II ingresados en Cirugía Vascular en un periodo de 12 meses. Registramos las características clínicas y los datos relacionados con el tratamiento de la hiperglucemia durante la hospitalización, al alta y a los 2-6 meses postalta. El control glucémico se evaluó mediante los perfiles glucémicos y la HbA1c al ingreso y a los 2-6 meses postalta.
ResultadosSe incluyeron 140 hospitalizaciones de 123 pacientes. El protocolo para la selección de la pauta de insulina se aplicó en el 96,4% de los pacientes (22,8% correctora; el 23,6% basal-correctora y 50% basal-bolo-correctora [BBC]). Los pacientes con BBC tenían HbA1c inicial (7,7±1,5% frente a 6,7±0,8%; p<0,001) y glucemia media el día del ingreso más elevadas (184,4±59,2 frente a 140,5±31,4mg/dl; p<0,001). La glucemia media se redujo en la mitad (162,1±41,8mg/dl) y en las últimas 24 h del ingreso (160,8±43,3mg/dl) en los pacientes con BBC (p=0,007), pero no se modificó en el resto. En el 22,1% de los pacientes en los que se realizaron modificaciones del tratamiento previo al alta, la HbA1c se redujo de 8,2±1,6 a 6,8±1,6%, a los 2-6 meses postalta (p=0,019).
ConclusionesLa aplicación por personal experto del protocolo de tratamiento de la hiperglucemia en el hospital permite identificar el tratamiento adecuado y mejorar el control glucémico durante la hospitalización y al alta, confirmando su eficacia en condiciones de práctica clínica.
The prevalence of type 2 diabetes mellitus (DM2) in Spain is 13.8%,1 and patients with diabetes have a higher probability of being hospitalized due to the comorbidities associated with the disease.2 This justifies the elevated prevalence of diabetes in hospitalized patients, which is more than 50% in patients hospitalized for coronary revascularization.3 Moreover, hyperglycemia during hospitalization is associated with poorer prognosis, longer hospitalizations and increased costs.4–8 Nonetheless, hospital discharge is a highly important event in patient care. It involves transferring the responsibility for treatment back to the patient, and generally the Primary Care Physician, and it is a period that is vulnerable to treatment discontinuity and possible adverse drug events.9–12 Randomized observational studies indicate that the control of hyperglycemia can reduce complications during hospitalization in medical and surgical areas,11,13,14 and that the strategies to organize hypoglycemic medication at discharge will improve post-discharge glycemic control.15–17 Therefore, it is important to prevent and treat hyperglycemia during hospitalization and to adjust the medication prescribed at discharge with what the patient was using before admittance.
There are currently guidelines and consensuses for the treatment of hyperglycemia in non-critical hospitalized patients7,11,18,19 that recommend avoiding oral diabetic agents and using standardized protocols with insulin regimens that contemplate baseline, nutritional and correction components. However, although there are data to indicate that these programs are safe and effective,14,17,20–23 there is very limited information about their implementation in practice during hospitalization and especially the adaptation of treatment at discharge.
At our hospital, the Endocrinology Department is responsible for the treatment of patients with diabetes hospitalized in the Vascular Surgery ward. This circumstance has enabled us to apply a hyperglycemia management protocol by expert staff in diabetes management, which is a unique opportunity to determine the characteristics and effectiveness of these programs in conditions of optimal use. Therefore, the objectives of the present study are: (1) to determine the characteristics of the insulin regimens used during the hospitalization of patients in the Vascular Surgery Ward, as well as any modifications in treatment upon discharge taking into account the personal and socio-familial characteristics of the patient and his/her diabetes; and (2) to evaluate the efficacy and safety of the program.
MethodsWe conducted a retrospective observational study that consecutively included patients with DM admitted to the Vascular Surgery Ward from April 2011 to March 2012. For the analysis, patients with type 1 diabetes were excluded. The study was approved by the hospital Ethics Committee and was performed in accordance with rules for proper clinical practice.
Procedures During HospitalizationAt our hospital, the Endocrinology team monitors patients who are hospitalized daily in the Vascular Surgery unit and have previously or newly diagnosed diabetes (glycosylated hemoglobin [HbA1c] greater or equal to 6.5%).
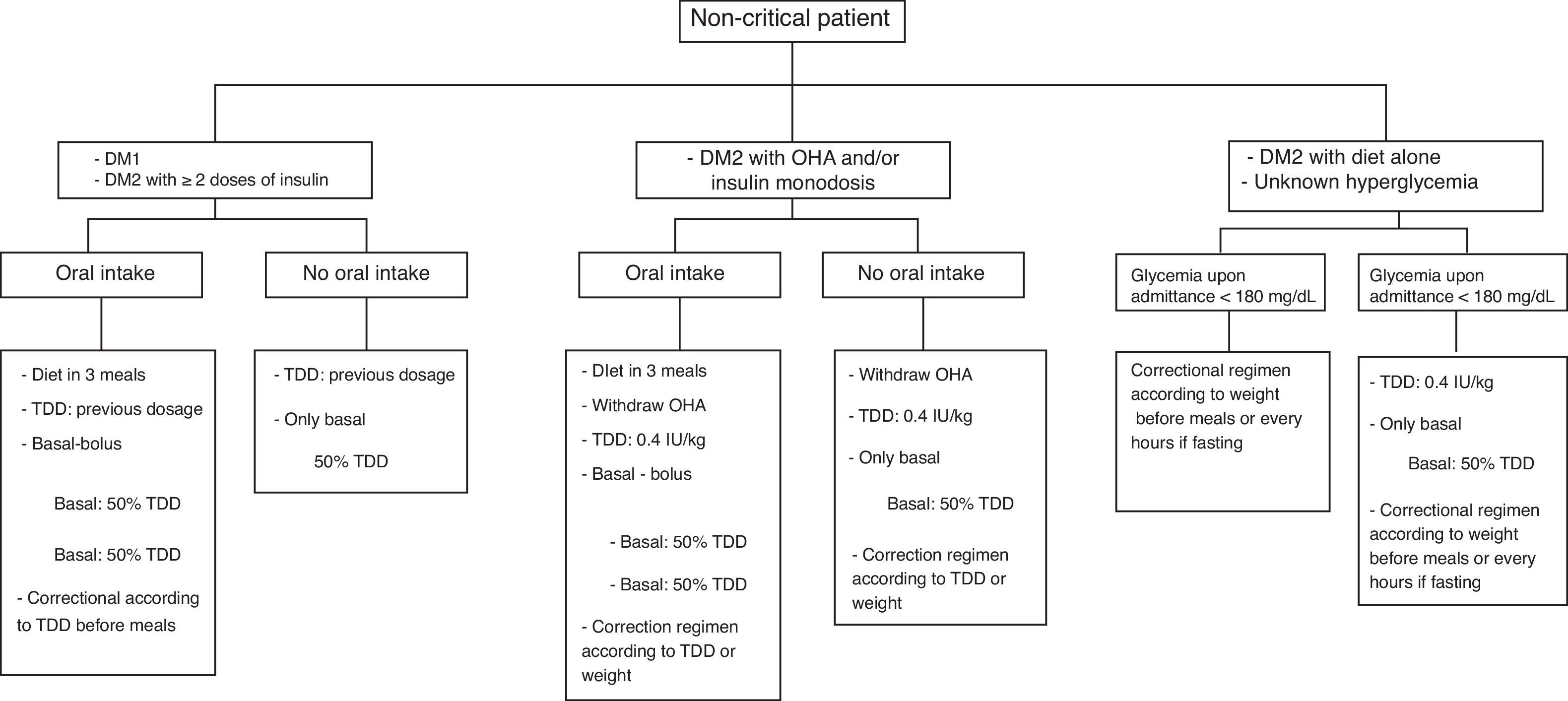
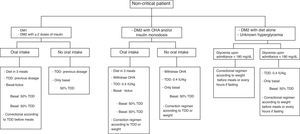
For all patients, at the time of admittance we requested HbA1c and established the treatment regimen within the first 24h in accordance with the protocol of our institution, which is based on the Spanish Consensus for the management of hyperglycemia in hospital19 (Fig. 1). The selection of the insulin regimen (correctional, basal plus correction, or basal-bolus-correction [BBC]) was made on an individual basis, following the protocol that contemplated the patient's previous treatment, glycemic profile within the first 24h, clinical situation and nutrition. The diet was calculated according to the caloric needs of patients and distributed in 3 daily doses, except in those patients who followed treatment with NPH insulin in 2 doses, in which case the diet was distributed in 5 daily meals.
Treatment algorithm for hyperglycemia during hospitalization at the Hospital de la Santa Creu i Sant Pau. DM: diabetes mellitus; TDD: total daily dose; OHA: oral hypoglycemic agents. Source: Adapted from Pérez et al.19
A minimum of 4 capillary blood glucose tests were done per day (pre-prandial and at 12 am) with Accu-Chek Aviva® glucometer (Roche, F. Hoffmann-La Roche, Basel, Switzerland). Glycemic profiles were reviewed daily, and adjustments were made to treatment to reach and maintain pre-prandial plasma glucose levels between 100 and 140mg/dL.
Discharge ProcedureIn order to establish the treatment at the time of discharge, we followed the criteria from the Spanish Consensus for discharge treatment.12 Briefly, we considered treatment prior to admittance, the degree of prior control determined by HbA1c upon admittance, the degree of glycemic control during hospitalization and clinical situation at discharge, as well as the degree of autonomy and family support. In patients transferred to a skilled nursing facility, the regimen was not modified.
The follow-up upon discharge was done at the Primary Care center or with the patient's specialist, except in patients with poor metabolic control, those who were discharged with complex insulin regimens or those who were being previously monitored at the hospital. All the patients with new insulin treatment or who required complex insulin regimens received basic education about diabetes by the nursing team in the hospital unit, which included injection techniques, self-testing, recognition and management of hypoglycemia.
Upon discharge, all patients were given a report with clinical data and recommendations for treatment after discharge, both dietary as well as pharmacological, blood glucose monitoring and follow-up.
VariablesWe retrospectively collected variables recorded in the hospital and Primary Care files that were related with diabetes (evolution time, prior treatment, HbA1c, micro and macrovascular complications), reason for hospitalization, processes and associated cardiovascular risk factors. The degree of control during hospitalization was assessed using the recorded glycemic profiles, which included the 3 pre-prandial blood glucose levels and the 12am glycemia. For the statistical analysis, glucose levels were evaluated the first day of hospitalization, mid-hospitalization, and the last day of hospitalization. We recorded mild hypoglycemia (below 70mg/dL with or without symptoms) and severe cases, defined as those that required the administration of glucagon or with an altered state of consciousness in the patient.24 For the evaluation of the post-discharge control, we recorded the first HbA1c between 2 and 6 months after discharge.
Statistical AnalysisCategorical variables are presented as absolute values and percentages. Continuous variables are presented as mean±standard deviation (SD) when they have a normal distribution and as median (interquartile range) when they did not. The deviation from normal was confirmed with the Shapiro–Wilk test. The comparisons between the two strategies were performed with the Student's t test for independent samples. The comparison between more than 2 means was done with the ANOVA test and the comparison of several means with intrasubject measurements, with the non-parametric Friedman test. The categorical variables for more than one group were studied with the Chi-squared test. A bilateral P<.05 was considered statistically significant. The statistical study was carried out with SPSS 20.0 software (SPSS Inc.; Chicago, Illinois, United States).
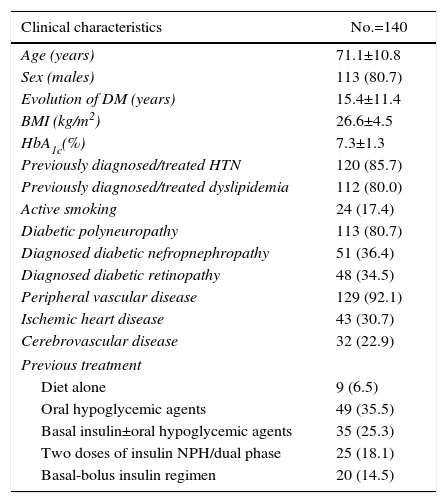
ResultsPatient CharacteristicsA total of 140 hospitalization episodes were included for study, which corresponded with 120 patients with DM2. 85% were admitted for surgical treatment of peripheral vascular disease and diabetic foot (n=119). The surgical procedure performed was revascularization in 62.9% (25.7% revascularization alone; 37.2% revascularization and minor amputation) and major amputation in 22.1%. The remaining 15% were hospitalized for other reasons (n=21). The characteristics of the patients included in the study are shown in Table 1.
Clinical Characteristics of the Patients.
| Clinical characteristics | No.=140 |
|---|---|
| Age (years) | 71.1±10.8 |
| Sex (males) | 113 (80.7) |
| Evolution of DM (years) | 15.4±11.4 |
| BMI (kg/m2) | 26.6±4.5 |
| HbA1c(%) | 7.3±1.3 |
| Previously diagnosed/treated HTN | 120 (85.7) |
| Previously diagnosed/treated dyslipidemia | 112 (80.0) |
| Active smoking | 24 (17.4) |
| Diabetic polyneuropathy | 113 (80.7) |
| Diagnosed diabetic nefropnephropathy | 51 (36.4) |
| Diagnosed diabetic retinopathy | 48 (34.5) |
| Peripheral vascular disease | 129 (92.1) |
| Ischemic heart disease | 43 (30.7) |
| Cerebrovascular disease | 32 (22.9) |
| Previous treatment | |
| Diet alone | 9 (6.5) |
| Oral hypoglycemic agents | 49 (35.5) |
| Basal insulin±oral hypoglycemic agents | 35 (25.3) |
| Two doses of insulin NPH/dual phase | 25 (18.1) |
| Basal-bolus insulin regimen | 20 (14.5) |
The continuous variables are expressed as mean (SD) and categorical variables as n (%).
SD: standard deviation; DM: diabetes mellitus; HbA1c: glycosylated hemoglobin; HTN: arterial hypertension: BMI: body mass index.
Most of the patients were men who had an elevated proportion of peripheral vascular disease and polyneuropathy and had long-term DM2. More than 50% of the patients received treatment with insulin, 2 or more doses in 33%. The complexity of the treatment increased with the time of DM2 progression (P<.001), which was 2.4±3.7 years in those treated with diet, 8.8±6.8 years in those treated with oral hypoglycemic agents (OHA), 16.1±9.8 years in those treated with basal insulin with or without OHA, 27.2±10 years in those treated with 2 doses of NPH and 20.3±10.2 years in those treated with basal-bolus insulin therapy.
Treatment During Hospitalization22.8% of the patients received only correctional insulin (n=32), 23.6% basal plus correction (n=33) and 50% BBC (n=70). In 3.6%, the previous regimen was maintained with 2 doses of NPH insulin (n=5), corresponding with patients with good prior control and a minor surgical procedure. The patients treated with BBC, when compared to the remaining patients, had a longer DM evolution time (19.6±1.4 vs. 11.1±9.6 years; P<.001), worse HbA1c upon admittance (7.7±1.5% vs. 6.7±0.8%; P<.001), elevated mean glycemia the first 24h (184.4±59.2 vs. 140.5±31.4mg/dL; P<.001) and more complex prior treatment (54.4 vs. 11.4% ≥2 insulin doses; P<.001). The BBC regimen was related with longer hospitalization (14.5±10.4 vs. 10.3±6.3 days; P=.004).
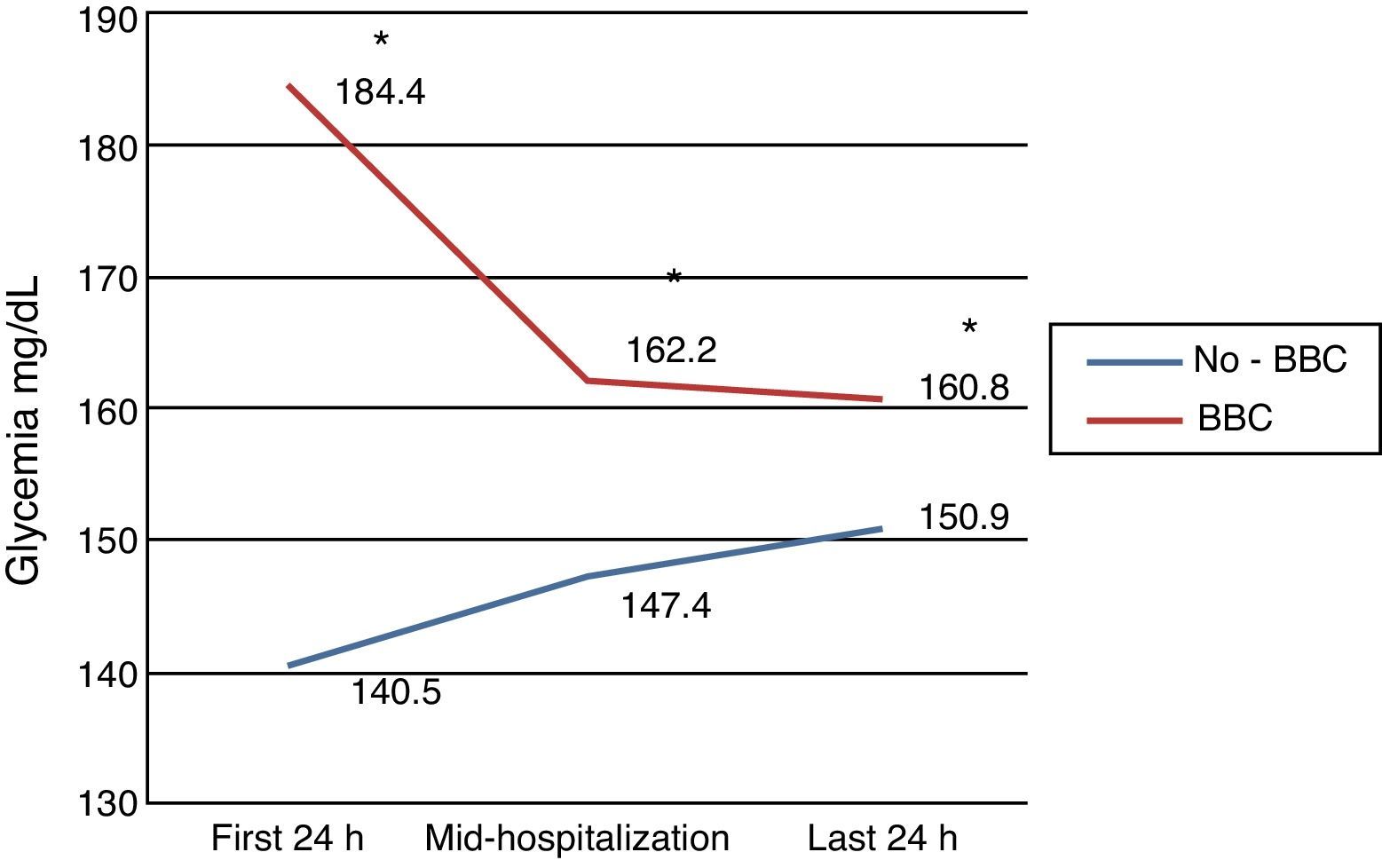
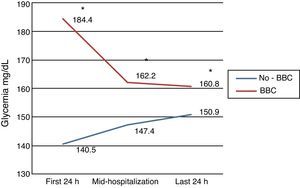
Degree of Control During HospitalizationMean hospital stay was 12.4±8.9 days, and 7 patients (5%) died during hospitalization. Mean glycemia on the first day of hospitalization was 162.3±52mg/dL, mid-hospitalization 154.6±40.6mg/dL and in the last 24h 155.8±41.5mg/dL. In patients treated with correctional insulin or basal plus correction, there were no differences in glycemia levels in the first 24h, mid-hospitalization or in the last 24h of hospitalization (140.5±31.4mg/dL vs. 147.4±38.4mg/dL vs. 150.9±39.3mg/dL, respectively; P=.094). In patients treated with BBC, glycemia on the first day of hospitalization (184.4±59.2mg/dL) dropped significantly mid-hospitalization (162.1±41.8mg/dL) and in the last 24h of hospitalization (160.8±43.3mg/dL); P=.007 (Fig. 2). In the last 24h of hospitalization, there were no differences in glycemia between those who were and those who were not treated with BBC (P=.162) (Fig. 2).
The prevalence of severe hypoglycemia was 2.1% (n=3) and there were no differences between those not treated and those treated with BBC (2.9 vs. 1.4%; P=.559). 35% (n=49) presented mild hypoglycemia at some time, which was more frequent in patients with BBC (45.7 vs. 24.3%; P=.008).
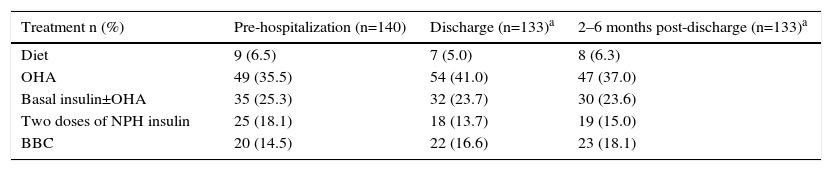
Treatment Modification and Control After Hospital DischargeAt discharge, modifications were made to the prior treatment in 31 patients (22.1%). This subgroup presented a higher HbA1c (8.3±1.6% vs. 6.9±1%; P<.001) but did not differ from the remaining patients for age, BMI, evolution time and mean glycemia during hospitalization. The most frequent change in treatment was the increase or association of OHA (n=20, 64.5%) and the start of insulin therapy (n=7; 22.6%). The distribution of the different treatments upon admittance, at discharge and after 2–6 months are shown in Table 2.
Distribution of Treatments Upon Hospitalization, Discharge and 2–6 Months Post-Discharge.
| Treatment n (%) | Pre-hospitalization (n=140) | Discharge (n=133)a | 2–6 months post-discharge (n=133)a |
|---|---|---|---|
| Diet | 9 (6.5) | 7 (5.0) | 8 (6.3) |
| OHA | 49 (35.5) | 54 (41.0) | 47 (37.0) |
| Basal insulin±OHA | 35 (25.3) | 32 (23.7) | 30 (23.6) |
| Two doses of NPH insulin | 25 (18.1) | 18 (13.7) | 19 (15.0) |
| BBC | 20 (14.5) | 22 (16.6) | 23 (18.1) |
Categorical variables are expressed as n (%).
BBC: basal-bolus-correction; OHA: oral hypoglycemic agents
Follow-up after discharge was carried out in 133 of the hospitalization episodes. In 15.8%, this was at the hospital, in 9.8% with the patient's endocrinologist and in 74.4% at the Primary Care center. In all cases, information was obtained about treatment 2–6 months post-discharge by reviewing the electronic patient records of the hospital or Primary Care center and shared medical records. The value of the post-discharge HbA1c was obtained in 45.7% of the hospitalization episodes (n=64).
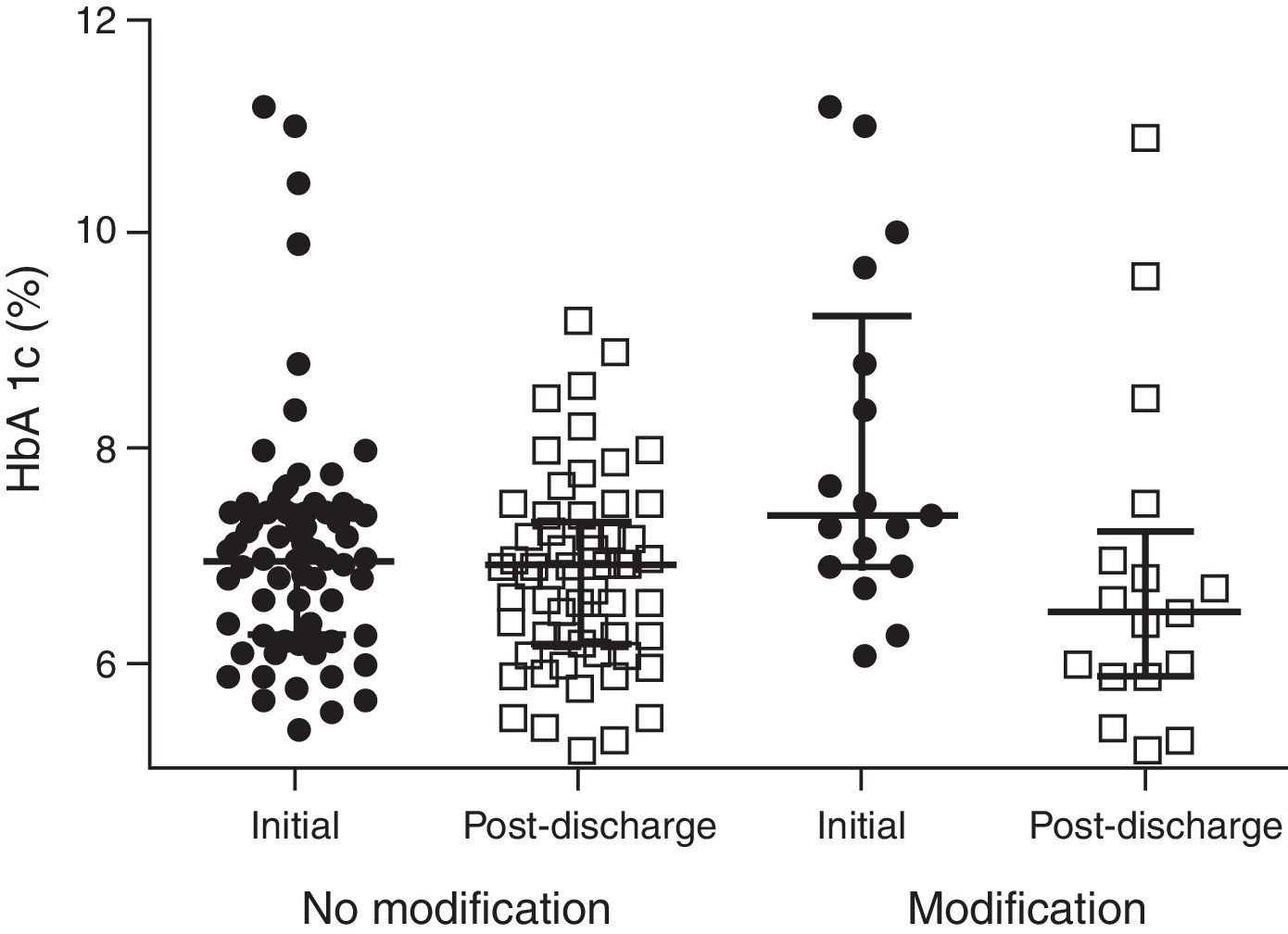
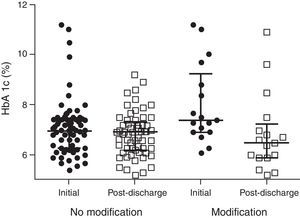
HbA1c 2–6 months post-discharge dropped from 7.2±1.3% to 6.8±1.1% (P=.023). In the subgroup of patients in whom treatment was not modified, there was no difference in the initial or post-discharge HbA1c (6.9±1% vs. 6.8±0.9%; P=.510) (n=49), while in the group of patients with modified treatment there was a significant improvement with reduction in HbA1c from 8.2±1.6% to 6.8±1.6% (P=.019) (n=15) (Fig. 3), and in 75% of patients an HbA1c <7% was reached.
DiscussionIn this retrospective observational study, we have evaluated the hyperglycemia management protocol based on basal-bolus regimens and conciliation of the treatment at discharge, applied by experts in diabetes management. The study offers new information about the characteristics of the insulin therapies used during hospitalization and the adjustments to treatment upon discharge used in daily clinical practice. The study also confirms the efficacy and safety of the regimens used during hospitalization and modifications made at discharge, considering characteristics of the patients and of their diabetes. We believe that the information provided can contribute to facilitating the implementation of hyperglycemia management protocols in hospitalized patients.
The study was carried out in the Vascular Surgery Ward at our hospital. As expected, and due to the reason for admittance, the patients were older in age and had diseases that had been progressing for a long period. They also presented a high rate of chronic complications and cardiovascular risk factors, which explains the high percentage of patients treated with insulin prior to admittance. Direct supervision by an endocrinologist has meant that the hyperglycemia management protocol of our hospital has been applied by experts in diabetes management, patients with individual characteristics and complex diabetes.
Although different consensuses and recommendations7,11,18,19 establish similar strategies for the selection of the different subtypes of basal-bolus regimens (BBC, basal-correction and only correctional) according to prior treatment and glycemia upon hospitalization, to our knowledge there is no information about the proportion of patients who require the different subtypes of basal-bolus insulin during hospitalization. In general, the studies available refer to the proportion of patients in whom the basal-bolus regimen is established, with no consideration given to the subtypes.24,25
In the present study, in 96.4% of hospitalized patients with hyperglycemia, the insulin regimen was applied following the recommendations of the established protocol (Fig. 1). In 50% of the patients, insulin therapy was used with all the components (BBC), in 23.6% the regimen included the basal plus correction component, and in 22.8% only the correctional component. In accordance with the strategy established for the choice of regimen, the patients treated with the 3 components, compared to those treated with the basal plus correction component or only correction, received more complex treatment (≥2 doses of insulin) before admittance, had poorer glycemic control and hospitalizations were longer. One factor that probably contributed to a greater use of the basal plus correction regimen is the expected lower intake of nutrients common in patients hospitalized for surgical processes, which obviously reduces the prandial component.11 In 3.6% of patients, the previous regimen of the patient was maintained with 2 doses of NPH insulin, and the most relevant characteristic was the short duration of the hospitalization.
Overall, the mean glycemias obtained mid-hospitalization and the last day of hospitalization were significantly lower compared to those from the first day of hospitalization, with a low rate of severe hypoglycemia. However, the improvement was exclusively at the expense of the subgroup of patients treated with the BBC insulin regimen and whose mean glycemia the first day of hospitalization was 184.4±59.2mg/dL, while in the remaining patients the mean glycemia the first day was 140.5±31.4mg/dL and was not modified during hospitalization. These findings confirm the results of previous studies14,20,21,23,26 that demonstrate the efficacy of treatment strategies based on BBC to reach and maintain adequate control in non-critical hospitalized patients. Furthermore, the results of this study show that, in clinical practice, an important percentage of hospitalized patients with type 2 diabetes do not require complete BBC. In 46% of the patients, adequate control is maintained by using basal plus correction or correctional-only components, and the strategy utilized is able to identify these patients. There were no differences in the rate of severe hypoglycemia between the BBC group and the remaining regimens, which demonstrates the adequate indication and safety of BBC during hospitalization. Nonetheless, the rate of mild hypoglycemia was elevated and is probably explained by the definition used, which includes all glycemias <70mg/dL, and the context of a hospital surgery ward, where there are often unanticipated changes in nutrition, changes in medication and presence of comorbidities, such as deteriorated renal function.
Hospital discharge is a situation of risk for patients with diabetes. It is the main risk predictor for severe hypoglycemia in seniors,27 and the presence of diabetes increases by 2.6 times the risk for readmittance due to adverse drug reactions.28 However, the transition in diabetes care at discharge receives little attention, and previous studies have demonstrated that it is clearly an underestimated area12 in which the suppression of previous hypoglycemic medication, therapeutic inertia and the lack of post-discharge follow-up are frequent.29,30 Although the relevance of planning hospital discharge is widely accepted31 and specific recommendations have been established,12,19 information about its effectiveness is very limited.15,17 In the present study, excluding the changes in insulin dose without modification of the regimen, the hypoglycemic treatment at discharge was modified in 22.7% of patients. The most frequent modification was increased dosage or the addition of a non-insulin drug and insulinization with the addition of basal insulin or basal-bolus therapy in patients who were transferred to skilled nursing facilities. In the subgroup of patients for whom we had post-discharge information available, the treatment modifications at discharge were maintained in most patients and glycemic control improved, which reinforces the efficacy of this intervention.
The study presents the limitations inherent of an observational design and retrospective data collection; furthermore, we did not have follow-up data for all patients after discharge. However, the study offers information about the application of hyperglycemia management protocols during hospitalization and at discharge under conditions of standard clinical practice in patients hospitalized for surgery and contributes to the comprehension of this area. Due to the patient characteristics, we consider that the information obtained can be applicable to the majority of hospitalized patients, but especially to surgical patients.
Contributions of the Authors- 1.
Caimari F: study design, acquisition and data collection, analysis and interpretation of the results, composition of the article, critical review and approval of the final version.
- 2.
González C: study design, analysis and interpretation off the results, article composition, critical review and approval of the final version.
- 3.
Ramos A: study design, data collection and acquisition, analysis and interpretation of the results, critical review and approval of the final version.
- 4.
Chico A: composition of the article, critical review and approval of the final version.
- 5.
Cubero J.M: data acquisition and collection, critical review and approval of the final version.
- 6.
Pérez A: study design, analysis and interpretation of the results, composition of the article, critical review and approval of the final version.
The authors have no conflicts to declare related with the content of the manuscript.
Please cite this article as: Caimari F, González C, Ramos A, Chico A, Cubero JM, Pérez A. Eficacia de un programa de tratamiento de la hiperglucemia en un Servicio de Cirugía Vascular supervisado por Endocrinología. Cir Esp. 2016;94:392–398.
This study was presented at the conference of the Spanish Diabetes Society in April 2013 (Seville, Spain).