The liver is one of the most frequently affected organs in abdominal trauma. Classically, severe liver trauma (AAST grade ≥ IV) has been a contraindication for liver donation.1 Increased experience and more refined surgical technique allow these organs to be used safely without adding morbidity and mortality to the procedure, thus allowing the donor pool to be expanded.
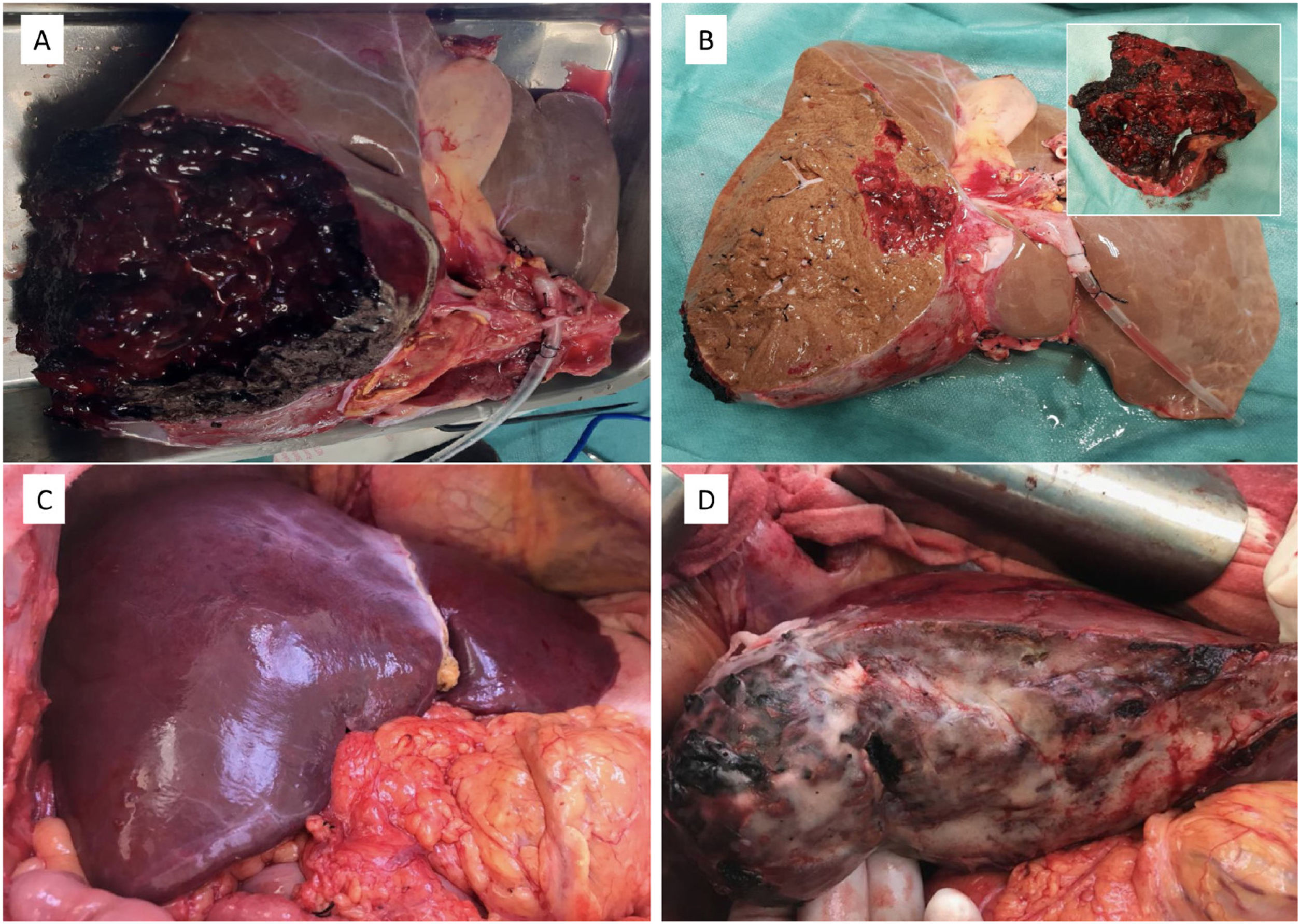
We present the case of a 27-year-old woman with no previous history of interest who was admitted for polytrauma secondary to a traffic accident. During transfer, the patient suffered a cardiorespiratory arrest which lasted 10 min after recovery. The cranial CT scan showed massive subarachnoid haemorrhage and the abdominal CT scan, in addition to other injuries, showed severe liver trauma with a haematoma of about 10 cm with parenchymal disruption affecting segments 6, 7 and part of segment 8 (AAST grade IV) with no associated major vascular and/or biliary injuries. Given the poor prognosis of the brain lesions, optimisation measures for possible organ donation were initiated, but encephalic death occurred a few hours after admission. The maximum dose of noradrenaline was 1.8 µg/kg/min. Peak AST and ALT values were 248 U/L and 231 U/L, respectively, slowly decreasing to 183 U/L and 196 U/L at the time of donation. During extraction, a macroscopically normal liver was observed with a large haematoma on the posterior aspect of the LHD affecting segments 6, 7 and part of segment 8 with no associated major vascular or biliary lesions. Extraction was performed according to the usual technique and subsequently, given the extent of the trauma and the good appearance of the rest of the parenchyma, it was decided to perform an ex situ reduction, eliminating the entire area affected by the trauma (250 g), leaving a sufficient liver remnant with a weight of 1,168 kg (Fig. 1). Parenchymal transection was performed with a cold scalpel, progressively suturing all vascular and biliary nozzles and finally a fibrin sealant was sprayed over the entire surface. The recipient was a 63-year-old male with compensated enolic cirrhosis and secondary hepatopulmonary syndrome requiring oxygen therapy 16 h per day. Liver transplantation (LT) was performed with preservation of retrohepatic vena cava and conventional vascular anastomoses, followed by end-to-end choledocholedocholedochostomy without Kehr. Cold ischaemia time was 445 min and warm ischaemia time 55 min. During reperfusion there was no haemorrhage on the liver section surface and transfusion of blood products was not necessary, and a collagen fibre dressing was applied over the section edge to reinforce haemostasis. The postoperative period was uneventful and the patient was discharged after optimisation of his respiratory status 7 days after transplantation. After 2 years of follow-up, the patient evolved favourably, with complete resolution of the hepatopulmonary syndrome and normal liver function.
For years, the use of severely traumatised livers has been an absolute contraindication for donation, having been associated with higher rates of primary failure and retransplantation.1 However, different studies have shown that with proper donor selection, optimal livers can be salvaged for transplantation.2–4 However, few studies have been published describing the performance of LT with a severely traumatised graft that requires reduction. In 2009, Geenen et al.4 published the results of 15 LTs performed with trauma grafts, the largest series to date. Five cases had trauma ≥AAST grade II, with 100% survival at 3 months and 80% survival at 1 year. In 3 of these cases, liver graft reduction was necessary at bench surgery. In addition, we can find some published cases of living donor LT and heart-stopping donor LT with liver trauma. In 2005, Tucker et al.5 stated that AAST grade I-II liver trauma should not contraindicate liver donation, even in heart-stopped donors. In 2009, Chen et al.6 described the case of a patient with severe liver trauma (AAST grade IV) that had resulted in a complete section of the left hepatic duct impossible to reconstruct and necessitating a left hepatectomy (Table 1). Because the left hepatic lobe (LHL) had adequate volume (>40% of the total liver volume) the patient became a living donor and the LHL was used for LT. The authors stated that all donors with liver trauma should always be considered in the absence of major vessel injury, sufficient parenchymal volume for the recipient and absence of uncontrolled abdominal and systemic septic foci.
Review of published cases of LT with reduced liver grafts with severe trauma (≥ AAST grade 4).
| Author | n | AASTGrades | Liver volume | Complications | Survival |
|---|---|---|---|---|---|
| Chen et al., 2009 | 1 | Grade IV | ≥ 40% | No | Alive (56 days) |
| Geenen et al., 2009 | 4 | 2 Grade IV2 Grade V-2 | – | No | 3 months: 100%1 year: 80% |
| Navarro et al., 2021 | 1 | Grade IV | ≥ 80% | No | Alive (2 years) |
In conclusion, proper selection of donors with severe liver trauma7 and the application of techniques such as graft reduction during bank surgery allows safe liver graft retrieval for LT without increasing the risk of LT-associated complications.
In conclusion, proper selection of donors with severe liver trauma7and the application of techniques such as graft reduction during bank surgery allows safe liver graft retrieval for LT without increasing the risk of LT-associated complications.