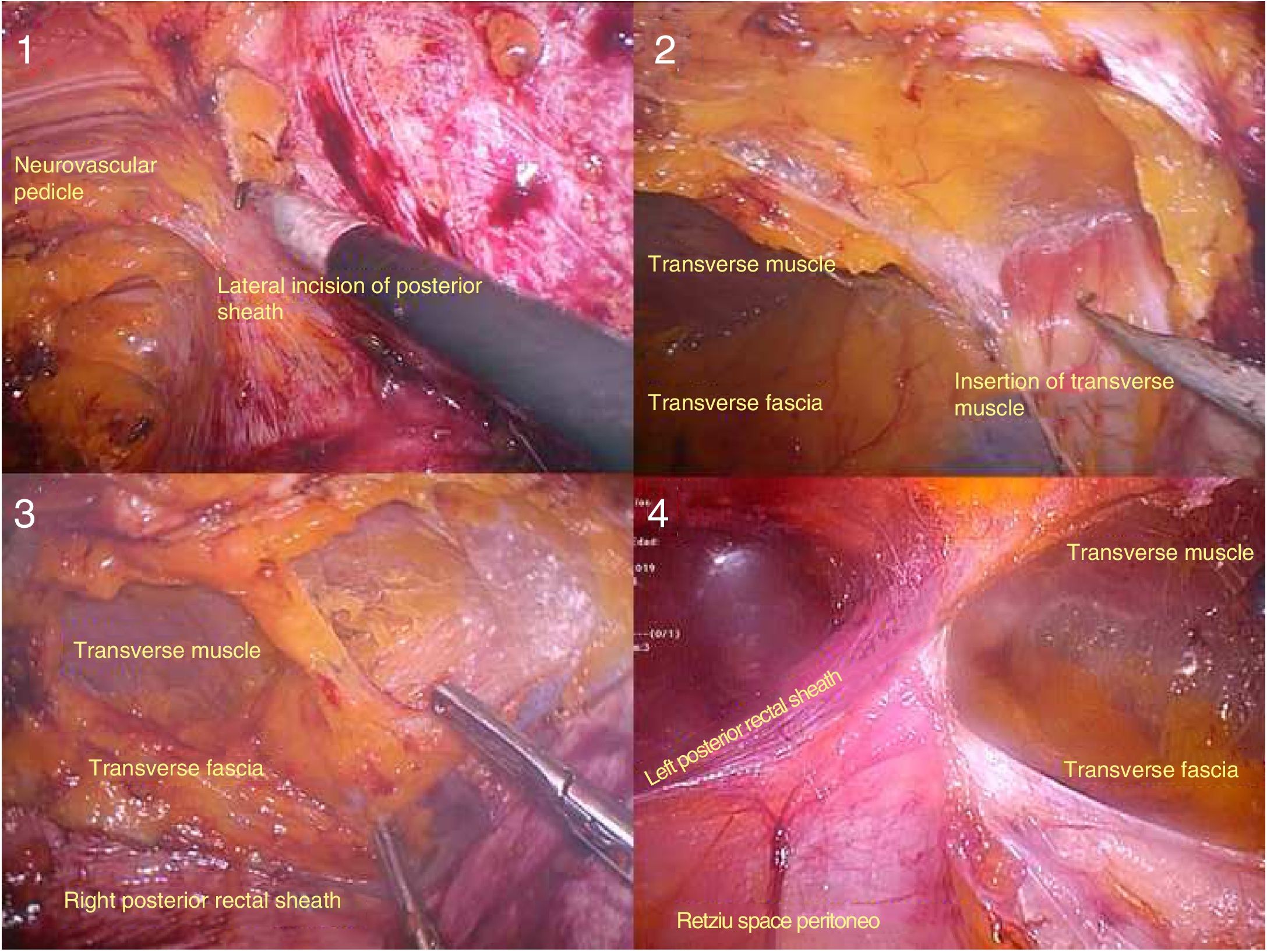
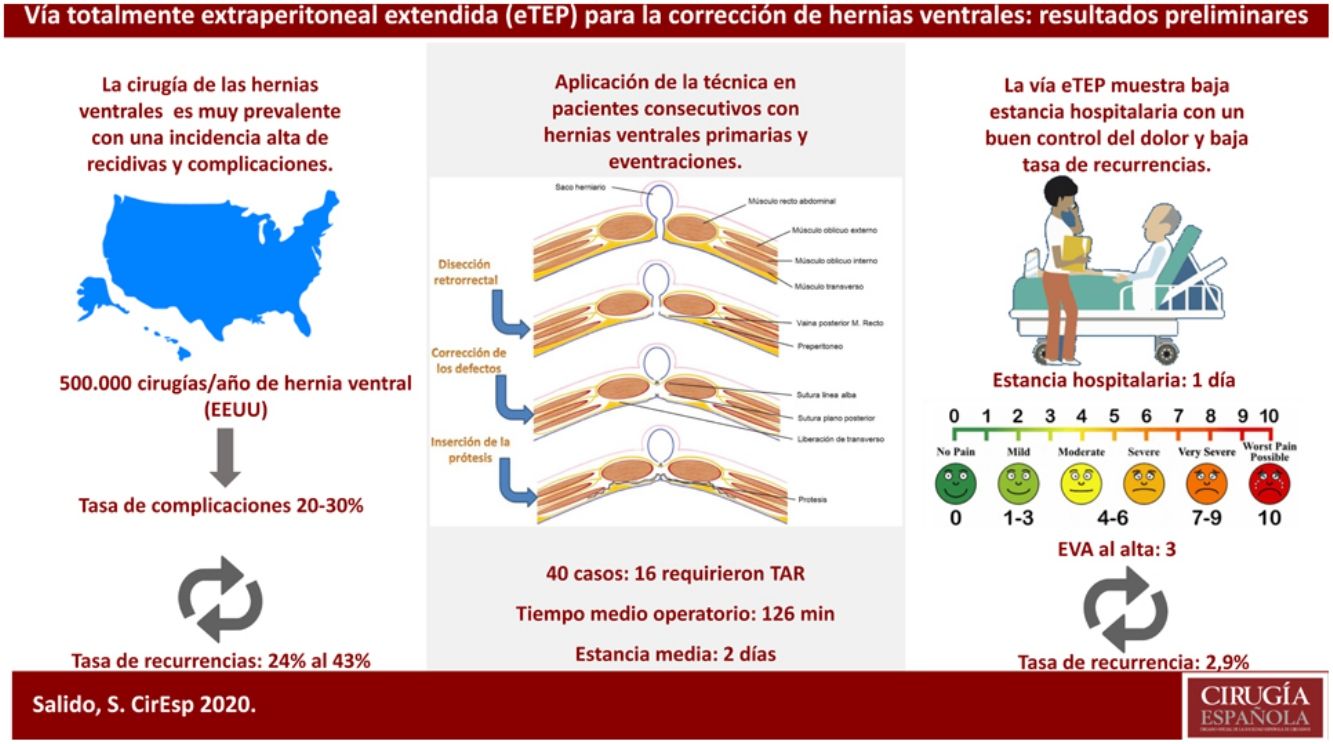
Since the first laparoscopic incisional hernia repair, several minimally invasive procedures have been developed in abdominal wall repair. In 2017, the extended totally extraperitoneal (eTEP) approach for abdominal wall repair was published. We present the results from eTEP implementation at two medical centers by one surgeon.
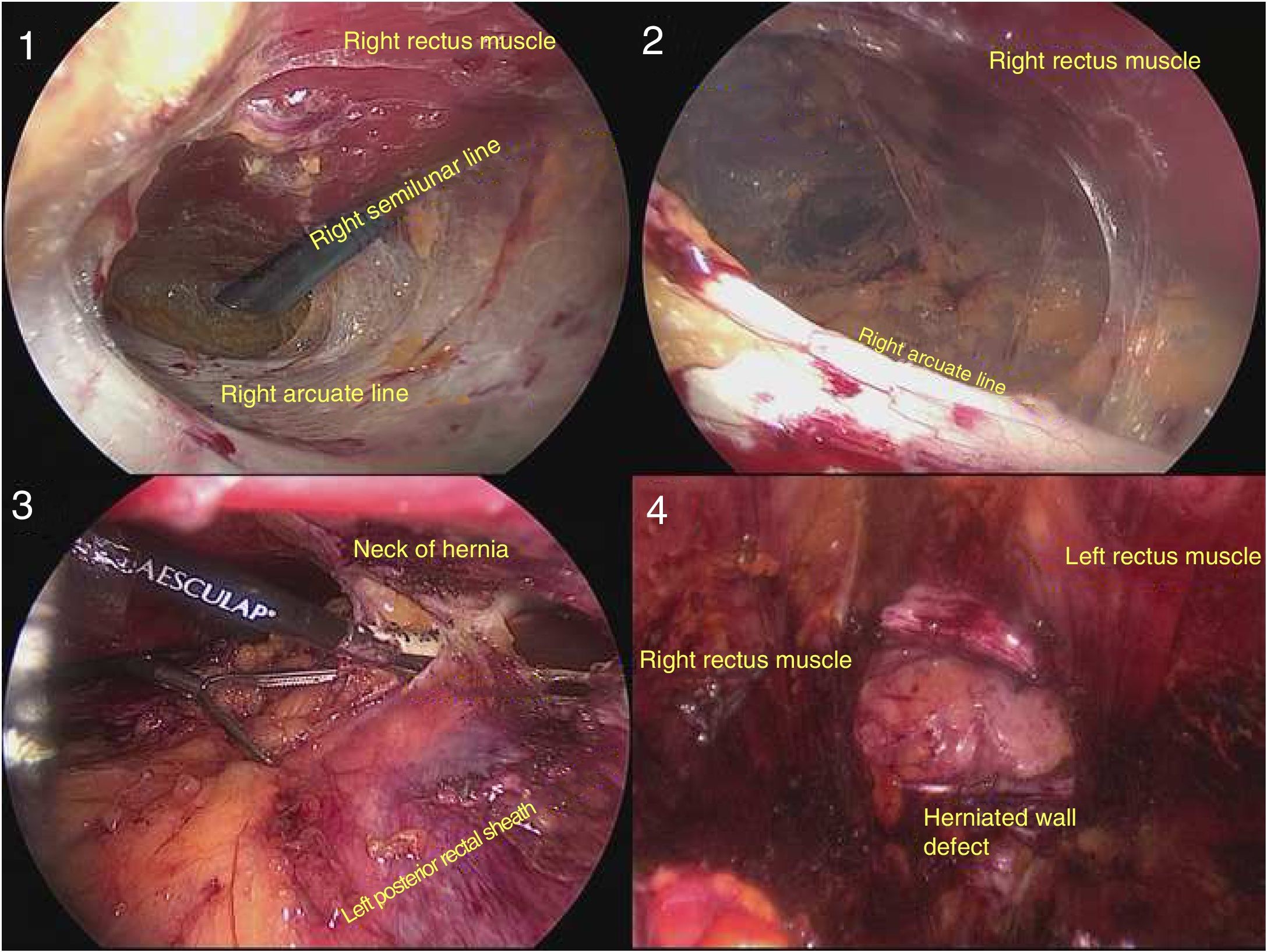
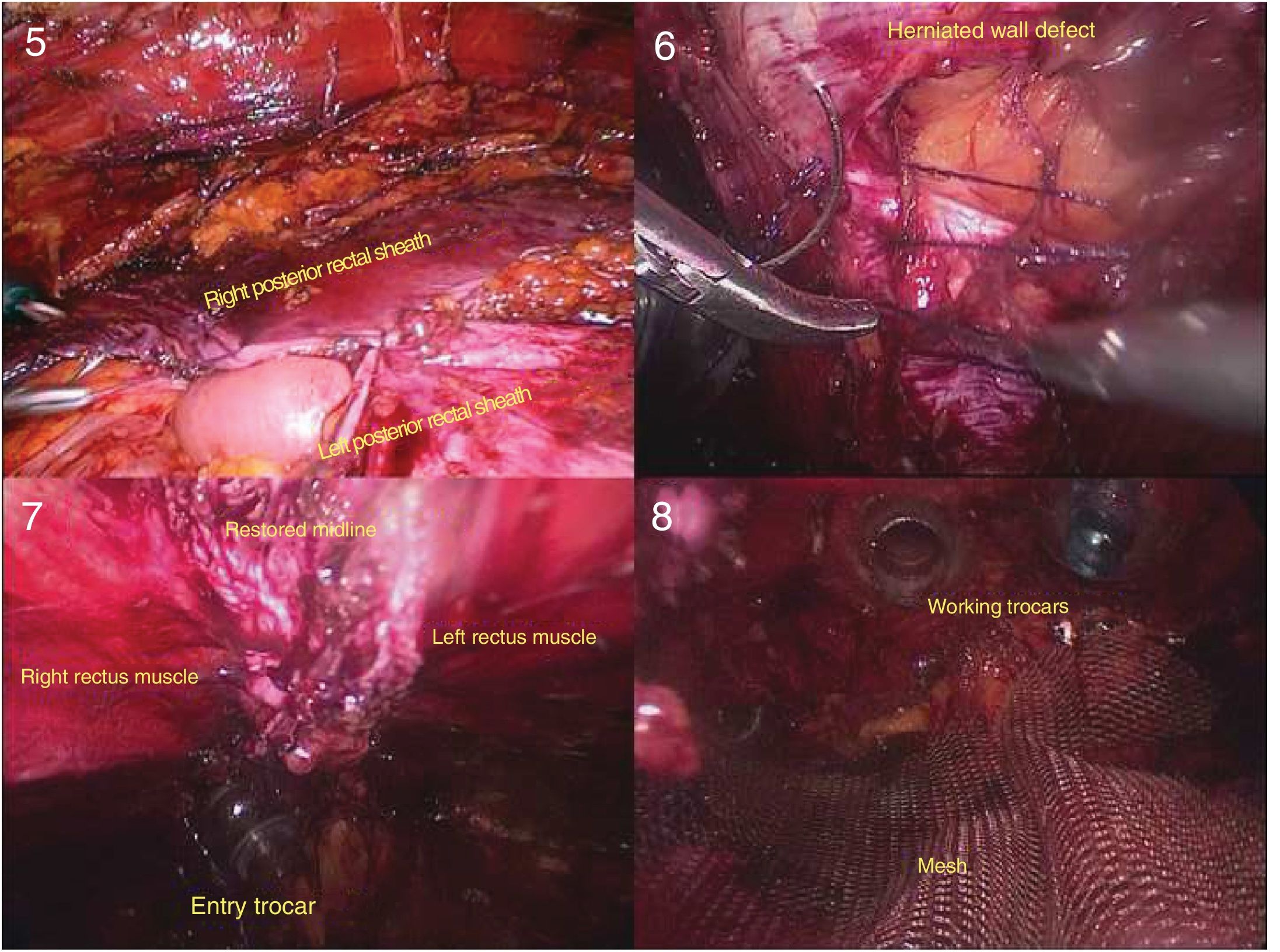
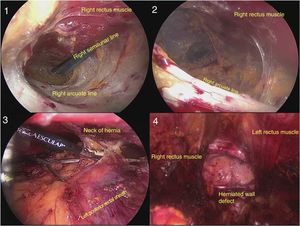
MethodsProspective descriptive study of the implementation of the eTEP approach, with transversus abdominis release (TAR) when needed. The surgical technique was initiated by accessing the space between the rectus abdominis muscle and posterior rectus sheath, connecting this space with the fatty preperitoneal space at the midline and the contralateral retrorectal space. Identification and dissection of the hernia sac is performed in the created cavity. Additionally, posterior component release in a TAR fashion could be done. Finally, closure of posterior plane and linea alba is completed and mesh prosthesis is deployed along the whole dissected space.
ResultsForty patients underwent an eTEP procedure with 20 supraumbilical defects, 10 infraumbilical and 10 lateral hernias. Sixteen cases required a TAR technique. Mean operative time was 126min. Median pain reported the first postoperative day was 3 on the visual analog scale. Median length of stay was 1 day and mean follow-up was 10 months. Only one patient developed recurrence, and two patients underwent reoperation.
ConclusionsImplementation of eTEP in abdominal wall repair is safe. Preliminary outcomes of the eTEP approach in ventral hernia repair show good pain control with less hospital stay.
Desde la primera eventroplastia laparoscópica se han desarrollado múltiples procedimientos en cirugía miniinvasiva de la pared abdominal. En 2017 se publica el acceso endoscópico totalmente extraperitoneal extendido (eTEP) para la reparación abdominal. Se presentan los resultados de la implementación de la técnica en 2 centros por un único cirujano.
MétodosEstudio prospectivo descriptivo de la implementación de la vía eTEP con o sin liberación de transverso (TAR) para defectos de la pared abdominal. La técnica quirúrgica se inicia con el acceso al espacio entre el músculo recto y la vaina posterior, uniendo dicho espacio con el preperitoneo de la línea media y el espacio retrorrectal contralateral. En la cavidad creada se realiza la disección y reducción del saco herniario. Se puede realizar adicionalmente una liberación posterior de componentes tipo TAR. Se realiza el cierre del peritoneo y del defecto fascial y se extiende una prótesis en el espacio definitivo.
ResultadosSe intervinieron 40 casos, 20 casos con defectos supraumbilicales, 10 casos infraumbilicales y 10 en la línea semilunar. Dieciséis casos asociaron TAR. El tiempo quirúrgico medio fue de 126minutos. El dolor mediano por la escala EVA al alta fue de 3. La estancia mediana fue de un día y el seguimiento medio de 10 meses. Un caso mostró recidiva y 2 pacientes requirieron reintervención.
ConclusionesLa reparación de hernias primarias e incisionales abdominales mediante eTEP es segura y reproducible. Los resultados preliminares muestran buen control del dolor postoperatorio y baja estancia.
Minimally invasive surgery (MIS) of the abdominal wall has evolved tremendously, and several different procedures having been developed since the first laparoscopic incisional hernia repair. Initially, endoscopic techniques were described with occlusion of the defect using a prosthetic mesh (intraperitoneal onlay mesh [IPOM]),1 and later laparoscopic closure of the defect was added.2 Subsequently, the need to avoid contact of the mesh with the abdominal content led to the development of transabdominal preperitoneal techniques,3 placing the mesh in the preperitoneal position and later in the retromuscular position.4 Another use for abdominal wall MIS has been the application of component separation techniques, which, in the case of the preperitoneal transabdominal approach, was described for posterior separation, known as transversus abdominis muscle release (TAR).5
At the same time, the totally extraperitoneal (TEP) approach was developed, which had been applied to hernias in the inguinocrural region.6 In 2012, Daes7 also described the extended-view TEP (eTEP) technique, which resolved certain ergonomic problems and expanded the operating field. Finally, both routes converged in 2017 when Belyansky8 published the totally-extraperitoneal access for the correction of ventral hernias, which reproduced the technique described by Rives and Stoppa for endoscopic retromuscular repair. While still not widely used, the endoscopic Rives–Stoppa (eRS) technique offers very positive preliminary results, achieving excellent recurrence and postoperative morbidity rates. Additionally, there is better pain control and a shorter stay compared to techniques like IPOM.9 In addition to the eRS technique for the correction of midline defects, the eTEP access combined with lateral access to the space posterior to the transverse abdominal muscle allows for correction of defects of the semilunar line and abdominal flanks.
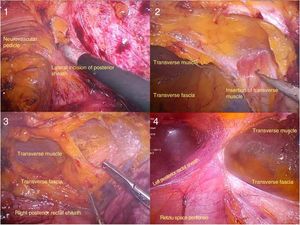
We present initial results after applying the eTEP approach for the correction of primary or incisional midline hernias or lateral abdominal hernias, conducted by our minimally-invasive abdominal wall reconstruction team (Figs. 1–3).
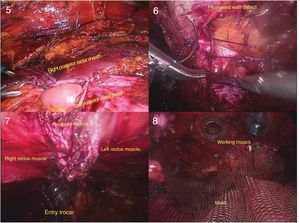
Posterior component separation (TAR: 1) beginning of the lateral dissection of the posterior sheath of the rectus abdominis muscle; (2) progression of dissection in the cranial direction; (3) separation of the transverse muscle of the transverse fascia; (4) ‘down to up’ transverse muscle release maneuver.11
We present a prospective descriptive study with patients undergoing elective surgery for primary or incisional ventral hernia, either midline or lateral, at the Hospital General de Villalba and the Hospital Universitario Fundación Jiménez Díaz. Patients were treated by the same surgeon between April 2018 and December 2019 using the eTEP approach, with or without TAR. The inclusion criteria were: primary or incisional hernias; size W2 (3–10cm) according to the European Hernia Society (EHS) classification10 or multiple hernias whose sum of the defects was greater than 3cm with or without associated diastasis recti; midline and lateral hernias (M and L according to EHS). The exclusion criteria were: defects classified as W3 (greater than 10cm) according to the EHS10; loss of abdominal domain; need to remove previous prostheses, skin resection or scarring; history of previous complicated surgery (previous infection, secondary closure, skin fistulae, mesh extrusion or contained evisceration).
The operating room preparation (Video 1), sRS surgical technique (Video 2) and TAR (Video 3) are explained in detail in the videos of the supplementary material accompanying this article. Antibiotic prophylaxis included one dose of cefazolin (2g, intravenous). In patients with allergy to beta-lactams, 1g of vancomycin was administered. The suture material used was a 2/0 barbed suture for the peritoneal closure, and 0 for the linea alba. The mesh of choice was polypropylene, macroporous and low molecular weight, or titanized polypropylene in cases where minor peritoneal defects remained during dissection. No fixation method was used for the mesh prostheses, and no surgical drains were placed in any case. Antithrombotic prophylaxis with low-molecular-weight heparin was started 12h after surgery if there was no evidence of active bleeding.
Demographic data were collected for age, sex, BMI and ASA classification. Preoperative variables included: primary or incisional ventral hernia, previous incisional hernia repair, number of defects, measurement of wall defects on computed tomography (CT) scan, and location of the main defect according to the EHS classification. Intraoperative variables included: placement of trocars (lower, lateral or upper), surgical time, suture time of the anterior fascial defect, application of TAR, number of defects, mesh size, and ratio between the area of the mesh and the defect. Postoperative variables included: pain on the first postoperative day and at discharge (visual analog scale), registry and classification of complications (Dindo–Clavien12), hospital stay, clinical follow-up after one month, and clinical/radiological follow-up with CT scan after 3, 6 and 12 months to assess recurrence or complication.
The primary objective of the study was to implement the new surgical technique. The secondary objective was to evaluate the preliminary results.
The statistical study was carried out with SPSS® 21.0 software for Windows®. Qualitative variables were expressed as the number of events. Continuous quantitative variables were expressed as mean and standard deviation, and discrete variables as median and range, measures of central tendency and dispersion.
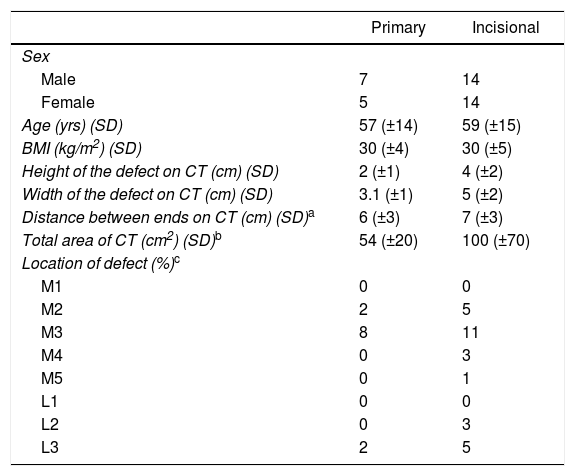
ResultsDuring the study period, 40 cases were treated, including 12 primary hernias and 28 incisional hernias. Patient demographic characteristics and the characteristics of the defects studied by CT are summarized in Table 1. The distribution of patients according to anesthetic risk was ASA I in 4 patients, ASA II in 31 patients and ASA III in 5 patients. Six patients had previous incisional hernia repairs. The eTEP approach was inferior in 20 patients, superior in 10 patients and lateral in 10 other patients. The average surgical time was 126min (±36). The time required for suturing the anterior fascial defect was 19min (±11). The mean area of the mesh used was 400cm2 (±199), with a ratio of 5.5:1 with the hernia defect. Sixteen cases had associated TAR. Two cases required conversion to open surgery. The first was due to a massive rupture of the peritoneum associated with a loss of relaxation, and the open Rives–Stoppa repair was selected. In the second case, eTEP access was not achieved due to the scarring of the midline, which made it impossible to cross. One open Rives–Stoppa repair was also done. In 3 cases, adhesions required adhesiolysis, while in 2 cases the intestinal serosa was sutured. The mean pain score on the VAS scale the first postoperative day was 3 (0–8) and at discharge 3 (0–6). The mean stay was one day (0–17), and 11 patients were treated as day surgery. Data for hospital stay and postoperative complications are shown in Table 2. Two patients had a Dindo–Clavien complication grade of 3B and required reoperation: one on the third postoperative day due to iatrogenic injury during adhesiolysis, with contained perforation to the retromuscular dissection space; and the second for intestinal obstruction due to intraperitoneal adhesions, without recurrence. The rest of the complications recorded were grade 1 of the Dindo–Clavien classification. The median follow-up was 10 months (5–20), and 18 patients had completed at least one year of follow-up. One case was observed of millimetric umbilical recurrence and millimetric persistence of a cranial defect not observed on the preoperative CT scan, which was found intraoperatively due to failure to dissect cranially to the defect treated during surgery. Two cases of dehiscence of the posterior plane closure were found, both asymptomatic and diagnosed by the 3-month imaging tests. In both cases, correction was observed radiologically, with plane adhesion to the mesh at the 12-month follow-up.
Demographic Data and Preoperative Characteristics.
| Primary | Incisional | |
|---|---|---|
| Sex | ||
| Male | 7 | 14 |
| Female | 5 | 14 |
| Age (yrs) (SD) | 57 (±14) | 59 (±15) |
| BMI (kg/m2) (SD) | 30 (±4) | 30 (±5) |
| Height of the defect on CT (cm) (SD) | 2 (±1) | 4 (±2) |
| Width of the defect on CT (cm) (SD) | 3.1 (±1) | 5 (±2) |
| Distance between ends on CT (cm) (SD)a | 6 (±3) | 7 (±3) |
| Total area of CT (cm2) (SD)b | 54 (±20) | 100 (±70) |
| Location of defect (%)c | ||
| M1 | 0 | 0 |
| M2 | 2 | 5 |
| M3 | 8 | 11 |
| M4 | 0 | 3 |
| M5 | 0 | 1 |
| L1 | 0 | 0 |
| L2 | 0 | 3 |
| L3 | 2 | 5 |
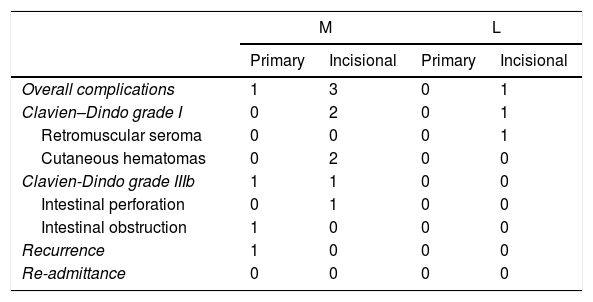
Postoperative Results.
| M | L | |||
|---|---|---|---|---|
| Primary | Incisional | Primary | Incisional | |
| Overall complications | 1 | 3 | 0 | 1 |
| Clavien–Dindo grade I | 0 | 2 | 0 | 1 |
| Retromuscular seroma | 0 | 0 | 0 | 1 |
| Cutaneous hematomas | 0 | 2 | 0 | 0 |
| Clavien-Dindo grade IIIb | 1 | 1 | 0 | 0 |
| Intestinal perforation | 0 | 1 | 0 | 0 |
| Intestinal obstruction | 1 | 0 | 0 | 0 |
| Recurrence | 1 | 0 | 0 | 0 |
| Re-admittance | 0 | 0 | 0 | 0 |
It is key that MIS of the abdominal wall should meet the main objectives of open techniques: complete reconstruction of the wall by restoration of continuity of the aponeurosis, tension-free closure, and mesh placement. The eTEP technique for abdominal repair complies with the principles published by Rives13 and Stoppa14 for open retromuscular repair: reduction of hernia content, closure of the peritoneal or posterior fascial defect, closure of the anterior fascial or midline defect and placement of a sufficiently large prosthetic mesh. Compared to other laparoscopic techniques, a pillar of the eTEP technique is the closure or restoration of the midline. Midline defects cause loss of synergy with the diaphragm during breathing, intestinal herniation with each breath, lordosis and lumbar pain; there is no antagonistic compensation for the dorsal musculature, and retraction of the lateral abdominal musculature occurs. Closure of the midline reduces adverse surgical site event rates15 and the recurrence rate,16 but adds complexity and surgical time to the technique, making it more demanding for the surgeon. In this present study, all midline defects were closed, and concomitant diastases were corrected.
Regarding the plane where the prosthetic mesh is to be placed, the retromuscular position has been proven to have the best vascularization for correct integration of the mesh. In animal models, a greater collagen I/collagen III ratio is observed during mesh integration,17 providing greater force against tension. Preperitoneal or retromuscular mesh has been shown to have the lowest rates of recurrence,18 while MIS provides the lowest rates of postoperative complications.18 Another benefit of the retromuscular plane is to avoid the presence of intra-abdominal foreign bodies and associated complications, as well as the significant reduction in costs associated with mesh, which is already higher in invasive CMI versus open procedures.
It is routinely recommended that the size of the mesh used in laparoscopic surgery should surpass the edges of the original defect by at least 5cm.19 However, this measurement may be insufficient for large defects, as the mesh could migrate or protrude through the defect. According to Laplace's law, the surface size that prevents mesh migration surrounds the entire defect and remains in position due to friction forces in the retromuscular space and the pressure on the abdominal wall. The larger the mesh ‘ring’ surrounding the defect, the greater the adhesion. Tulloh20 calculated that the ratio of the mesh diameter to the diameter of the initial wall defect should be 4 times greater in order to guarantee the previous statement. In the eTEP technique, wide retromuscular dissection is performed in addition to TAR, which enables the surgeon to insert a mesh that is greater in proportion than the wall defect. In the present study, a mesh/defect ratio of 5.5 was observed, which complied with the described ratio. The tendency of the recurrence rate in the present study is low, and the only case registered was in the second patient treated in the series. These data are preliminary, given the short follow-up time. However, previous authors present similar rates.8,21
Penetrating fixation of the prosthetic mesh, usually with ‘tackers’ and the double-crown technique,22 require several applications and are largely responsible for postoperative pain and discomfort, which can lead to acute and chronic pain. In a controlled trial of bilateral laparoscopic inguinal hernia repairs, the authors performed mesh fixation with tackers on one side and no fixation in the contralateral repair; patients experienced higher rates of pain on the side with tacker fixation, measured by the VAS scale, as well as increased discomfort.22,23 Other non-penetrating options can be used, such as the use of adhesives and biological glues, with better postoperative pain results. One study showed better pain control in the first 7 postoperative days in patients treated with eTEP correction versus IPOM.9 In this study, no fixation was performed in any case, and the mean pain score measured by the VAS scale was 4 on the first postoperative day and 3 at discharge. These results allow a significant percentage of cases (27.5%) to be managed on an outpatient basis, given the good pain control despite the extent of retromuscular dissection.
Open abdominal reconstruction can present a significant complication rate due to the extent of the necessary dissection of skin and subcutaneous cell tissue.18 Large dermal-fat flaps, especially in the anterior separation of components, can lead to injury of perforating arterial branches and to complications such as seromas, hematomas, infection and skin necrosis. The eTEP approach minimizes cutaneous aggression by requiring only small incisions for insertion of the trocars.8,21 Retromuscular dissection and TAR do not alter the perforating vascularization of the abdominal wall, avoiding the large cutaneous complications of open surgery. In the present study, there were no major skin complications. Routine use of surgical drains is also not necessary,21 as the presence of subcutaneous seromas is unlikely. The extraperitoneal working chamber maintains partial isolation from the intestinal content, minimizing possible abdominal iatrogenic injury. However, great care is necessary during dissection of the hernia sac, as there may be adhesions to the hernia sac as well as to the midline. In our series, only one out of 3 cases with adhesions had abdominal iatrogenesis, causing an unnoticed lesion due to probable loss of serous membrane and perforation; clinical symptoms were observed on the third postoperative day.
The application of the eTEP technique is complex, and its learning curve is long. The author has needed to complete a learning curve of more than 100 inguinal hernia repairs with TEP. Furthermore, prior to the application of eTEP in ventral hernias, eTEP approaches were performed for inguinal hernias in obese patients, large inguinal hernias, and biopsies of iliac lymphadenopathies for standardization of the technique. The most demanding steps are the crossing of the midline, which is more complex in superior trocar approaches. The absence of a posterior rectus sheath in the lower third of the abdominal wall facilitates the localization of the contralateral muscular belly and spatial orientation. Another critical point is the dissection of the hernia neck, which should be as close as possible to the hernia ring so that the opening of the sac is as small as possible, facilitating its closure. Lastly, the linea alba suture is technically demanding due to the inverse needle position and the tension that the abdominal wall can offer. It is recommended to perform several stitches in a row without exerting tension, and then reduce the pressure of the pneumoperitoneum to 8–6mmHg to then tighten the suture loops made (Video 2).
One strength of the present article is the uniform application of the technique, as the patients had been treated by a single surgeon. However, the limitations include the short follow-up period and the external validity of the application of the technique, as it is a surgery that requires advanced laparoscopic skills.
In conclusion, the repair of primary and incisional abdominal hernias using the totally extraperitoneal route is safe and reproducible. Preliminary results show good control of postoperative pain, shorter hospital stay and a trend toward fewer recurrences. A longer follow-up time is required to assess recurrence rates.
Conflict of InterestsThe authors declare that they have no conflict of interest.
Please cite this article as: Salido Fernandez S, Fraile Vilarrasa M, Osorio Silla I, Georgiev Hristov T, Bernar de Oriol J, González-Ayora S, et al. Vía totalmente extraperitoneal extendida (eTEP) para la corrección de hernias ventrales: resultados preliminares. Cir Esp. 2020;98:260–266.