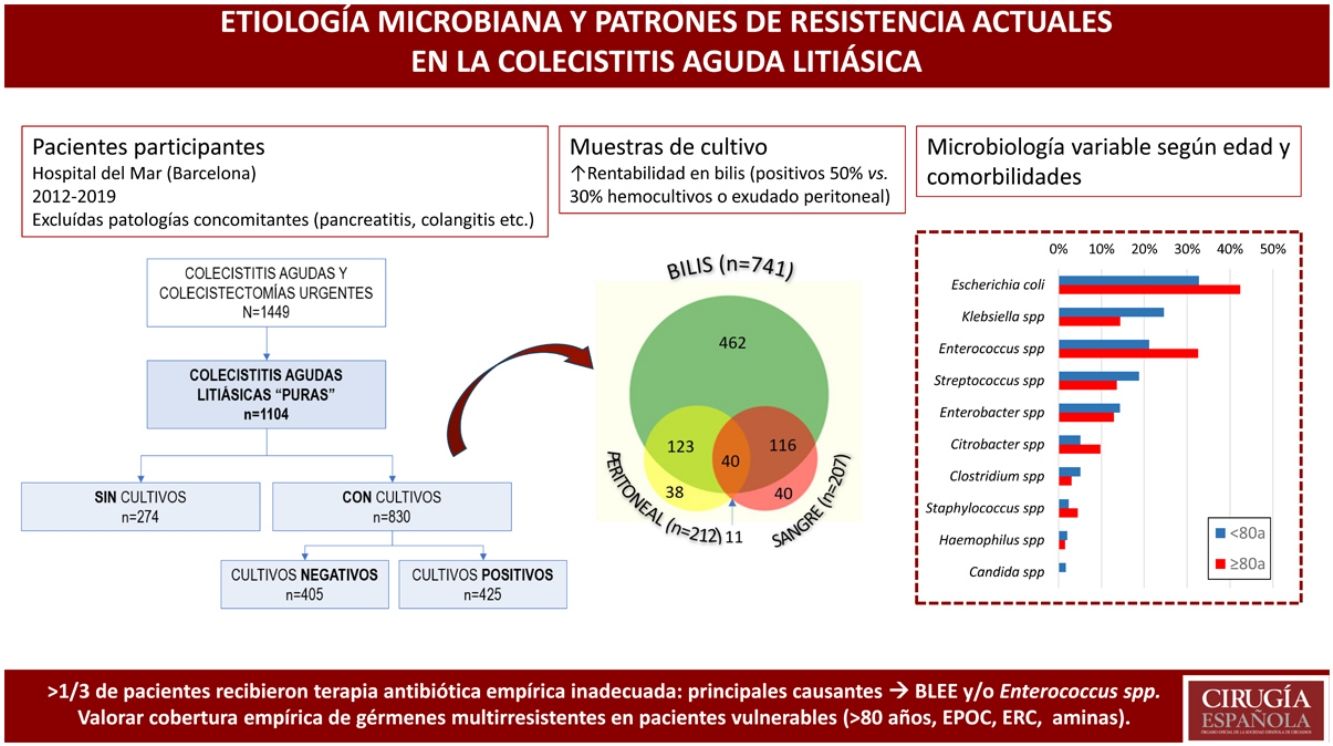
The current treatment for acute calculous cholecystitis (ACC) is early laparoscopic cholecystectomy, in association with appropriate empiric antibiotic therapy. In our country, the evolution of the prevalence of the germs involved and their resistance patterns have been scarcely described. The aim of the study was to analyze the bacterial etiology and the antibiotic resistance patterns in ACC.
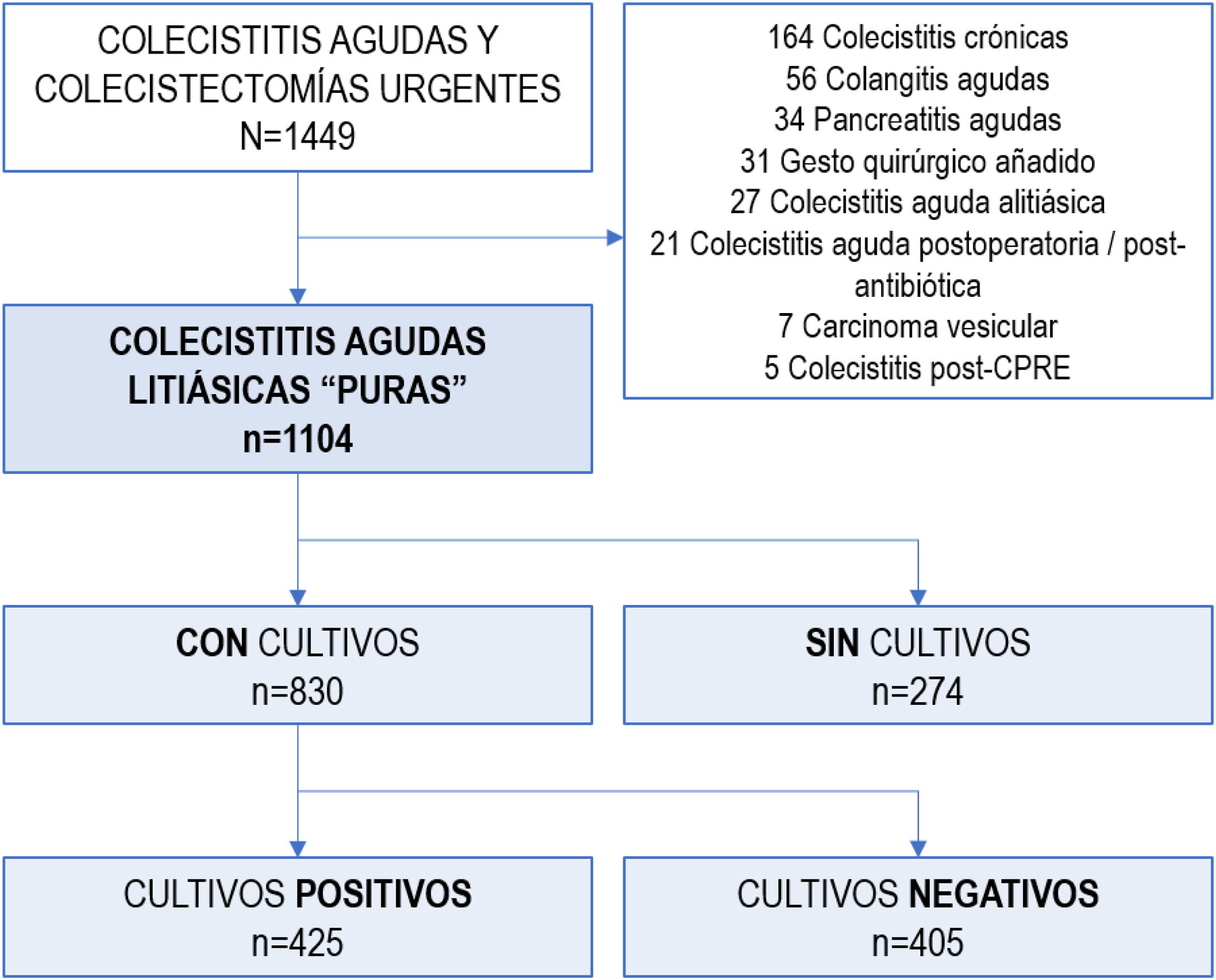
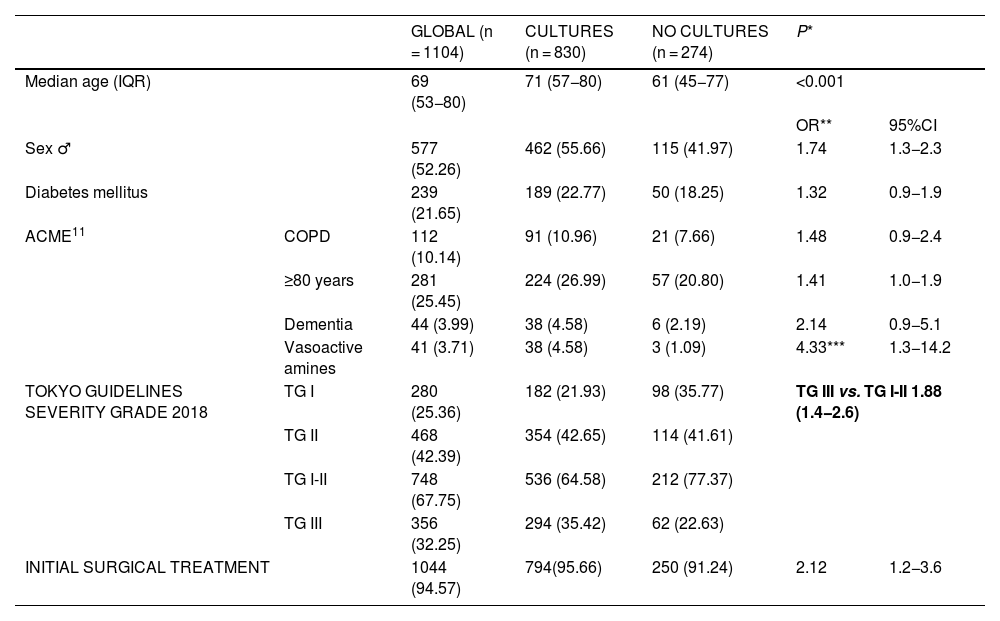
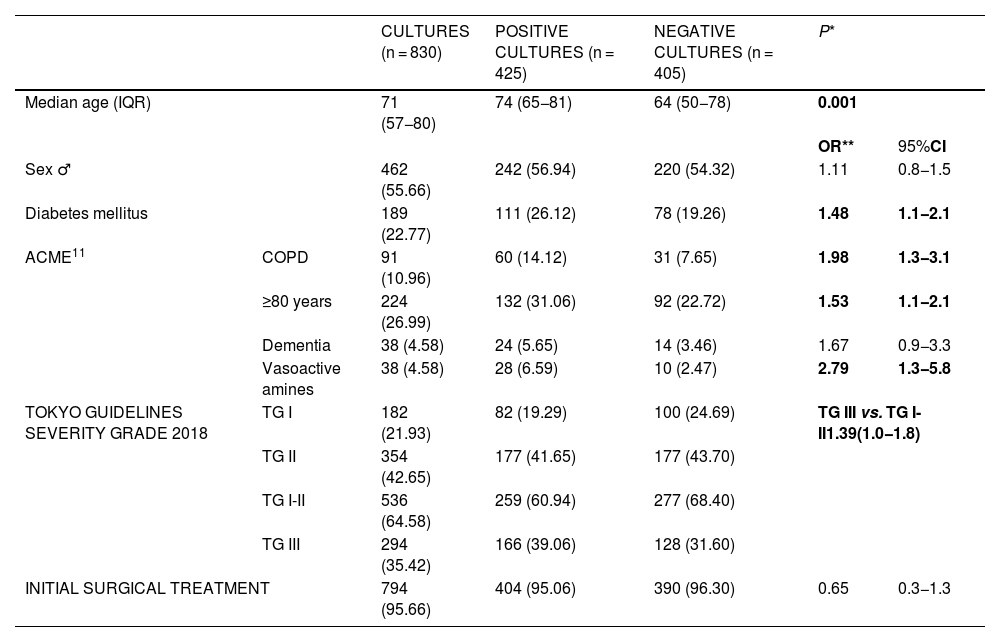
MethodsWe conducted a single-center, retrospective, observational study of consecutive patients diagnosed with ACC between 01/2012 and 09/2019. Patients with a concomitant diagnosis of pancreatitis, cholangitis, postoperative cholecystitis, histology of chronic cholecystitis or carcinoma were excluded. Demographic, clinical, therapeutic and microbiological variables were collected, including preoperative blood cultures, bile and peritoneal fluid cultures.
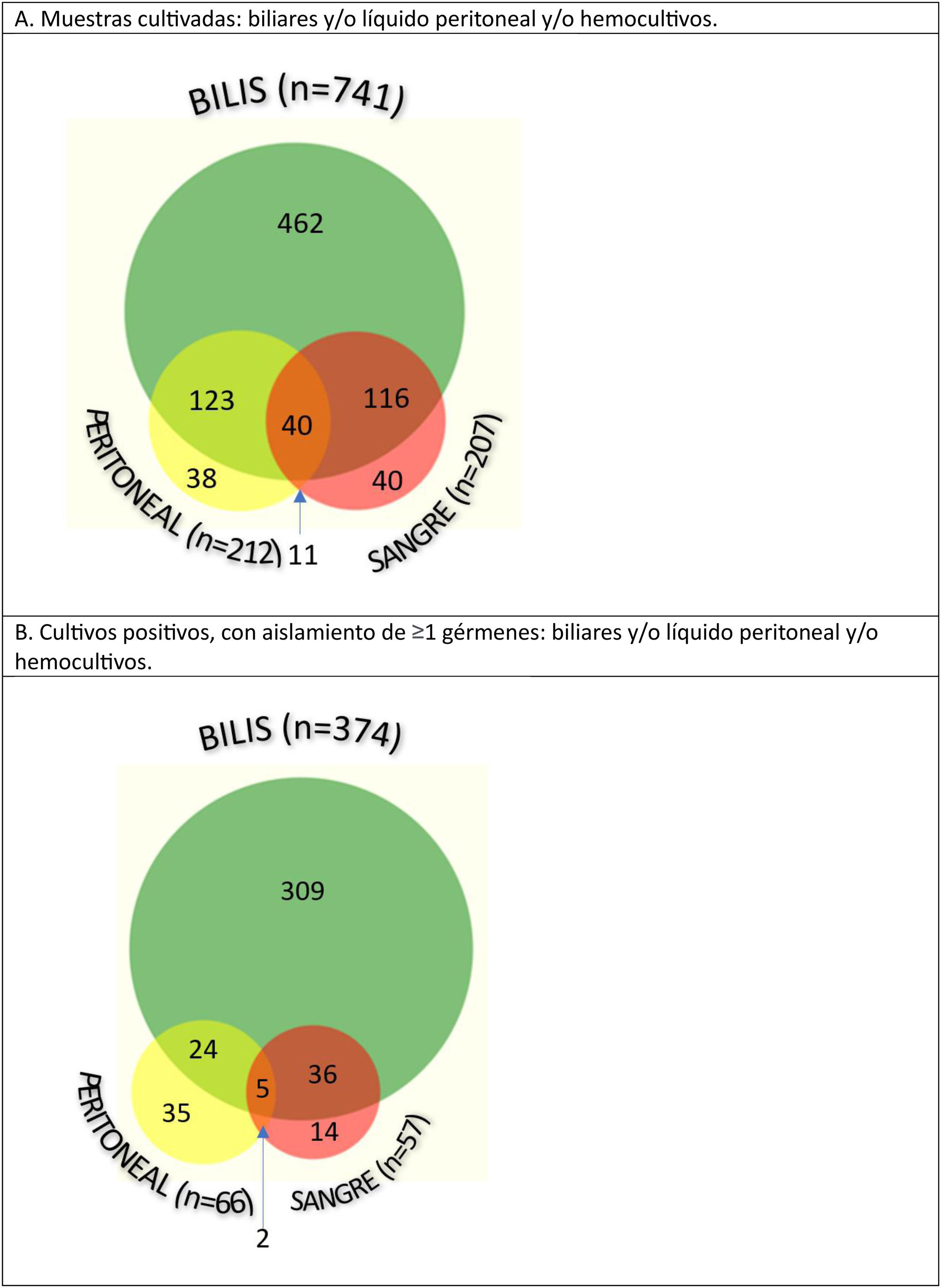
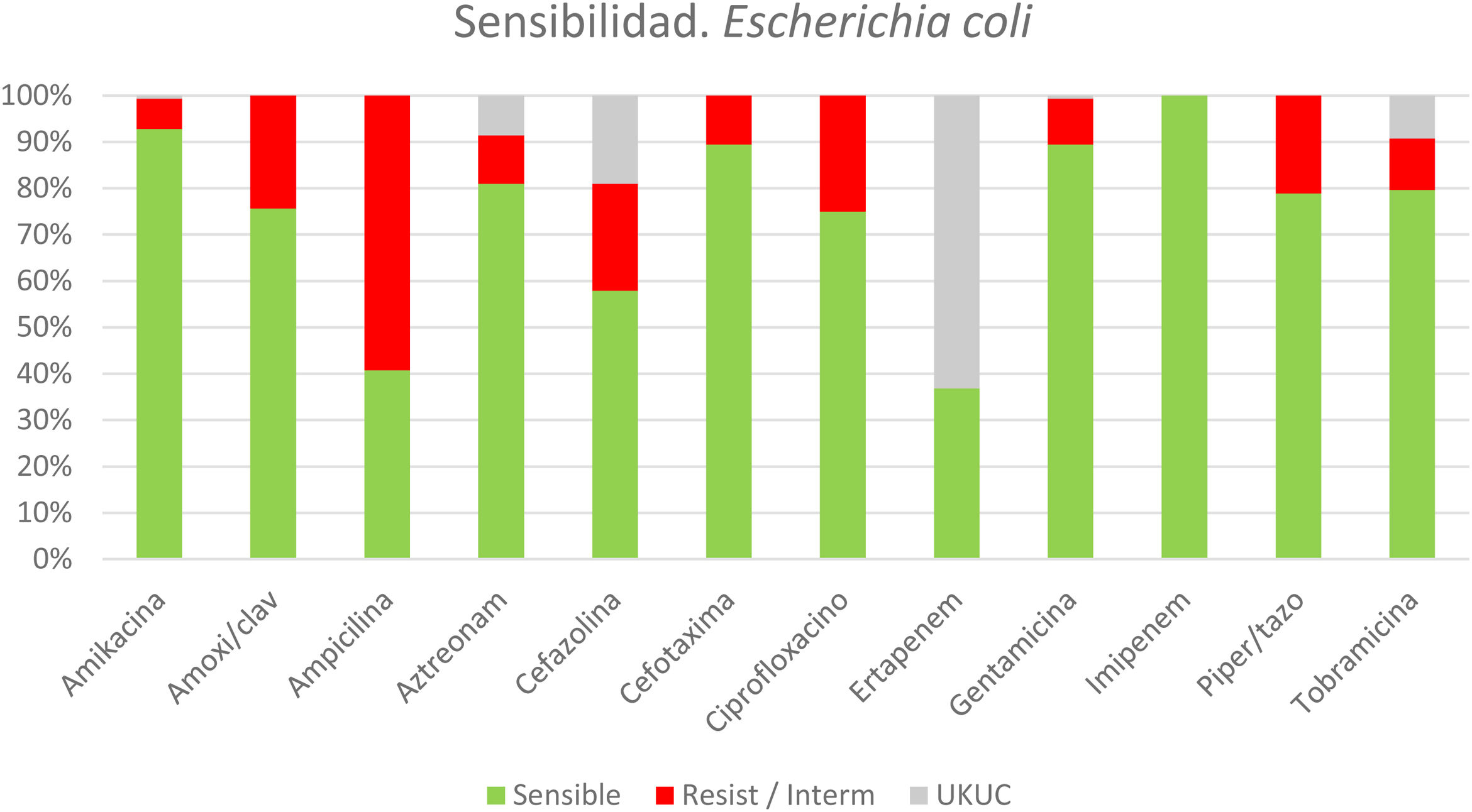
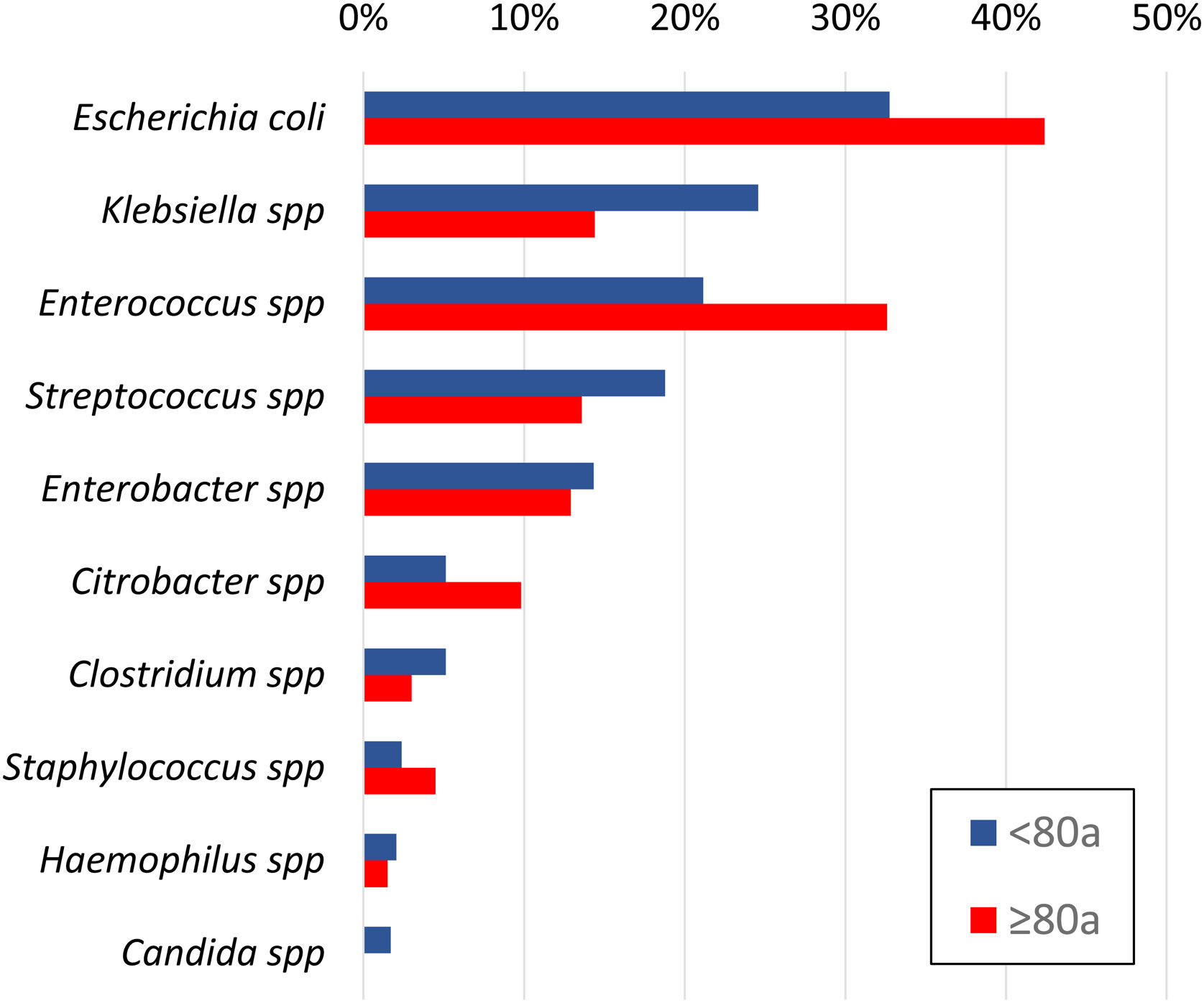
ResultsA total of 1104 ACC were identified, and samples were taken from 830 patients: bile in 89%, peritoneal fluid and/or blood cultures in 25%. Half of the bile cultures and less than one-third of the blood and/or peritoneum samples were positive. Escherichia coli (36%), Enterococcus spp (25%), Klebsiella spp (21%), Streptococcus spp (17%), Enterobacter spp (14%) and Citrobacter spp (7%) were isolated. Anaerobes were identified in 7% of patients and Candida spp in 1%. Nearly 37% of patients received inadequate empirical antibiotic therapy. Resistance patterns were scrutinized for each bacterial species. The main causes of inappropriateness were extended-spectrum beta-lactamase–producing bacteria (34%) and Enterococcus spp (45%), especially in patients older than 80 years.
ConclusionsUpdated knowledge of microbiology and resistance patterns in our setting is essential to readjust empirical antibiotic therapy and ACC treatment protocols.
El tratamiento actual de la colecistitis aguda litiásica (CAL) es la colecistectomía laparoscópica precoz, asociada a una antibioticoterapia empírica apropiada. La prevalencia de los gérmenes causantes y sus resistencias han sido poco descritas en nuestro medio. El objetivo del estudio fue analizar la etiología bacteriana y sus patrones de resistencia antibiótica en CAL.
MétodosEstudio observacional unicéntrico, retrospectivo, de pacientes consecutivos diagnosticados de CAL en 01/2012-09/2019. Se excluyeron los pacientes con diagnóstico concomitante de pancreatitis, colangitis, colecistitis postoperatoria, estudio anatomopatológico de colecistitis crónica o carcinoma. Se recogieron variables demográficas, analíticas, terapéuticas y microbiológicas, incluyendo hemocultivos preoperatorios, cultivos biliares y de exudado peritoneal.
ResultadosDe un total de 1104 CAL, se tomaron muestras en 830 pacientes: biliares en 89%, de líquido peritoneal y/o hemocultivos en 25%. La mitad de los cultivos biliares y menos de un tercio en sangre y/o peritoneo resultaron positivos. Se aislaron E.coli (36%), Enterococcus spp. (25%), Klebsiella spp. (21%), Streptococcus spp. (17%), Enterobacter spp. (14%) y Citrobacter spp. (7%). Se identificaron anaerobios en el 7% y Candida spp. en 1%. El 37% de los pacientes recibieron una antibioticoterapia empírica inadecuada. Se analizaron detalladamente los patrones de resistencia para cada especie bacteriana. Las bacterias productoras de beta-lactamasas de espectro extendido (34%) y Enterococcus spp. (45%) fueron las principales causantes de la inadecuación, especialmente en pacientes >80 años.
ConclusionesEl conocimiento actualizado de la microbiología y patrones de resistencia en nuestro medio resulta fundamental para reajustar la antibioticoterapia empírica y los protocolos de tratamiento de la CAL.