The SARS-CoV-2 pandemic has a great impact worldwide, being Spain one of the most affected countries. The delay in bariatric surgery can have fatal consequences since up to 50% of the patients who are on the waiting list develop a new comorbidity during the time they remain on it and 1.5% of patients die while waiting for the intervention. That is why bariatric surgery should not be delayed, if the occupation of the hospital by COVID-19+ patients decreases significantly, and sufficient resources and safety are available to restart surgery in patients with benign pathology. This document contains the main recommendations for the bariatric surgery programs in our country from the point of view of safety, bariatric patient preparation and follow up during the SARS-CoV-2 pandemia.
La pandemia SARS-CoV-2ha tenido un gran impacto en todo el mundo, siendo España uno de los países más afectados. La demora en la cirugía bariátrica puede tener consecuencias fatales, ya que hasta el 50% de los pacientes que se encuentran en lista de espera desarrollan una nueva comorbilidad durante el tiempo que permanecen en ella y el 1,5% de pacientes fallecen mientras esperan la intervención. Es por ello por lo que la cirugía bariátrica no debe demorarse en cuanto la ocupación del hospital por pacientes COVID-19+ disminuya de forma significativa y se disponga de recursos y seguridad suficiente para realizar la cirugía en pacientes con patología benigna. Este documento recoge las principales recomendaciones para los programas de cirugía bariátrica en nuestro país desde el punto de vista tanto de seguridad como de preparación y seguimiento del paciente bariátrico en el contexto de la pandemia SARS-CoV-2.
The SARS-CoV-2 pandemic of the first half of 2020 has had great impact around the world. Spain has been one of the hardest-hit countries, with a high number of infected people (more than 239,000 as of June 3) and also very high mortality (more than 27,000 deaths on the same date). The avalanche of patients with SARS-CoV-2 infection in emergency departments in early March and the emerging need for intensive care beds paralyzed operating rooms across the country. The incidence of cases has not been homogeneous in all regions, and some geographical areas have been much more affected than others.
The Spanish Association of Surgeons (AEC) has published a dynamic scale describing the different scenarios in which a hospital may find itself related to the percentage of hospitalization and ICU beds occupied by patients with SARS-CoV-2, as well as the hospital resources available.1 Once the health crisis was considered less serious, regions that were less affected by the pandemic progressively restarted elective surgery, starting with cancer patients and gradually including preferential benign pathologies.
Bariatric surgery was postponed in most of the country’s hospitals from the months of March to May. However, at this writing, there are already geographic regions where the necessary conditions exist to conduct it safely.
Despite the fact that the incidence of cases decreased after confinement and the health crisis seems to be more under control, there was still no effective treatment or vaccine that would allow the pandemic to be considered under control. Thus, it is necessary to maintain certain precautions to reduce the number of infections: it is still necessary to maintain social distancing and maximize hygiene measures. In this context, the restart of elective surgery requires careful planning and the introduction of new preventive measures that protect both patients and healthcare personnel.2 It will be necessary to maintain ‘clean’ or ‘COVID-19–free’ circuits within the hospital to provide maximum safety, carry out periodic controls of healthcare workers, identify possible cases early and avoid performing elective surgery in potentially infected patients, given that the development of SARS-CoV-2 respiratory symptoms in the postoperative period of major surgery have been shown to significantly increase mortality.3 For these reasons, several scientific societies, such as the Spanish Society for the Surgery of Obesity and Metabolic Diseases (SECO), the Spanish Association of Surgeons (AEC), the Spanish Society for the Study of Obesity (SEEDO), the Spanish Society of Endocrinology and Nutrition (SEEN) and the Spanish Scientific Society of Diet and Nutrition (SEDYN) have united to develop this document of recommendations for safe bariatric surgery in the context of the SARS-CoV-2 pandemic.
Morbidly obese patients are more vulnerable to infection with the COVID-19 virus than the rest of the population. Obesity has been a prognostic factor for the poor evolution of the infection.4,5 Furthermore, patients with severe obesity generally have multiple associated comorbidities, and this group is at a much higher risk of death due to the complications generated by SARS-CoV-2.6,7 It is known that bariatric surgery is a safe, effective treatment that is indicated in people with morbid obesity and type II obesity with associated serious comorbidities, such as type 2 diabetes mellitus (DM2), arterial hypertension (HTN) or obstructive sleep apnea (OSA).8,9 Therefore, bariatric surgery should be included in the structured waiting lists with the commitment of the autonomous communities to guarantee a delay of no more than 6 months, as is done with other benign surgical pathologies.10
Risks of delay in bariatric surgeryThe delay in bariatric surgery can have fatal consequences: up to 50% of patients develop a new comorbidity while on the waiting list, and 1.5% of patients die while waiting for surgery.11 This is why bariatric surgery should be restarted as soon as possible after the hospital occupancy of COVID-19+ patients decreases significantly, and sufficient resources and safety are available to restart surgery in patients with benign pathology.12
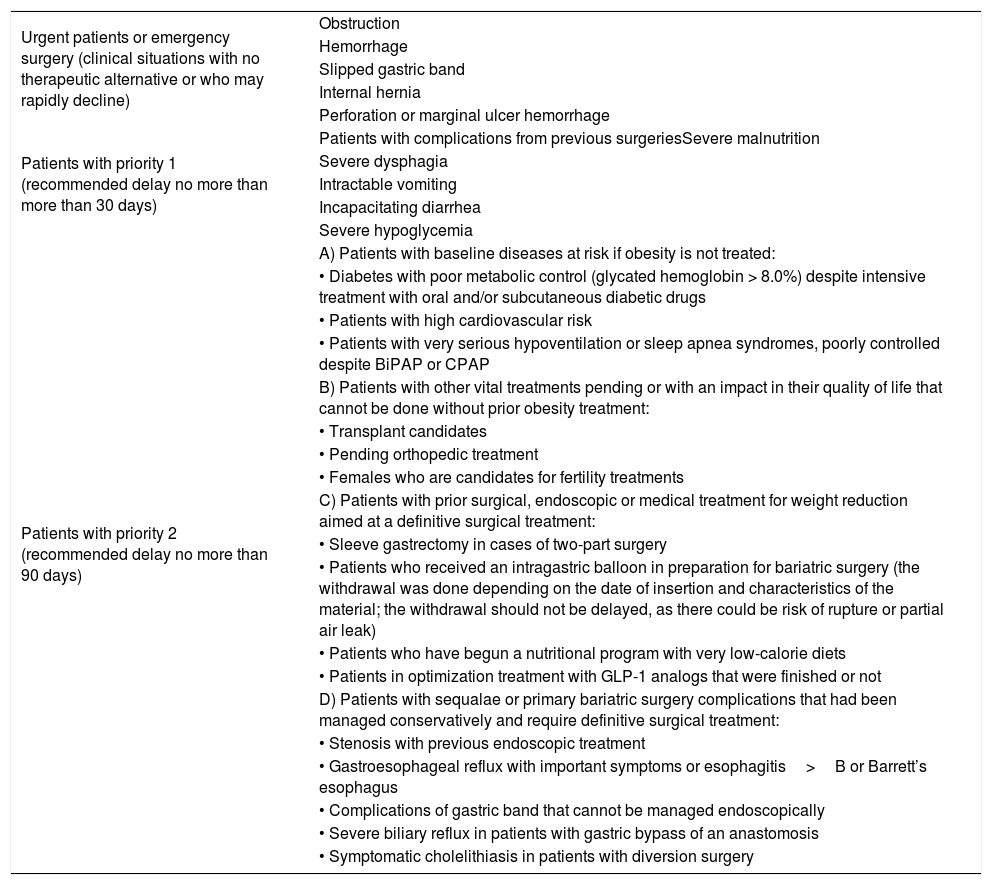
Selection of patients for the restart of bariatric surgeryThe prioritization of patients will depend on the baseline status of each patient and their associated diseases.13–15 Patients will be classified into 4 groups, whose characteristics are shown in Table 1:
- 1
Urgent or emergent patients (clinical situations with no therapeutic alternative or who may deteriorate rapidly)
- 2
Priority 1 patients: recommended delay of no more than 30 days
- 3
Priority 2 patients: recommended delay of no more than 90 days
- 4
Elective patients: recommended delay of no more than 6–12 months
Prioritization of bariatric patients according to their baseline status, associated diseases, clinical situation and possible sequalae of delayed surgery.
| Urgent patients or emergency surgery (clinical situations with no therapeutic alternative or who may rapidly decline) | Obstruction |
| Hemorrhage | |
| Slipped gastric band | |
| Internal hernia | |
| Perforation or marginal ulcer hemorrhage | |
| Patients with priority 1 (recommended delay no more than more than 30 days) | Patients with complications from previous surgeriesSevere malnutrition |
| Severe dysphagia | |
| Intractable vomiting | |
| Incapacitating diarrhea | |
| Severe hypoglycemia | |
| Patients with priority 2 (recommended delay no more than 90 days) | A) Patients with baseline diseases at risk if obesity is not treated: |
| • Diabetes with poor metabolic control (glycated hemoglobin > 8.0%) despite intensive treatment with oral and/or subcutaneous diabetic drugs | |
| • Patients with high cardiovascular risk | |
| • Patients with very serious hypoventilation or sleep apnea syndromes, poorly controlled despite BiPAP or CPAP | |
| B) Patients with other vital treatments pending or with an impact in their quality of life that cannot be done without prior obesity treatment: | |
| • Transplant candidates | |
| • Pending orthopedic treatment | |
| • Females who are candidates for fertility treatments | |
| C) Patients with prior surgical, endoscopic or medical treatment for weight reduction aimed at a definitive surgical treatment: | |
| • Sleeve gastrectomy in cases of two-part surgery | |
| • Patients who received an intragastric balloon in preparation for bariatric surgery (the withdrawal was done depending on the date of insertion and characteristics of the material; the withdrawal should not be delayed, as there could be risk of rupture or partial air leak) | |
| • Patients who have begun a nutritional program with very low-calorie diets | |
| • Patients in optimization treatment with GLP-1 analogs that were finished or not | |
| D) Patients with sequalae or primary bariatric surgery complications that had been managed conservatively and require definitive surgical treatment: | |
| • Stenosis with previous endoscopic treatment | |
| • Gastroesophageal reflux with important symptoms or esophagitis>B or Barrett’s esophagus | |
| • Complications of gastric band that cannot be managed endoscopically | |
| • Severe biliary reflux in patients with gastric bypass of an anastomosis | |
| • Symptomatic cholelithiasis in patients with diversion surgery |
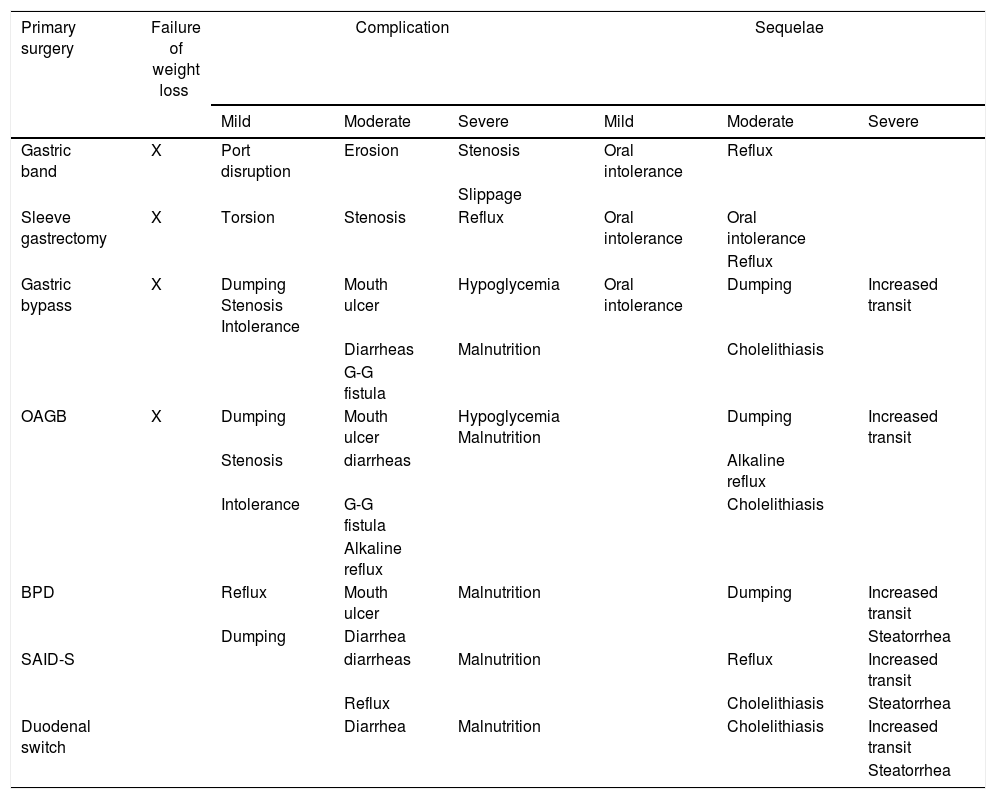
Revision surgery includes a wide range of possibilities, from treating complications to managing the failure of weight loss after a primary procedure. With all this, situations can vary widely from patients who have simply regained weight, to circumstances with serious or life-threatening symptoms. The latter should be prioritized. The main causes of revision surgery after primary bariatric surgeries currently accepted by the international community are summarized in Table 2.
Main indications for revision surgery after primary bariatric surgery currently accepted by the international community.
| Primary surgery | Failure of weight loss | Complication | Sequelae | ||||
|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | Mild | Moderate | Severe | ||
| Gastric band | X | Port disruption | Erosion | Stenosis | Oral intolerance | Reflux | |
| Slippage | |||||||
| Sleeve gastrectomy | X | Torsion | Stenosis | Reflux | Oral intolerance | Oral intolerance | |
| Reflux | |||||||
| Gastric bypass | X | Dumping Stenosis Intolerance | Mouth ulcer | Hypoglycemia | Oral intolerance | Dumping | Increased transit |
| Diarrheas | Malnutrition | Cholelithiasis | |||||
| G-G fistula | |||||||
| OAGB | X | Dumping | Mouth ulcer | Hypoglycemia Malnutrition | Dumping | Increased transit | |
| Stenosis | diarrheas | Alkaline reflux | |||||
| Intolerance | G-G fistula | Cholelithiasis | |||||
| Alkaline reflux | |||||||
| BPD | Reflux | Mouth ulcer | Malnutrition | Dumping | Increased transit | ||
| Dumping | Diarrhea | Steatorrhea | |||||
| SAID-S | diarrheas | Malnutrition | Reflux | Increased transit | |||
| Reflux | Cholelithiasis | Steatorrhea | |||||
| Duodenal switch | Diarrhea | Malnutrition | Cholelithiasis | Increased transit | |||
| Steatorrhea | |||||||
OAGB: one-anastomosis gastric bypass; BPD: biliopancreatic diversion.
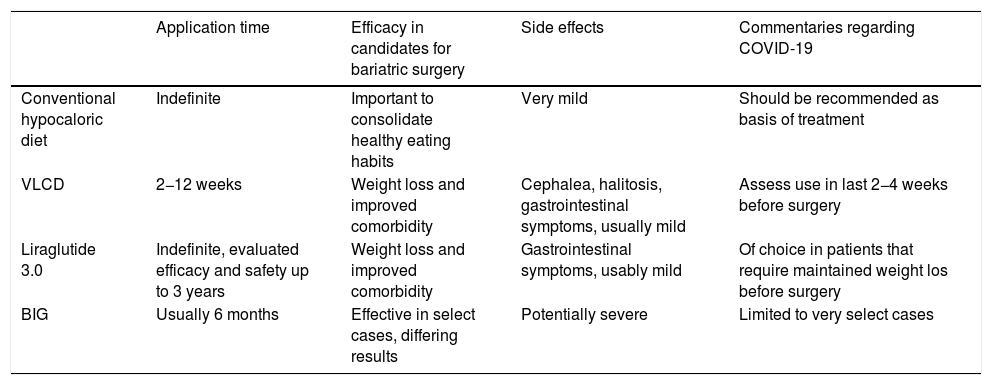
The evaluation and preparation of patients for bariatric surgery have not been substantially modified due to the current situation, except for patient screening for possible SARS-CoV-2 infection.1,16 It is important to consider that elevated stress levels secondary to the COVID-19 pandemic can exacerbate emotional symptoms,17 which increases impulsivity and could trigger binge episodes before and after bariatric surgery. When preparing the patient for bariatric surgery, it is essential to achieve adequate control of secondary or obesity-related diseases, such as DM2, HTN or OSA, which may have been affected by the effect of confinement and the COVID-19 epidemic on clinical care.18 In the case of DM2 treatment, drugs that have a beneficial effect on body weight are preferred, such as GLP-1 analogs or SLGT-2 inhibitors.19 Weight loss prior to the intervention is very important,20 and in the COVID-19 era there may be some changes in the usual recommendations that are summarized in Table 3 and in the following points:
- •
A conventional hypocaloric diet should be recommended as the basis of treatment.
- •
Assess the use of very low-calorie diets in the last 2−4 weeks before surgery.21
- •
Liraglutide 3.0 may be of choice in patients who require sustained weight loss prior to surgery.22
- •
The intragastric balloon should be limited to highly selected cases in accordance with the possible restrictions on endoscopic procedures depending on the phases of the SARS-CoV-2 pandemic.
Summary of recommendations for preoperative weight loss in bariatric patients in the context of the SARS-CoV-2 pandemic.
| Application time | Efficacy in candidates for bariatric surgery | Side effects | Commentaries regarding COVID-19 | |
|---|---|---|---|---|
| Conventional hypocaloric diet | Indefinite | Important to consolidate healthy eating habits | Very mild | Should be recommended as basis of treatment |
| VLCD | 2−12 weeks | Weight loss and improved comorbidity | Cephalea, halitosis, gastrointestinal symptoms, usually mild | Assess use in last 2−4 weeks before surgery |
| Liraglutide 3.0 | Indefinite, evaluated efficacy and safety up to 3 years | Weight loss and improved comorbidity | Gastrointestinal symptoms, usably mild | Of choice in patients that require maintained weight los before surgery |
| BIG | Usually 6 months | Effective in select cases, differing results | Potentially severe | Limited to very select cases |
BIG: intragastric balloon; VLCD: very low-calorie diet.
Weight loss prior to bariatric surgery is especially recommended in all patients, but in times of the SARS-CoV-2 pandemic it is especially important in:
- •
Patients with BMI>50kg/m2
- •
Patients with serious obesity complications (poorly controlled DM2, severe OSA or poor tolerance to CPAP, disabling arthropathy, non-alcoholic steatohepatitis and hepatomegaly)
- •
Patients with cardiovascular diseases (poorly controlled HTN, ischemic heart disease, atrial fibrillation, heart failure)
- •
Patients with chronic kidney disease (grades 3–4)
- •
Patients awaiting other treatments (candidates for transplantation or orthopedic surgery)
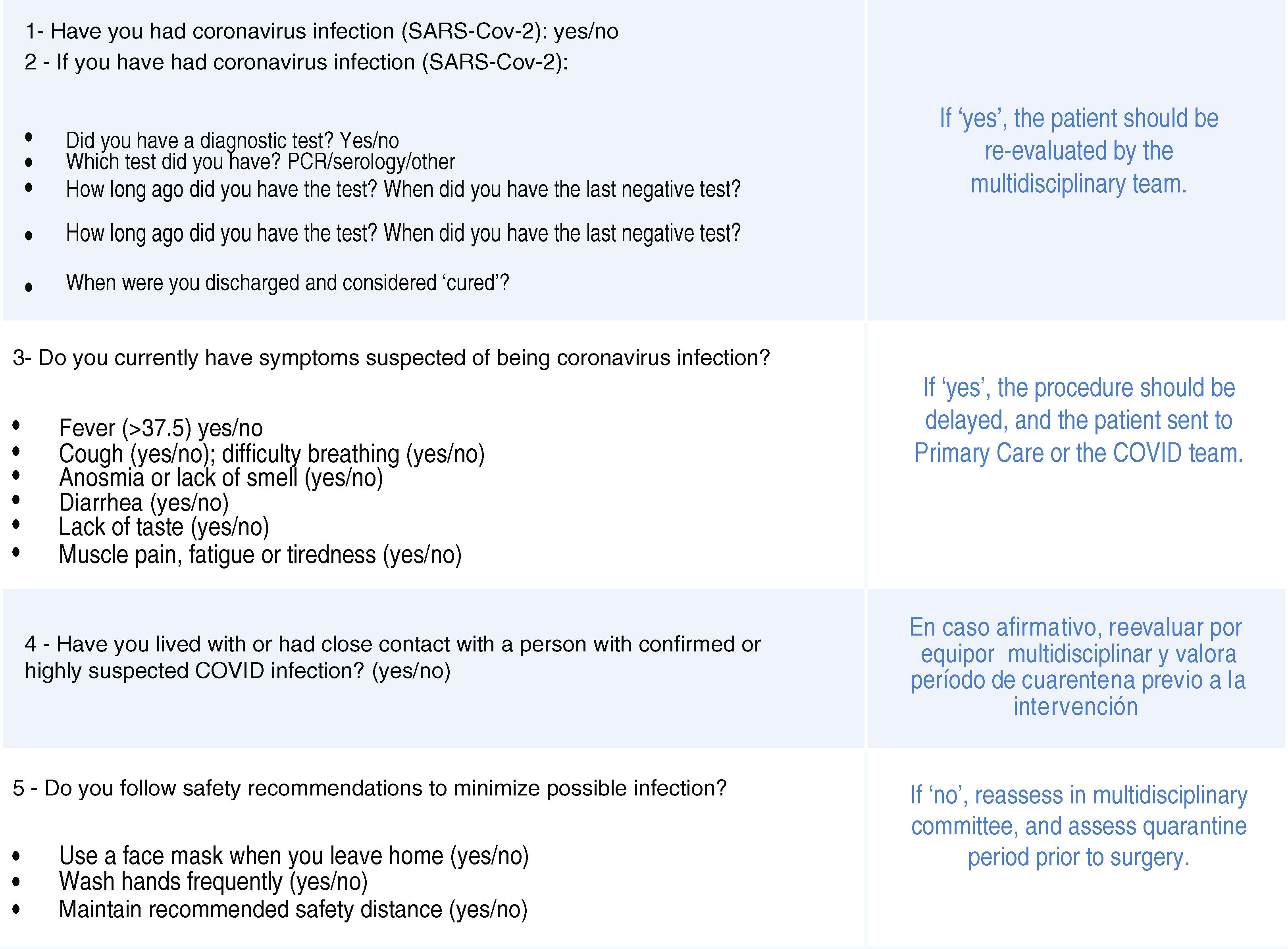
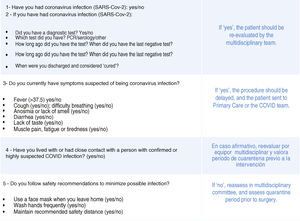
In the event of any symptom that is suspicious of SARS-CoV-2 infection, the healthcare professional must withdraw from the healthcare activity, notify their superiors and proceed according to the protocol established in their hospital so that symptoms are assessed and PCR, serologies or other appropriate tests are done. Early surgical scheduling 15 days in advance is recommended to be able to perform clinical and epidemiological screening 14 days before surgery, a PCR 48−72h before and another clinical/epidemiological screening test in the 24−48h prior to surgery. If suspicion of SARS-CoV-2 infection is ruled out, the process is continued, and surgical intervention is performed. The recommended questionnaire for the clinical and epidemiological screening of SARS-CoV-2 in the bariatric patient is shown in Fig. 1. In the event that a questionnaire response is positive, or the PCR is positive and there is suspected SARS-CoV-2 infection, it is recommended to delay the intervention and reevaluate the patient by the multidisciplinary team with the collaboration of the COVID team or the preventive medicine service, following the hospital action protocol for suspected cases. In areas with a very low incidence of SARS-CoV-2, performing PCR may not be necessary as long as there is no community transmission of the infection and the cases and their contacts are closely controlled in that area. The symptom and epidemiological questionnaire should be maintained until there is a vaccine or effective treatment for the SARS-CoV-2 pandemic, regardless of the incidence of cases in the area.
COVID-19–free surgical circuitTo safely perform bariatric surgery, the existence of a clean ‘COVID-free’ circuit must be ensured in the different areas: emergency rooms, hospitalization, consultations, operating rooms, and recovery rooms.1 It is important to screen for symptoms daily in hospitalized patients in order to detect possible cases early on. If a case is detected, the patient should be quickly isolated and reported to the COVID team or preventive medicine (depending on the internal protocol of the hospital) to establish the appropriate measures and the surveillance of possible contacts. In hospitalization rooms and the surgical area, preventive measures should be maintained for healthcare personnel and patient companions: frequent hand washing, masks, maintaining a safe distance (also in waiting rooms and common areas), minimizing personal items and storing them in a closed bag. It is recommended to limit the number of family members accompanying the patient (preferably one, under the age of 70).23 Hospital stay should be minimized, so multimodal rehabilitation or fast-track recovery programs (ERAS) will be of great use.24 It should be noted that with current measures it is not possible to ensure a zero risk of contagion for healthcare personnel. It is advisable to keep the personnel in the operating room to the absolute minimum, especially during orotracheal intubation and extubation at the end of the procedure.25 Extreme caution should also be exercised with aerosols and surgical smoke, which have been shown to transmit other viruses and could also transmit SARS-CoV-2.26,27
Recommendations for patient follow-upThe clinical follow-up protocol after bariatric surgery will be similar to the usual protocol,28 but it should be adapted to the circumstances of each hospital regarding the COVID-19 pandemic and reduce face-to-face visits to the absolute minimum.29 It is especially important to carry out a coordinated follow-up plan agreed upon with the patient that favors remote care and ensures adequate accessibility to the clinical team if necessary.30 In this context, the participation of primary care in this process will facilitate patient follow-up. Telematic clinical care, either individual or in a group, must follow well-defined guidelines at each hospital and ensure that basic issues related to identification, confidentiality, information registration, patient safety and adequate legal coverage are met.31,32 Specific clinical protocols must be established to identify situations that require face-to-face consultation in order to complete the evaluation or detect a possible complication.33 Our ultimate goal is for the patient to maintain confidence in the therapeutic team at all times. For this, it is necessary to emphasize that emergency surgical or medical support will be available at all times in case assistance is required for possible postoperative complications. It is also necessary to know the opinion and degree of satisfaction of the patients and the impact of this type of clinical care on the development and results of the care process.
Final thoughtsObesity is a pandemic that has multiple associated diseases. The chances of survival of obese patients are reduced, and they are much more vulnerable to complications generated by SARS-CoV-2. The SARS-CoV-2 pandemic has caused many surgical interventions to be delayed, and this delay, in the case of bariatric surgery, can have serious consequences for people who are obese and are on the waiting list, as half will develop new comorbidities and 1.5% may die while waiting for surgery. For this reason, it is essential not to delay bariatric surgery. As soon as the resources and sufficient safety measures are available, surgery should be restarted in patients with benign pathology. Prioritization criteria should be taken into consideration the baseline status and associated diseases of patients on the bariatric surgery waiting list. When preparing patients for surgery, preoperative weight loss should be emphasized, and screening for SARS-CoV-2 infection should be done. To perform bariatric surgery safely, the existence of a clean, COVID-free circuit must be ensured in the different areas: emergency rooms, hospitalization, outpatient consultations, operating rooms, and recovery rooms. It is recommended to minimize hospital stay by relying on ERAS programs and limiting visitors. The follow-up protocol after bariatric surgery should be adapted to the epidemiological circumstances of each hospital regarding the SARS-CoV-2 pandemic. The analysis of this year’s caseload will be necessary to compare the results with the quality indicators of official societies.34
Conflicts of interestThe authors have no conflict of interests to declare.
Please cite this article as: Sánchez Santos R, Garcia Ruiz de Gordejuela A, Breton Lesmes I, Lecube Torelló A, Moizé Arcone V, Arroyo Martin JJ, et al. Obesidad y SARS-CoV-2: consideraciones sobre la cirugía bariátrica y recomendaciones para el inicio de la actividad quirúrgica. Cir Esp. 2021;99:4–10.