Preoperative progressive pneumoperitoneum and botulinum toxin type A are useful tools in the preparation of patients with loss of domain hernias. Both procedures are complementary in the surgical repair, especially with the use of prosthetic techniques without tension, that allow a integral management of these patients.
The aim of this paper is to update concepts related to both procedures, emphasizing the advantages that take place in the preoperative management of loss of domain hernias.
El neumoperitoneo progresivo preoperatorio y la toxina botulínica tipo A son herramientas útiles en la preparación de los pacientes con hernias gigantes que han perdido el domicilio. Ambos procedimientos son armas complementarias del procedimiento quirúrgico, especialmente con el uso de técnicas protésicas sin tensión, que permiten el manejo integral de estos pacientes.
Este artículo tiene por objeto actualizar conceptos relacionados con ambos procedimientos, incidiendo en las ventajas que aportan en el manejo preoperatorio de las hernias gigantes que han perdido el domicilio.
Preoperative progressive pneumoperitoneum (PPP) and type A botulinum toxin (BTX) are useful tools in the preoperative preparation of patients with giant loss of domain (LOD) hernias.1 Both procedures are complementary tools of the surgical procedure and facilitate the integral management of these patients.2
PPP is a technique that was described several decades ago. It has brought about a change in the surgical approach to LOD hernias, by making complete repair possible and reducing the number of complications, such as abdominal compartment syndrome and restrictive lung disease.3 Goñi-Moreno decided to use PPP to widen the abdominal cavity in patients with LOD hernias, and thereby be able to adequately reduce the herniary content.4 Although its use has not been extensively established in the majority of hospitals, specialized groups that have implemented PPP have reported good results with an acceptable risk rate.5–7
Despite its relatively recent incorporation, the BTX infiltration technique is a useful tool in the preoperative preparation of LOD hernias as it acts as a reversible chemical separation of components with minimal patient discomfort.8 Furthermore, it presents the advantage of continuing action in the late postoperative period, for approximately 6 months, in which the post-surgical abdomen adapts to these changes.9
The objective of this review is to describe the results published in the literature regarding the use of PPP and BTX in the preoperative preparation of LOD hernias.
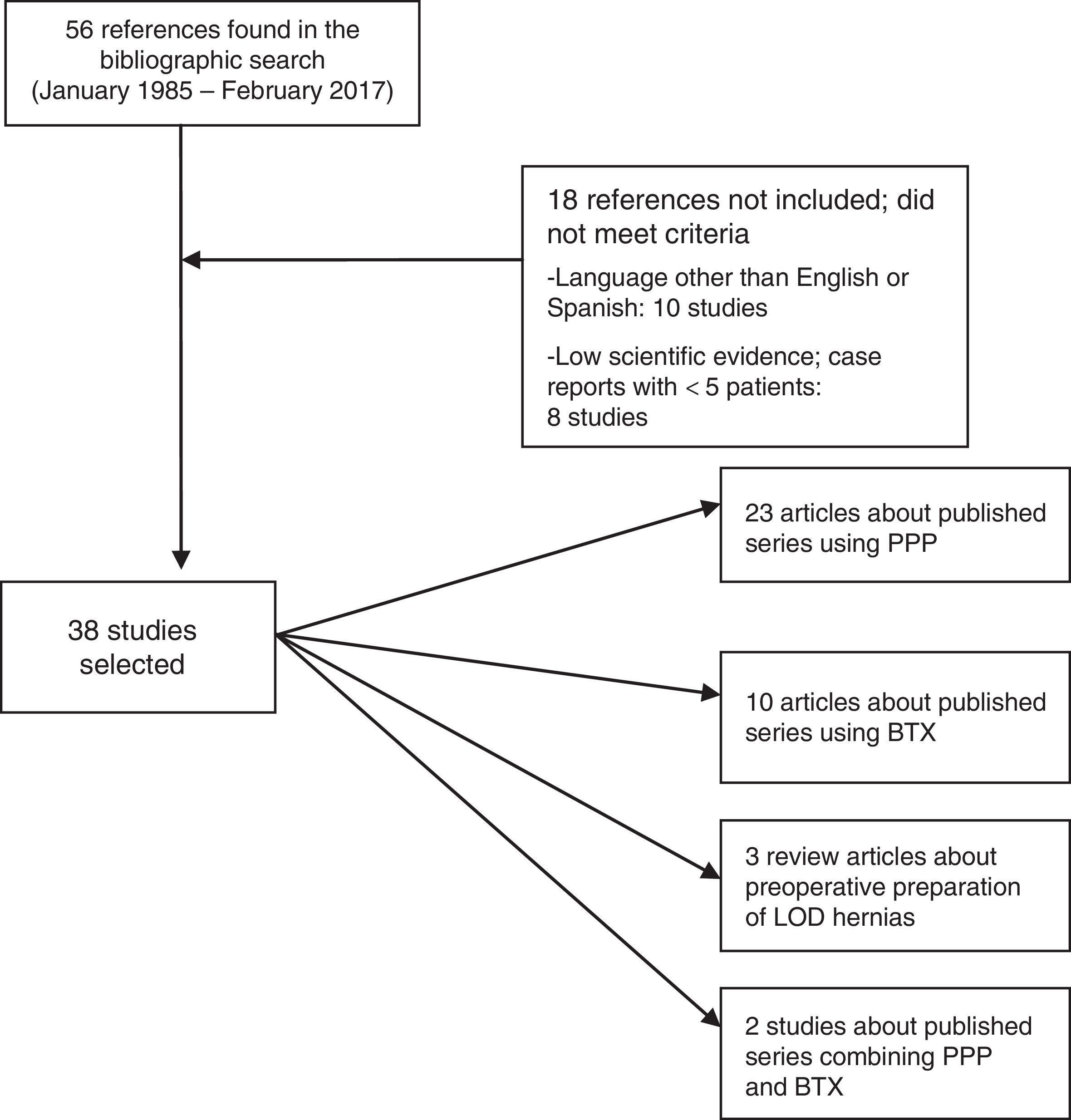
MethodsWe have carried out an electronic search with the Pubmed and Cochrane Library search engines (January 1985 to December 2016) of scientific articles (original and review articles) published in English and Spanish, with the keywords “progressive pneumoperitoneum”, “preoperative pneumoperitoneum”, “botulinum toxin”, “giant hernia”, “loss of domain hernia” and “large incisional hernia”. The bibliographic search followed the criteria of PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses).10 We have found 56 references in common with the different combinations of keywords. We ruled out 18 articles because they did not meet appropriate levels of evidence, were case reports with less than 5 cases, or were written in a language other than English or Spanish. In the end, we reviewed a total of 38 articles, assessed the abstracts of all the studies, and fully analyzed (with detailed reading of the entire article) 34 cases (Fig. 1).
Preoperative Progressive PneumoperitoneumThe objectives provided by the use of PPP include11:
- 1)
Progressive distension of the abdominal wall to be able to close the herniary defect with the least amount of tension possible during surgery.
- 2)
Stabilization of the form and function of the diaphragm, improving ventilatory function.
- 3)
Elongation of the muscles of the abdominal wall and the volume of the abdominal cavity.
- 4)
Pneumatic dissection of visceral bands and adhesions, which facilitates the reinsertion of intestinal loops into the abdominal cavity.
- 5)
Lastly, there are descriptions of peritoneal irritation and reactive local vasodilatation with increased macrophages the first days of the application, which improves healing capabilities.
Prior to considering the technique, an abdominal computed tomography (CT) scan, taken during the Valsalva maneuver if possible, is useful to evaluate the diameters and volumes of the abdomen and herniary sac as well as the characteristics of the lateral muscles and the rectus abdominis.12,13 Tanaka13 was the first author who provided an objective method for calculating these diameters and volumes based on CT findings. In fact, this author uses these measurements (hernia volume [VIH] and volume of the abdominal cavity [VAC]) to “radiologically” define LOD hernias. Thus, a VIH/VAC ratio higher than 20% is indicative of LOD hernia and would cause traumatic reinsertion into the cavity, with possible appearance of the complications described.14
The insufflation of air is done after the insertion of a catheter that facilitates the entire process until the surgical intervention. Different procedures have been described for catheter insertion throughout the evolution of the technique.15–19 Placement may be guided by ultrasound, which is most frequent, or by CT, which provides better control over localization.20 The technique is performed after the patient has fasted and is in the dorsal decubitus position. The point of puncture is determined according to the location of previous incisions and possible spaces without adhesions, preferably in the left hypochondrium. Certain workgroups, such as the Mayagoitia group,21 use a Veress needle similar to the laparoscopic procedure, a triple-lumen subclavian catheter left permanently in the cavity, and a 50mm syringe for insufflation with room air. Other groups use the puncture needle that comes with the central venous access kit (Cavafix®) and carry out the procedure similarly to vascular cannulation, but in the abdominal region.1,22
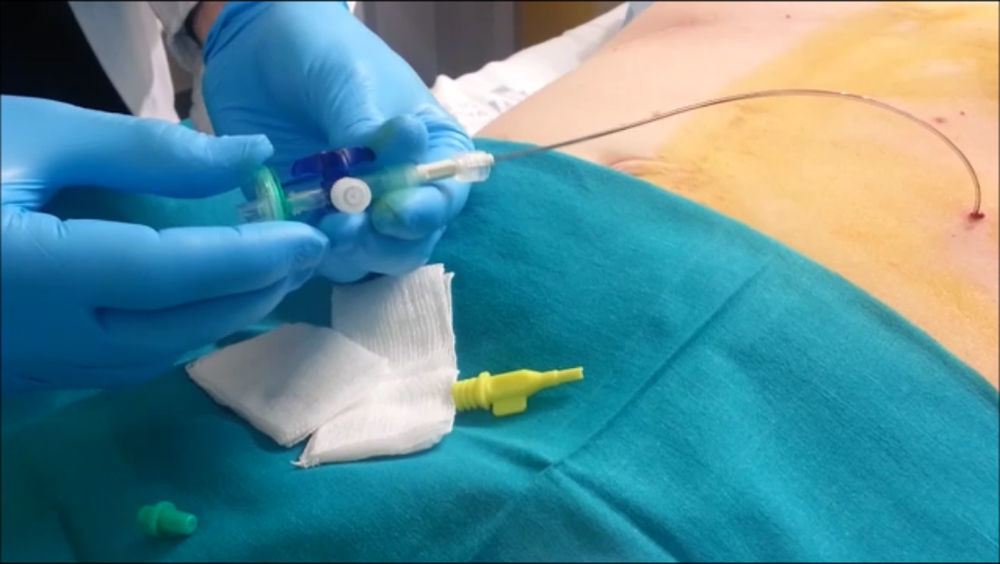
After having confirmed insertion within the abdominal cavity, a 3-way valve is placed in the distal lumen of the catheter along with an antibacterial filter (Fig. 2). In this manner, insufflation of the cavity is initiated with 200-300cc and the patient is sent to the radiology department to confirm the pneumoperitoneum.21 If the radiograph shows free air in both hemidiaphragms, the insufflation of air is completed according to the previously established protocol. Thus, daily rounds of 1000–1500cc can be introduced, according to patient tolerance.23,24 The most frequent event is pain radiating toward the scapula, which is usually temporary and does not require analgesia.25
An interesting aspect is the technique for monitoring intraabdominal pressure during insufflation. Although one author uses a sphygmograph connected to the other lumen of the catheter (the intraabdominal pressure should not exceed 15mmHg),23 in general, this verification is no longer used since experience indicates that it is very difficult to surpass 12mmHg without the patient presenting severe discomfort requiring the suspension of further insufflation. In other series,14,25 intraabdominal pressure monitoring is applied by using a laparoscopic pressure sensor.
Once the procedure has been completed, wide spectrum antibiotic therapy is indicated, as well as analgesia in case of pain and thromboembolic prophylaxis, with compression stockings and low-molecular-weight heparin. The patient can be discharged, although other groups recommend hospitalization for 24–48h to evaluate the initial tolerance to PPP.1,23,24 This daily administration can be done through home hospitalization or in the outpatient surgery setting.
Last of all, at the end of the process, an abdominal CT scan is usually done in order to calculate the VAC and the new VIH/VAC ratio, which will be able to predict the efficacy of the procedure prior to the surgical repair.1,14,22,25,26 One group also carried out new spirometry tests to measure lung capacity after insuflation.27
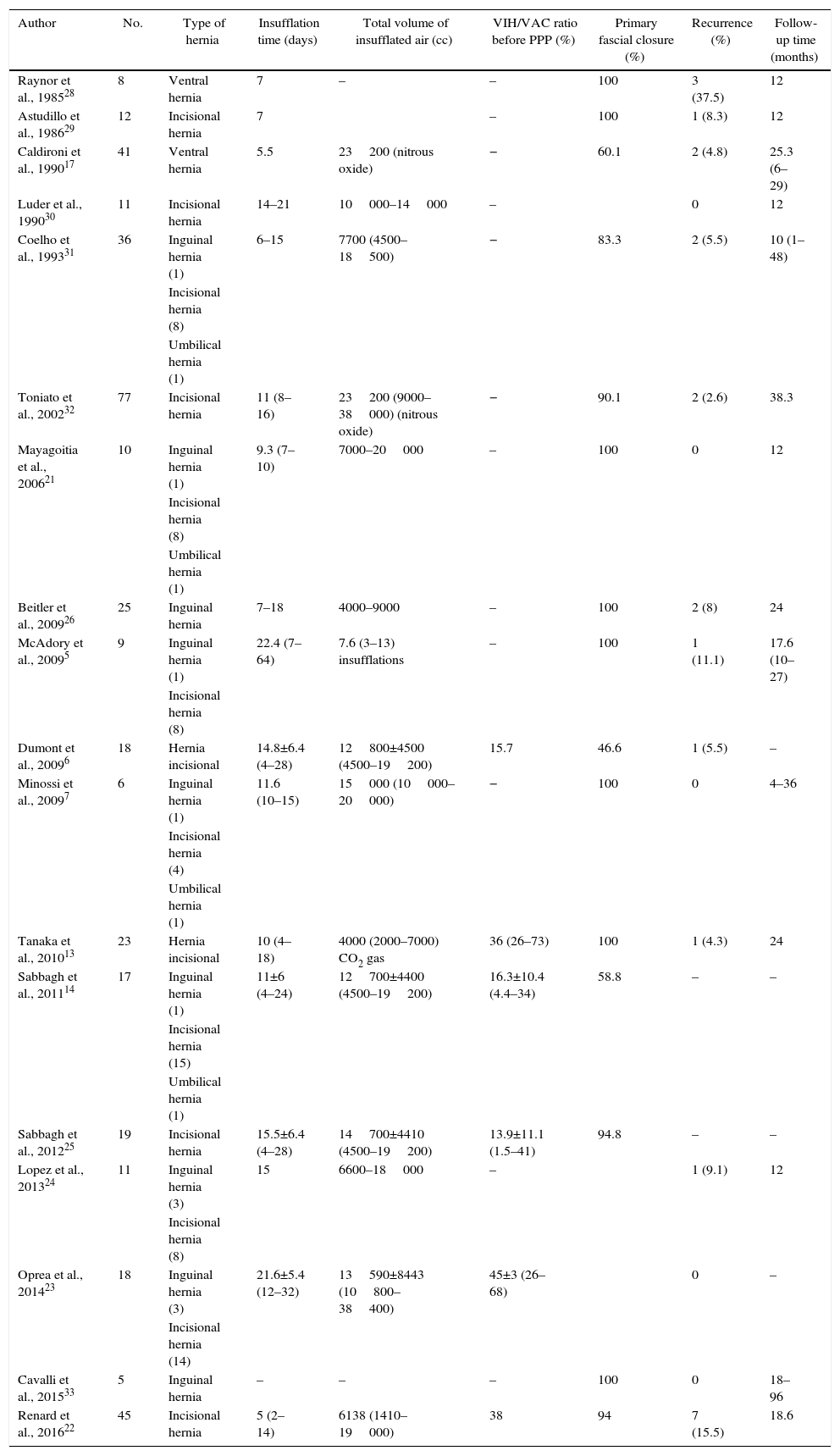
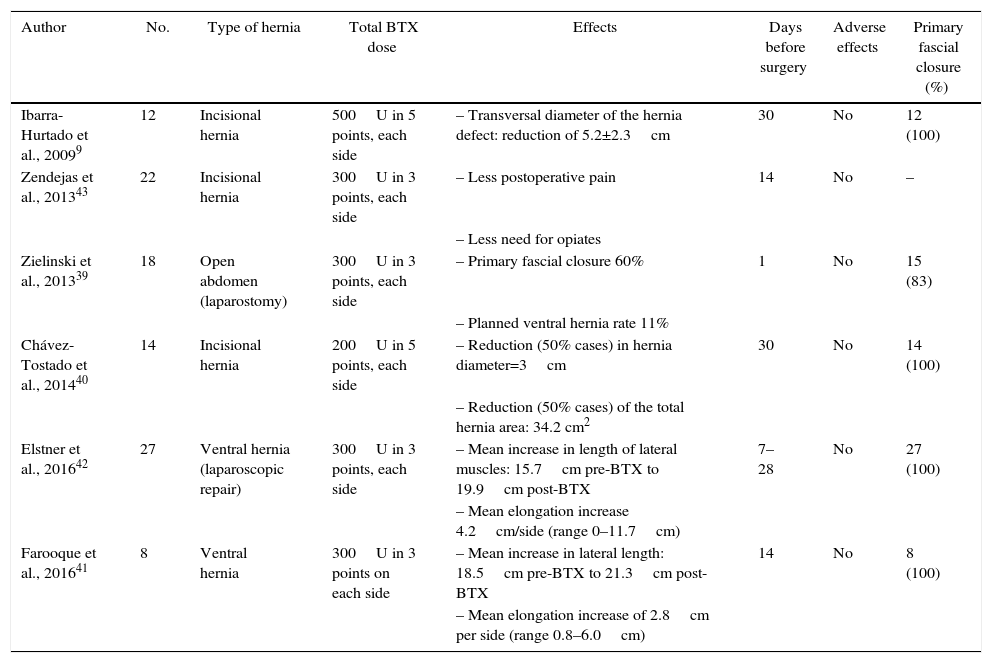
Table 1 lists the series published about the utilization of PPP and the results obtained.
Series Published About the Use of Preoperative Progressive Pneumoperitoneum in LOD Hernias (Studies Since 1985).
| Author | No. | Type of hernia | Insufflation time (days) | Total volume of insufflated air (cc) | VIH/VAC ratio before PPP (%) | Primary fascial closure (%) | Recurrence (%) | Follow-up time (months) |
|---|---|---|---|---|---|---|---|---|
| Raynor et al., 198528 | 8 | Ventral hernia | 7 | – | – | 100 | 3 (37.5) | 12 |
| Astudillo et al., 198629 | 12 | Incisional hernia | 7 | – | 100 | 1 (8.3) | 12 | |
| Caldironi et al., 199017 | 41 | Ventral hernia | 5.5 | 23200 (nitrous oxide) | − | 60.1 | 2 (4.8) | 25.3 (6–29) |
| Luder et al., 199030 | 11 | Incisional hernia | 14–21 | 10000–14000 | – | 0 | 12 | |
| Coelho et al., 199331 | 36 | Inguinal hernia (1) | 6–15 | 7700 (4500–18500) | − | 83.3 | 2 (5.5) | 10 (1–48) |
| Incisional hernia (8) | ||||||||
| Umbilical hernia (1) | ||||||||
| Toniato et al., 200232 | 77 | Incisional hernia | 11 (8–16) | 23200 (9000–38000) (nitrous oxide) | − | 90.1 | 2 (2.6) | 38.3 |
| Mayagoitia et al., 200621 | 10 | Inguinal hernia (1) | 9.3 (7–10) | 7000–20000 | – | 100 | 0 | 12 |
| Incisional hernia (8) | ||||||||
| Umbilical hernia (1) | ||||||||
| Beitler et al., 200926 | 25 | Inguinal hernia | 7–18 | 4000–9000 | – | 100 | 2 (8) | 24 |
| McAdory et al., 20095 | 9 | Inguinal hernia (1) | 22.4 (7–64) | 7.6 (3–13) insufflations | – | 100 | 1 (11.1) | 17.6 (10–27) |
| Incisional hernia (8) | ||||||||
| Dumont et al., 20096 | 18 | Hernia incisional | 14.8±6.4 (4–28) | 12800±4500 (4500–19200) | 15.7 | 46.6 | 1 (5.5) | – |
| Minossi et al., 20097 | 6 | Inguinal hernia (1) | 11.6 (10–15) | 15000 (10000–20000) | − | 100 | 0 | 4–36 |
| Incisional hernia (4) | ||||||||
| Umbilical hernia (1) | ||||||||
| Tanaka et al., 201013 | 23 | Hernia incisional | 10 (4–18) | 4000 (2000–7000) CO2 gas | 36 (26–73) | 100 | 1 (4.3) | 24 |
| Sabbagh et al., 201114 | 17 | Inguinal hernia (1) | 11±6 (4–24) | 12700±4400 (4500–19200) | 16.3±10.4 (4.4–34) | 58.8 | – | – |
| Incisional hernia (15) | ||||||||
| Umbilical hernia (1) | ||||||||
| Sabbagh et al., 201225 | 19 | Incisional hernia | 15.5±6.4 (4–28) | 14700±4410 (4500–19200) | 13.9±11.1 (1.5–41) | 94.8 | – | – |
| Lopez et al., 201324 | 11 | Inguinal hernia (3) | 15 | 6600–18000 | – | 1 (9.1) | 12 | |
| Incisional hernia (8) | ||||||||
| Oprea et al., 201423 | 18 | Inguinal hernia (3) | 21.6±5.4 (12–32) | 13590±8443 (10800–38400) | 45±3 (26–68) | 0 | – | |
| Incisional hernia (14) | ||||||||
| Cavalli et al., 201533 | 5 | Inguinal hernia | – | – | – | 100 | 0 | 18–96 |
| Renard et al., 201622 | 45 | Incisional hernia | 5 (2–14) | 6138 (1410–19000) | 38 | 94 | 7 (15.5) | 18.6 |
“Case reports” not included, only series with 5 or more patients.
There is no consensus in the literature about the quantity of air that should be insufflated in a PPP program, nor about how long it should be maintained.
Goñi-Moreno4 concludes the process when, by palpation, the abdominal flanks are observed to be prominent and tense. As other groups have reported, insufflation is stopped when excessive abdominal tension is observed.21,27 The main disadvantage of these arguments is that the calculation of the volume is not based on an objective factor and the that measurements are not completely reliable or reproducible, so it is only symptoms and signs of the patient treated with PPP that determine the volume insufflated.
Tanaka13 administers the volume equivalent to the VIH observed on preoperative CT scan and recommends the use of PPP when the VIH/VAC ratio is greater than 25%. Contrarily, Sabbagh24 utilizes the ratio between VIH and the total peritoneal content (PV), considering that PV is predictive of the closure of the fascia without tension in LOD hernias and represents a more specific measurement of the abdominal cavity volume. The VIH/PV ratio is indicative of the success of the primary facial closure without tension13: if the preoperative ratio is greater than 20%, the need for PPP can be anticipated before reconstruction of the abdominal wall. Lastly, Bueno-Lledó1 established the need to insufflate the VIH value 3 times due to uncontrolled losses during the procedure. Future studies are possibly needed to calculate the correct volume of insufflation of the PPP to predict fascial closure without tension, thereby avoiding the development of abdominal compartment syndrome.
The PPP insufflation time varies for each patient depending on the objective; according to the series studied, insufflation times range between 7 and 20 days.4,5,13–17,21 Thus, it is necessary to adjust the respiratory capacity throughout the duration of the procedure, confirming correct patient tolerance. Habitually, between 1000 and 1500 cc can be insufflated at each daily session until the patient feels mild abdominal pain or omalgia, which usually ceases spontaneously with mobilization.
Depending on the size of the defect, the final total volume is variable and generally ranges from 10 to 25L.23–37 Usually, the time that is established for maintaining the PPP ranges from 7 to 15 days in inguinal hernias and 11 to 30 days in ventral hernias.3,11 According to some groups, the most precise manner to know when to interrupt the PPP process and when a patient should be operated on is performing a CT scan after the procedure and re-calculating the VIH and VAC.1,13,14,25–27
Type A Botulinum ToxinThe first study that reported the benefits of BTX on the abdominal wall muscles was published by Cakmak.38 This author artificially induced compartment syndrome in rats and observed that BTX reduced abdominal wall tension and aided in tension-free closure of the fascial defect. Applied to the field of herniary diseases, the neurotoxin would act as a “chemical” separation of components, which causes relaxation of the lateral abdominal wall muscles.
In 2009, Ibarra-Hurtado9 published the first study about the use of BTX in 12 patients with ventral hernia. The author described the application technique for infiltrating BTX into the lateral muscles of the abdomen. Afterwards, Zielinski39 provided a retrospective review of his results with the administration of BTX in patients treated with open abdomen after damage control laparotomy; in all cases, negative pressure therapy was used for temporary abdominal closure until primary fascial closure was done. In 83% of these patients, complete early fascial closure without tension was achieved.
Ibarra and Chávez9,40 observed a significant decrease in the thickness and increased length of the lateral muscles of the abdominal wall after application of the neurotoxin. Farooque41 demonstrated a significant increase in the mean length of the lateral muscles of 2.8cm bilaterally. This degree of elongation of the abdominal wall is comparable with the separation of components, but does not alter the anatomical integrity of the abdominal wall, which preserves all the surgical options for repair.
Other groups use this technique in patients with LOD hernias who are candidates for assisted laparoscopic repair. Elstner42 applied BTX in 27 patients who underwent laparoscopic intraperitoneal repair, and the follow-up CT scans demonstrated a significant increase in the length of the lateral wall of 15.7 to 19.9cm after administration.
Similarly, Zendejas43 demonstrated that the preoperative administration of BTX before incisional hernia repair entails less need for opioid analgesia, although it does not influence other postoperative parameters, such as the appearance of complications, mean hospital stay, or recurrence.
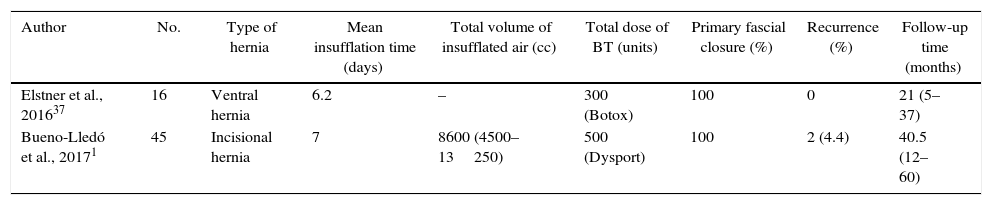
Table 2 shows the series published using preoperative BTX.
Series Published About the Use of Preoperative BTX in LOD Hernias.
| Author | No. | Type of hernia | Total BTX dose | Effects | Days before surgery | Adverse effects | Primary fascial closure (%) |
|---|---|---|---|---|---|---|---|
| Ibarra-Hurtado et al., 20099 | 12 | Incisional hernia | 500U in 5 points, each side | – Transversal diameter of the hernia defect: reduction of 5.2±2.3cm | 30 | No | 12 (100) |
| Zendejas et al., 201343 | 22 | Incisional hernia | 300U in 3 points, each side | – Less postoperative pain | 14 | No | – |
| – Less need for opiates | |||||||
| Zielinski et al., 201339 | 18 | Open abdomen (laparostomy) | 300U in 3 points, each side | – Primary fascial closure 60% | 1 | No | 15 (83) |
| – Planned ventral hernia rate 11% | |||||||
| Chávez-Tostado et al., 201440 | 14 | Incisional hernia | 200U in 5 points, each side | – Reduction (50% cases) in hernia diameter=3cm | 30 | No | 14 (100) |
| – Reduction (50% cases) of the total hernia area: 34.2 cm2 | |||||||
| Elstner et al., 201642 | 27 | Ventral hernia (laparoscopic repair) | 300U in 3 points, each side | – Mean increase in length of lateral muscles: 15.7cm pre-BTX to 19.9cm post-BTX | 7–28 | No | 27 (100) |
| – Mean elongation increase 4.2cm/side (range 0–11.7cm) | |||||||
| Farooque et al., 201641 | 8 | Ventral hernia | 300U in 3 points on each side | – Mean increase in lateral length: 18.5cm pre-BTX to 21.3cm post-BTX | 14 | No | 8 (100) |
| – Mean elongation increase of 2.8cm per side (range 0.8–6.0cm) |
The most widely used subtypes for medical application are types A and B BTX. The neurotoxin blocks the release of acetylcholine in the nerve endings and completely eliminates the electrical activity produced by the muscle contraction. The final effect is a temporary chemical denervation at the neuromuscular connection, with no physical injury to the nerve structures.44
The 2 commercial brands of type A BTX that are most widely used around the world are Botox® and Dysport®. The benefit of the neurotoxin is based on decreased lateral tension forces on the herniary defect and the elongation of the lateral muscles of the abdomen with a subsequent increase in the volume of the abdominal cavity, which provides for abdominal reconstruction without tension and an adequate period of protection.8 Additionally, this relaxation can reduce intraabdominal pressure, improve complete ventilation and thereby reduce the need and duration of invasive ventilatory support, as reported in several series.39,40,43 Muscle paralysis is achieved in the first 10 days, and the maximum effect is reached after 3–4 weeks, with decreasing duration the following 6–9 months.43 Therefore, most authors suggest to carry out the wall repair after 30 days, with the advantage of still having 5–6 more months of the toxin effect to protect the fascial closure.41
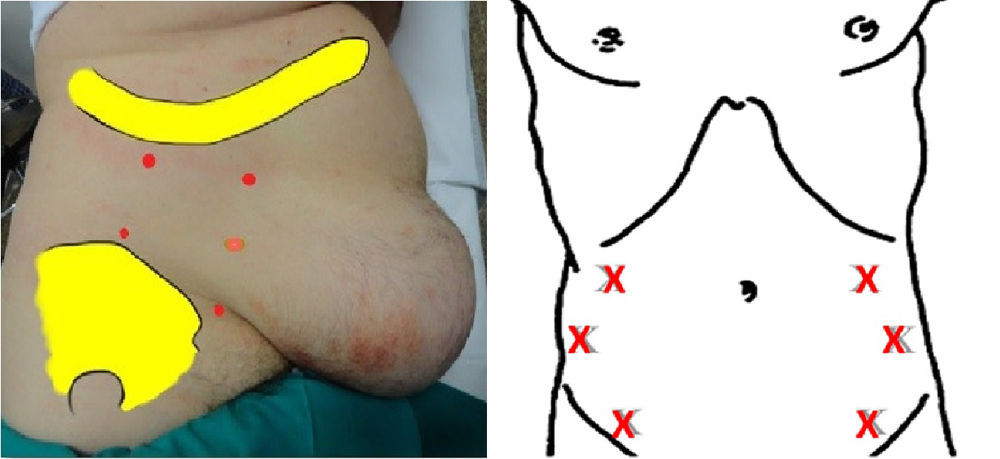
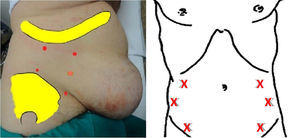
Method for Applying Botulinum Toxin to Abdominal MusclesThe neurotoxin is applied in the outpatient setting 4 to 6 weeks before hernia repair surgery. Surgeons usually administer it themselves, although in one group these injections are given by a neurophysiologist.1 The location of the points for injection is guided by ultrasound in order to visualize the 3 lateral muscle layers to be infiltrated (external oblique, internal oblique and transverse).40–43 A new contribution, together with ultrasound, is the guidance by electromyography, whose goal is to precisely identify and confirm whether the muscle where the neurotoxins applied is denervated or fibrotic depending on the history of previous surgeries or the incision type, and even allows one to change the point of administration to another muscle area in order to ensure the desired effect1 (Fig. 3).
The patient is placed in a lateral position, following the Ibarra-Hurtado model.9 Generally, 5 points of infiltration are defined: 2 on the axillary midline, at equidistant points between the rib edge and the iliac crest, as well as 3 more points on the anterior axillary and mid-clavicular line between the rib edge and superior iliac crest. This method is repeated on the contralateral side of the abdomen.
A 5ml injection of Dysport® (50 units/5ml) or 3ml of Botox® (30 units/5ml) are administered at each point. If we use the commercial brand Dysport® for this technique, 50U of toxin are infiltrated in each of the 5 specific points on the right side and 5 on the left, for a total of 500U. When the Botox® brand is used, the equivalent is 300 units, divided in the same manner.
Other workgroups37,39,41,42 base the location of the infiltration points on the Smooth model,45 which entails 3 points on each side of the abdomen, situated on the anterior axillary line equidistant between the inferior edge of the rib and the anterior superior iliac spine (Fig. 4).
Combination of Both Preoperative TechniquesTwo groups have described to date the benefits of combining PPP and BTX (Table 3), although it is difficult to analyze the independent effect of each preoperative technique, as their effects overlap in time prior to surgery.1,37
Series Published About the Combination of PPP and BTX in the Treatment of LOD Hernias.
| Author | No. | Type of hernia | Mean insufflation time (days) | Total volume of insufflated air (cc) | Total dose of BT (units) | Primary fascial closure (%) | Recurrence (%) | Follow-up time (months) |
|---|---|---|---|---|---|---|---|---|
| Elstner et al., 201637 | 16 | Ventral hernia | 6.2 | – | 300 (Botox) | 100 | 0 | 21 (5–37) |
| Bueno-Lledó et al., 20171 | 45 | Incisional hernia | 7 | 8600 (4500–13250) | 500 (Dysport) | 100 | 2 (4.4) | 40.5 (12–60) |
“Case reports”, only series with 5 or more patients.
It has been demonstrated that the combination of both techniques is useful in the management of LOD hernias, for treating hernia diameters and volumes as a preamble to surgical repair. In this manner, Bueno-Lledó1 were able to achieve an increase in VIH of 480cc after PPP and BTX (P=.003) and the VAC increased by 2121cc (P=.020). Before and after PPP, the VIH/VAC proportion was 27.9 and 13.9%, respectively (P=.001), with a significant reduction of 14%. A significant reduction was also observed in the longitudinal and transverse diameters of the hernia defect. These values could indicate the beneficial and synergic effect obtained with the combination of the 2 procedures compared with the results obtained with each technique separately.3,9,11,21 Thus, the PPP is more useful in the management of the 2 volumes (direct effect on the VIH/VAC ratio), while the effect of BTX lies in reducing the mainly transversal diameters of the defect, by achieving the temporary retraction of the lateral abdominal muscles.1
The hypothesis has also been proposed that the use of BTX complements the effect of PPP, as the flaccid paralysis of the lateral muscles accelerates the stretching of the abdominal wall. This effect enables us to manage greater insufflation volumes by temporarily relaxing the muscles, thereby shortening the duration of the PPP administration period. Elstner37 achieved fascial closure in 16 patients with recurrent ventral hernia by means of assisted laparoscopy after the combination of both preoperative techniques, and no hernia relapse was observed during the follow-up period. However, the series highlighted the appearance of complications associated with PPP, including pneumothorax, pneumomediastinum and metabolic acidosis, although the cycle of administration was able to be completed. The increase in abdominal perimeter after the combination of BT and PPP was 5.6% (P<.006), which enabled hernia repair with no postoperative complications.
In summary, it can be affirmed that PPP and BTX, used separately or in combination, are safe techniques that patients tolerate well. They are effective preoperative tools for the treatment of LOD hernias. Nonetheless, more prospective studies are needed that combine or compare both preoperative techniques to confirm these results.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Bueno-Lledó J, Torregrosa Gallud A, Jiménez Rosellón R, Carbonell Tatay F, García Pastor P, Bonafé Diana S, et al. Preparación preoperatoria de la hernia con pérdida de domicilio. Neumoperitoneo progresivo y toxina botulínica tipo A. Cir Esp. 2017;95:245–253.