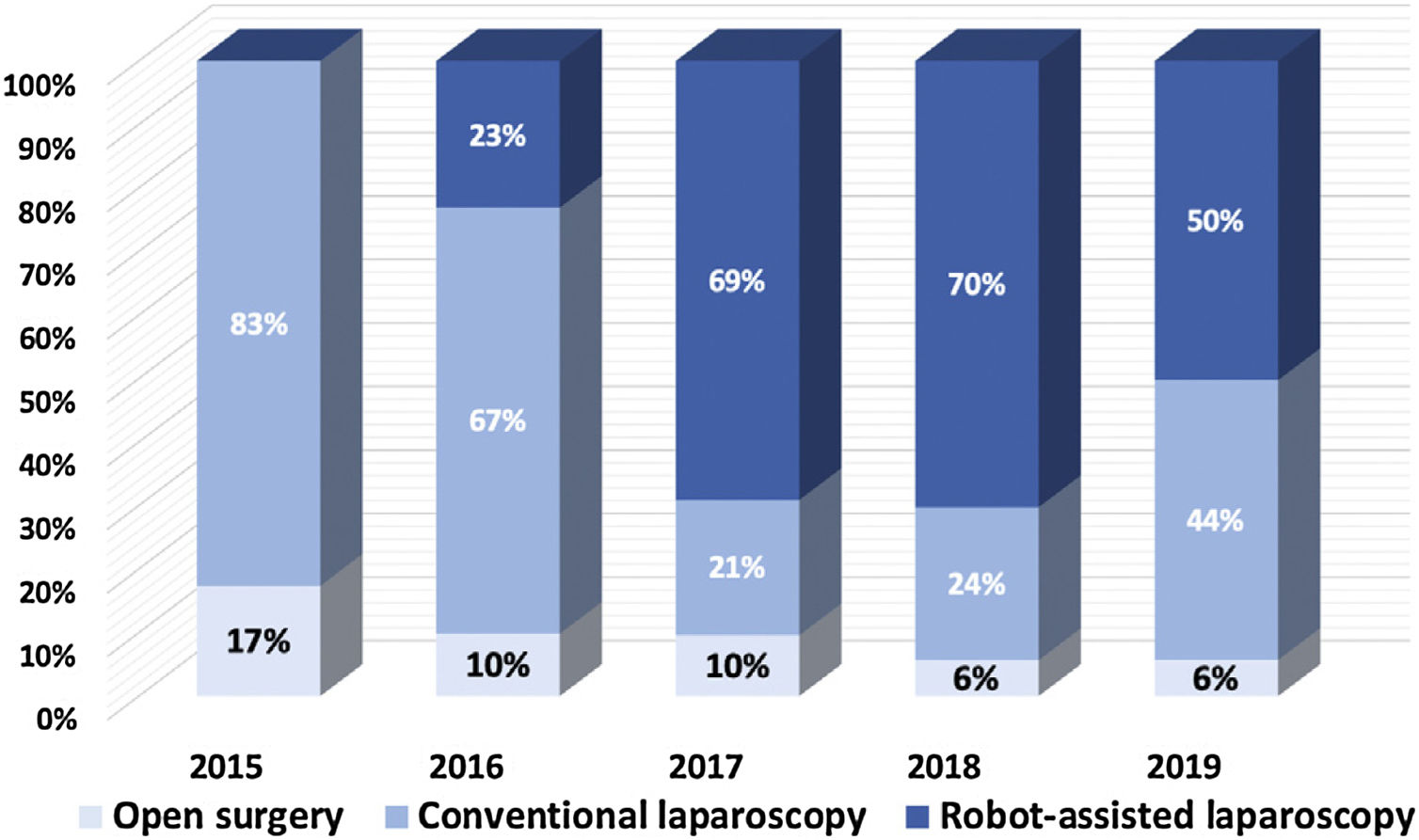
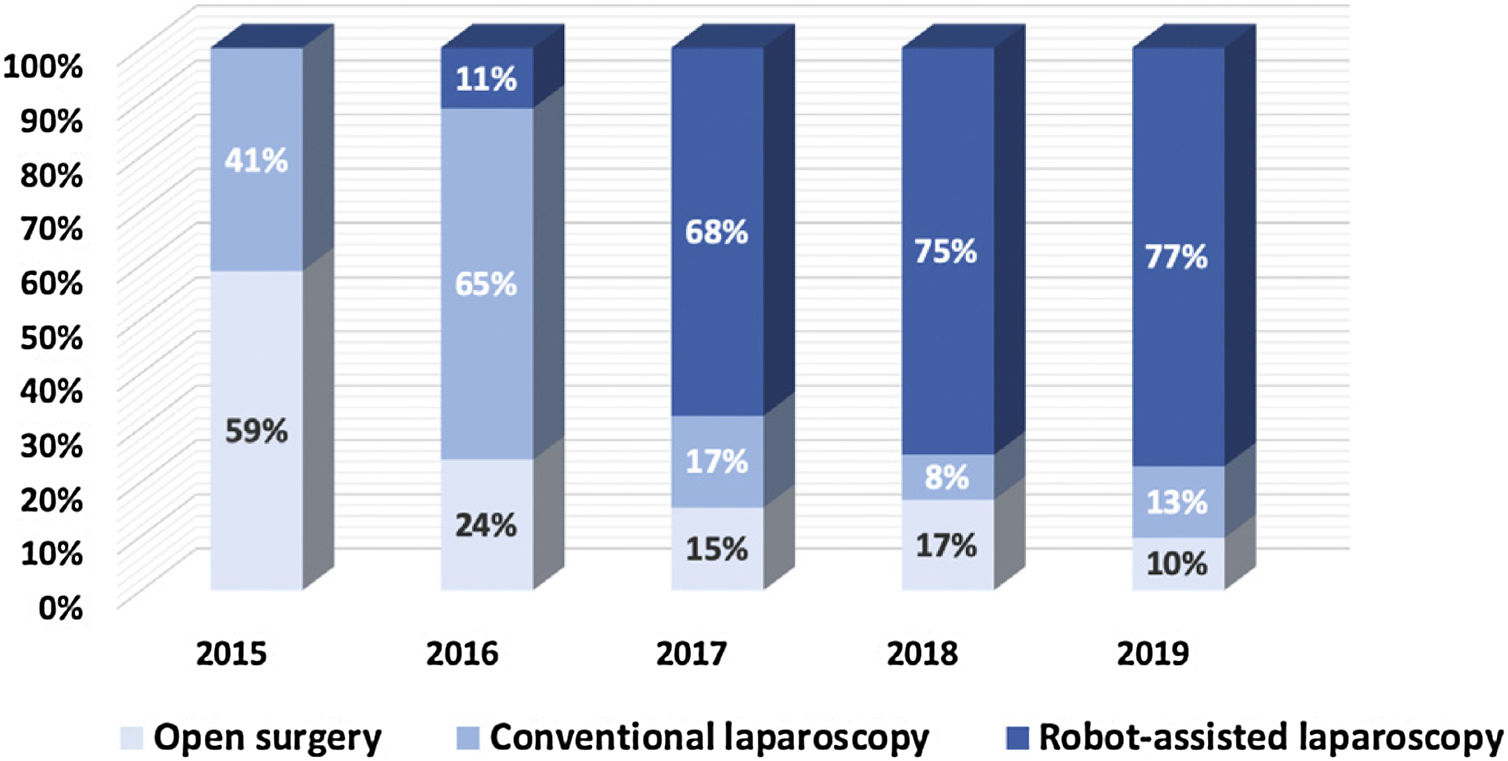
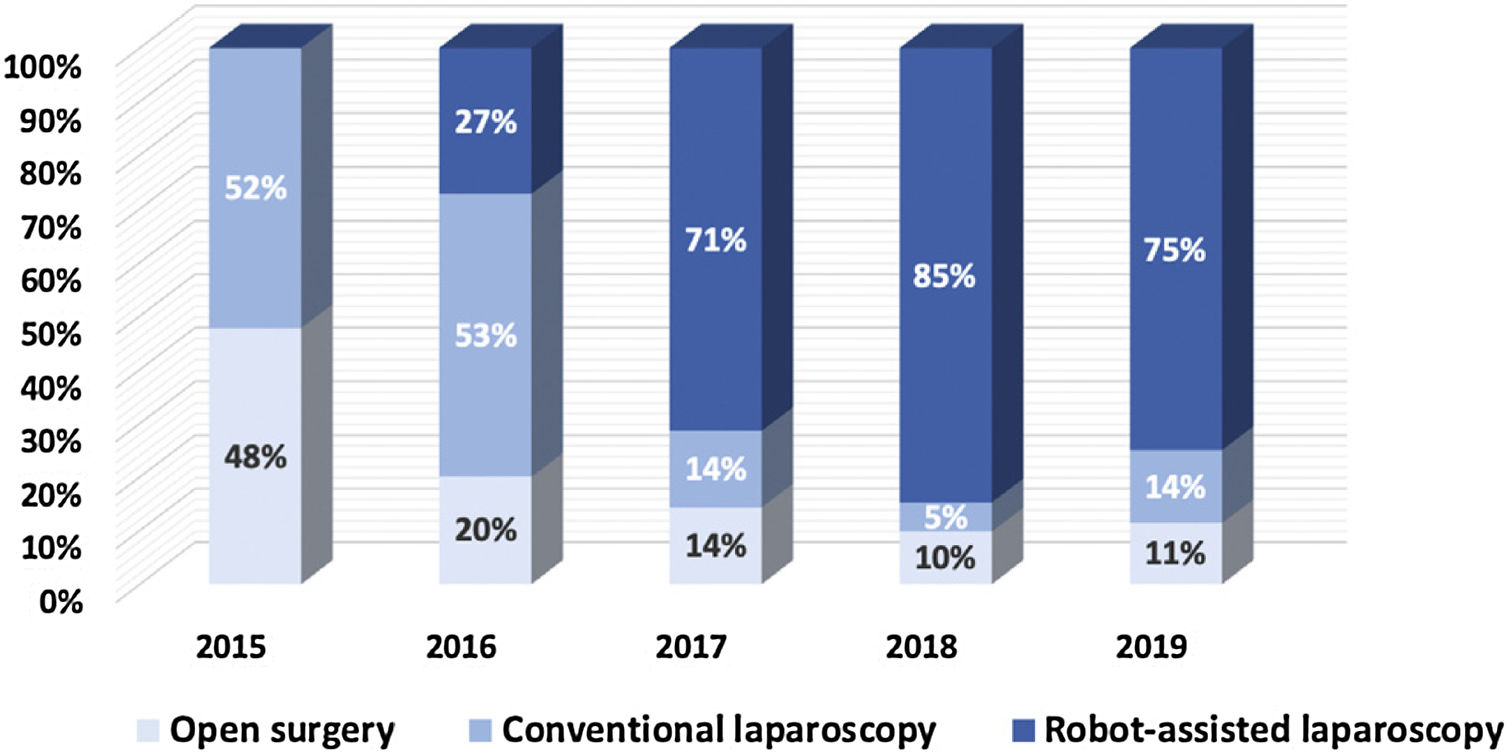
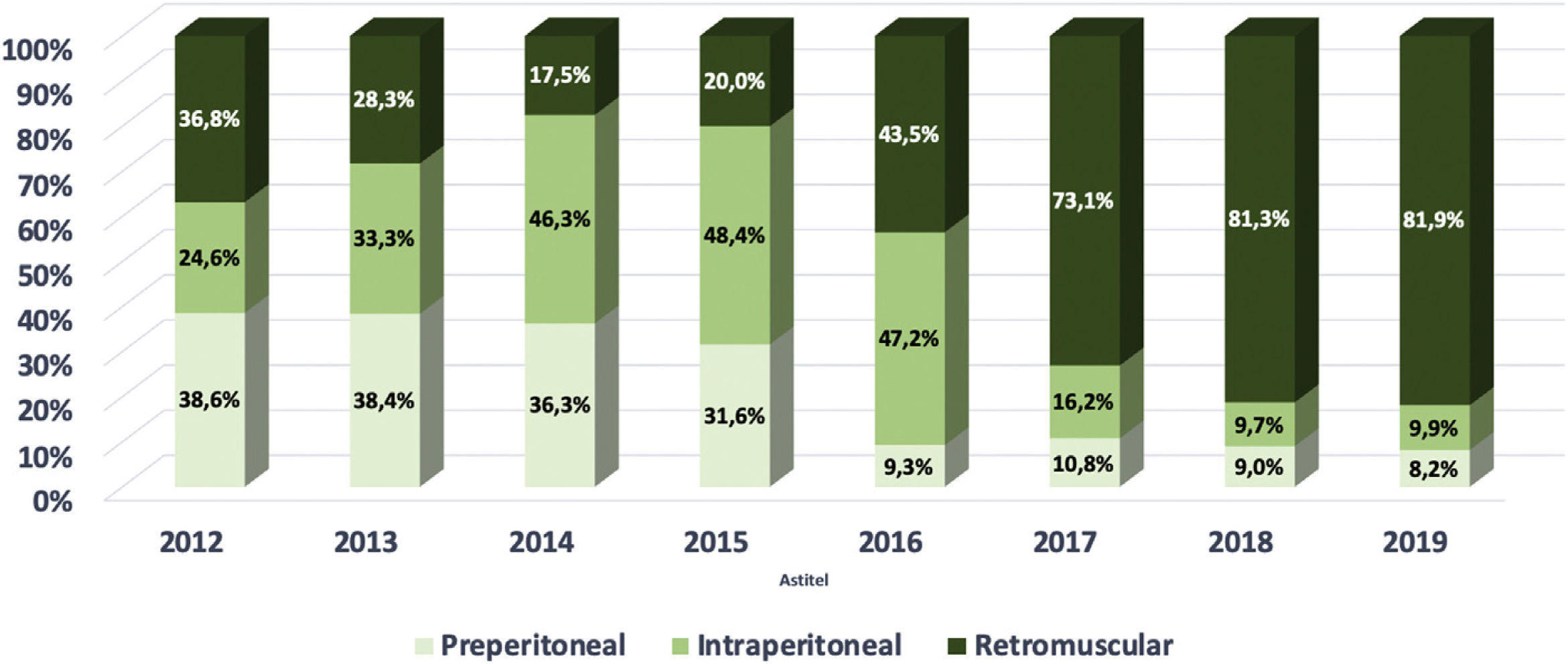
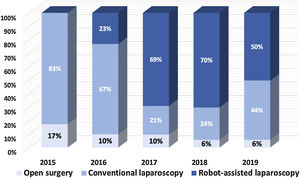
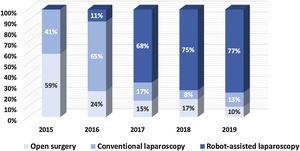
We describe the evolution in hernia repair approaches in our practice during the first 3 years of adopting robotic assisted laparoscopic surgery. For inguinal hernia repair, we began using the robotic platform for complex hernias, and the use of open repair decreased from 17% to 6%. For primary ventral hernias, open procedures decreased from 59% to 10% and for incisional ventral hernias, from 48% to 11%. Moreover, a large shift in mesh position for ventral hernias was seen, with an increase of the retromuscular position from 20% to 82% and a decrease of intraperitoneal mesh position from 48% to 10%.
The robotic platform seems to hold a significant potential for complex inguinal hernias, in addition to ventral and incisional hernias which require component separation. A shorter hospital stay and less postoperative complications might make the adoption of the robotic platform for abdominal wall surgery a valuable proposition.
Describimos la evolución de nuestra práctica en el abordaje quirúrgico de la hernia durante los primeros 3 años, después de la adopción de la cirugía laparoscópica asistida por robot. Respecto a la reparación de las hernias inguinales, comenzamos usando la plataforma robótica para hernias complejas y el uso del abordaje abierto disminuyó del 17 al 6%. Para las hernias ventrales primarias, los procedimientos abiertos disminuyeron del 59 al 10% y para las hernias incisionales del 48 al 11%. Además, se produjo un cambio importante en el posicionamiento de la malla para las hernias ventrales con un aumento de la posición retromuscular del 20 al 82% y una disminución de la posición intraperitoneal del 48 al 10%.
La plataforma robótica parece tener un potencial significativo para las hernias inguinales complejas, además de para las hernias ventrales e incisionales que requieren una separación de componentes. Una estancia hospitalaria corta y menos complicaciones postoperatorias pueden hacer que la adopción de la plataforma robótica para la cirugía de la pared abdominal sea una propuesta valiosa.
In the United States, robotic assisted general surgery has witnessed a formidable growth over the last few years. It has overtaken urological and gynecological surgery in number of cases being performed using the robotic platform. Abdominal wall surgery has contributed significantly to this growth, both the for treatment of ventral and inguinal hernias.1 This study investigates the utility of using the robotic platform to treat abdominal wall hernias and identifies treatment patterns that have changed during the initial 3 years of adopting robotic surgery in our practice.
MethodsStudy design. This is a retrospective and descriptive single center study of robotic assisted laparoscopic abdominal wall surgery during the initial 3 years of its adoption.
Setting. The study was performed at the Department of Surgery of Maria Middelares Hospital in Ghent, Belgium. All operations were performed by one surgeon with extensive experience in open and laparoscopic abdominal wall surgery prior to the adoption of robotic assisted surgery. The robotic program commenced in September 2016.
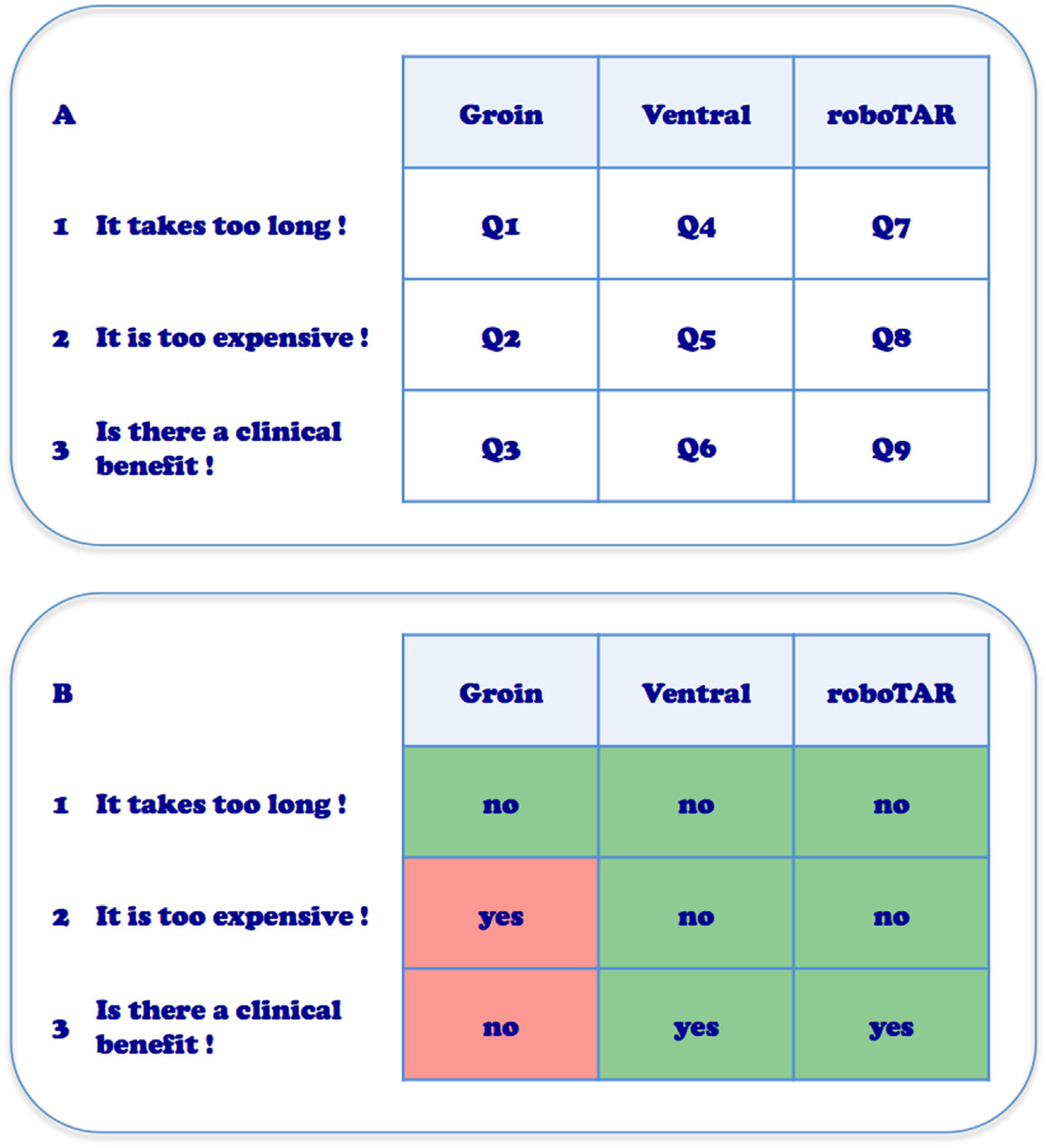
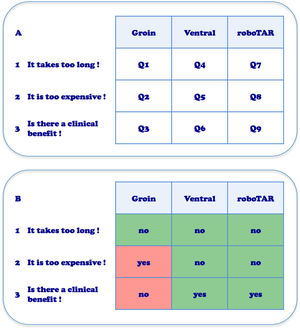
The ROBUST hernia projectRobotic assisted surgery first noted widespread adoption in urology with minimal invasive prostatectomy.2 Gynecologic and colorectal surgery were also relatively early adopters. It was at the 17th Annual Americas Hernia Society meeting in Washington DC, March 2016, that we became aware of the increasing interest by surgeons to adopt the robotic platform for repair of abdominal wall hernias. Healthy skepticism caused us to question the use of the robot for general surgery and for hernia surgery specifically. We had the same objections as many: firstly, “It takes too long”; secondly, “It is too expensive” and thirdly, “What is the clinical benefit for the patient?”. On the other hand, the early adopters of robotic assisted laparoscopic hernia surgery presented inspiring videos. Some face to face discussions with those pioneers, like Conrad Ballecer from Phoenix, Arizona, triggered our interest and curiosity. In the hospital Maria Middelares Ghent, Belgium we had at that time a new latest generation robotic platform daVinci Xi (Intuitive Surgical, Sunnyvale, CA, USA) which was used two days a week by the urologist. Within the department of general surgery, we had discussions with hospital management regarding indications within general surgery where the robotic platform might be useful. We then decided in our department to develop a program investigating the adoption of the robotic platform for the treatment of abdominal wall hernias. In the ROBUST hernia project, (ROBotic Utility for the Surgical Treatment of hernias) we planned to perform a pilot assessment of 50 groin hernias, 40 smaller ventral hernias and 10 wider ventral hernias requiring component separation (roboTAR). Dividing abdominal wall hernias in those 3 indications and posing the 3 questions about robotic assisted hernia surgery mentioned higher, left us with 9 research questions (Q1–Q9) to investigate (Fig. 1).
A. Nine research questions identified for the adoption of robotic hernia repair, dividing hernias in 3 indications and posing the 3 major questions about robotic assisted surgery (Q1–Q9). B. Personal current opinion on the 9 research questions after 3 years of adopting robotic assisted hernia repair with experience from 798 procedures.
The robotic platform includes a teaching pathway to implement safe introduction of clinical practice.3 It is essential that the surgeon who is first starting robotic surgery follow the educational training modules online and commits to practice on the simulator. Once acquainted with the robotic platform, a clinical case observation of robotic surgery performed by an expert followed by hands-on training on cadavers, are obligatory steps toward clinical adoption. When performing the first cases using the robotic platform, the presence of an experienced proctor in the operating room is essential to overcome the initial insecurities a surgeon might experience when working with new robotic technology. The importance of a comprehensive training pathway cannot be overestimated for safe introduction of robotic assisted surgery. Also, selecting easy and straightforward procedures in the beginning is recommended. For abdominal wall surgery, 25 uncomplicated inguinal hernia repairs as part of the initial case series will create the skill set and proficiency to continue with more complex ventral hernia cases.
Data extraction. We record all our abdominal wall surgery procedures prospectively in the EuraHS database (European Registry of Abdominal Wall hernias), which allowed us to examine patterns of change in surgical practice during the years before and after adopting robotic abdominal wall surgery.4 Data extracted include: type of access (open surgery, conventional laparoscopy or robotic assisted laparoscopy) and type of mesh position (intraperitoneal, preperitoneal, retromusclar or onlay repair).
ResultsThe EuraHS database captures prospectively data for all consecutive ventral hernia repairs since January 2012 and of inguinal hernia repairs since March 2015. Until the end of 2019, a total of 938 ventral hernias and 864 inguinal hernias have been repaired. Ventral hernias included primary ventral hernias (n=438), incisional ventral hernias (n=451) and parastomal ventral hernias (n=49).
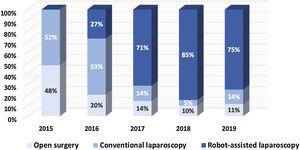
Fig. 2 depicts the evolution in our approach for inguinal hernia treatment and shows an increase in minimal invasive approaches and a decrease in the utilization of the open approach from 17% in 2015 to 6% in 2019.
Fig. 3 depicts our transition from open surgery toward minimal invasive robotic assisted repair of primary ventral hernias and Fig. 4 demonstrates a similar trend for incisional hernias. The changes in our preferential anatomical plane for mesh repair are illustrated in Fig. 5, with a large increase in retrorectus repairs and a decrease in intraperitoneal mesh placement.
Most studies describing robotic assisted inguinal hernia repair (rTAPP – robotic TransAbdominal PrePeritoneal) report longer operative times compared with conventional laparoscopic repair.5 Some reported however a similar operating time for rTAPP once the learning curve of the surgeon has been surpassed.6,7 We prospectively analyzed the operating time of rTAPP groin hernia repair in our initial 50 cases.7 We found that after a series of about 20 cases, the skin to skin operating time was similar both for unilateral and bilateral rTAPP. Also, in a larger study where we compared 272 conventional TAPP versus 404 rTAPP inguinal hernia repairs, the median operating time was comparable, with, 47min versus 45min for unilateral repairs and 62min versus 60min for bilateral repairs respectively.8
Most studies have found rTAPP to be significantly more expensive than conventional laparoscopic surgery. In a study on the economic assessment of adopting robotic assisted inguinal hernia repair we found that the robotic approach had an extra mean cost of 649€ in our hospital.8 This higher cost will limit the potential for adopting a robotic approach for all uncomplicated inguinal hernias. Nevertheless, we do think that rTAPP inguinal hernia repair is probably the best index operation for surgeons to learn how to handle the robotic platform and acquire essential skills needed for more complex abdominal wall hernia repairs. The surgeon is able to obtain the necessary experience with docking, robotic instrumentation, dissection, suturing and mesh handling during a well standardized and common surgical indication. We recommend that any surgeon and operating room team who are commencing a robotic hernia program follow the pathway of completing 25 inguinal hernia repairs before moving on to more complex ventral hernia repairs.
Is there a clinical benefit for inguinal hernia patients operated with the robotic platform compared with conventional laparoscopy? Conclusions in literature are heterogeneous. A systematic literature review from 2018 noted lower postoperative complications in rTAPP compared with open inguinal hernia repair, but did not find a difference between rTAPP and conventional TAPP.5 Also, the only RCT currently published on the topic, did not find any significant clinical benefit at 30 days postoperatively.9 Clinical outcomes for laparoscopic inguinal hernia repair, both with and without the robotic platform, proved to be excellent in our patients.8 A group of complex inguinal hernias that we initially addressed consistently with an open approach before adoption of the robotic platform, is now being treated minimally invasive due to enhanced visualization, availability of wristed instruments and a more stable operating field. Others have seen a similar shift toward a robotic approach for these complex inguinal hernias such as: inguinal hernias after previous abdominal prostatectomy, large non-reducible inguinoscrotal hernias and recurrences after previous preperitoneal meshes.6 More specifically, patients who need removal of a previous preperitoneal mesh seem to benefit greatly from the technological advantages that the robotic platform offers.
Robotic assisted laparoscopic ventral hernia repairFor many years we have used small round mesh devices to treat small and medium sized ventral hernias. This is often a quick and straightforward procedure, but already early in our experience we reported some severe adverse events related to the use of these intraperitoneal mesh devices.10 Moreover, we reported a high recurrence rate for ventral hernias larger than 2cm.11 This is probably due to the fact that these mesh devices are limited in size and thus have a restricted amount of overlap beyond the hernia defect. Therefore, we now prefer larger flat meshes for the repair of medium and large ventral hernias. There are several anatomical planes one can use to place mesh. Laparoscopic surgery has shown an advantage with less wound morbidity and traditionally is performed with an intraperitoneal mesh fixed with sutures and/or tackers. However, there is increasing evidence that subsequent abdominal surgery after previous intraperitoneal mesh placement has an increased risk of morbidity related to adhesions.12,13 Other options are now increasingly used to avoid intraperitoneal mesh placement. In ventral TAPP, a mesh is placed in the preperitoneal plane. This allows the use of a cheaper, uncoated mesh, while the peritoneal layer functions as antiadhesive barrier between the mesh and the viscera. Another option is utilization of the retromuscular plane. In minimal invasive retromuscular ventral hernia repair, the technique as described by Rives14 and Stoppa15 to repair ventral hernias with a retrorectus mesh placement within the rectus sheath, can be performed via an endoscopic approach. The retrorectus plane is approached either through a limited incision on the midline (MILOS approach: Minimal Invasive or Less Open Sublay repair), via a transabdominal approach (TARUP: Trans Abdominal Retromuscular Umbilical Prosthesis) or via an extraperitoneal approach (eTEP access: extended Totally Extra Peritoneal access).
In our practice, the TARUP technique is the preferred approach to access the retrorectus plane for repair of ventral hernias. It was previously described by Chowbey et al. in 2003 and by Schroeder et al. in 2013 using conventional laparoscopy.16,17 They found the technique to be safe and effective, but technically demanding. Using the robotic platform, the TARUP technique has been facilitated and is more reproducible. We reported operative times comparable with open retromuscular repairs using similar sized meshes once the learning curve had been surpassed.18 The robotic TARUP technique allows placement of a mesh with enough overlap beyond the hernia defect to establish a durable repair. Moreover, the extraperitoneal positioning of the mesh avoids the life-long presence of an intraperitoneal mesh, and avoids the need for penetrating mesh fixation with sutures or tackers. Therefore, a decrease in postoperative pain related to this penetrating fixation is anticipated. Although the cost for instrumentation of a robotic approach is higher, it allows the avoidance of a more expensive composite intraperitoneal mesh and tackers, which makes this treatment change cost neutral. We believe that the adoption of the robotic approach for ventral hernias has allowed us to perform more durable repairs with less postoperative pain from penetrating mesh fixation and has decreased the risk of potential adverse events from adhesions to the intraperitoneal mesh.
Robotic assisted component separation techniqueWe are confident that the main clinical value in adopting the robotic platform for hernia repair lies in the treatment of wide incisional hernias where a component separation technique is needed to close the hernia defect and place a large mesh. Traditionally, we performed a posterior component separation by TAR (Transversus Abdominus Release) using an open approach in those patients. These procedures have a significant risk of wound morbidity, a prolonged hospital stay and a prolonged interval to return to normal mobility and oral intake. We found that performing a minimal invasive approach for these complex abdominal wall reconstructions resulted in a significant decrease in hospital stay. This is in line with other case series describing a remarkable reduction in hospital stay for robotic assisted surgery for incisional hernia.19–22 This is likely related to earlier mobilization due to decreased postoperative pain and less postoperative ileus, which is often seen in the early postoperative period following open extensive abdominal wall reconstruction. Although evidence from high quality prospective studies this is still lacking, we are convinced by our clinical experience that it is only a matter of time before this evidence of improved clinical outcome in these patients will emerge.
Conflicts of interestF. Muysoms reports having received research grants from Intuitive, Medtronic, Dynamesh and received speakers honorarium from Medtronic, Bard-Davol, Dynamesh, Intuitive and received consultancy fees from Medtronic, Intuitive, CMR Surgical. F. Nachtergaele, P. Pletinckx and M. Dewulf have no conflicts of interest or financial ties to disclose.