Rectal prolapse is defined as a full-thickness protrusion of the rectal wall through the anal canal. It commonly occurs in elderly women due to weakness of the pelvic floor muscles, and it is uncommon in young men.1
Rectal prolapse is differentiated between 3 clinical entities: mucosal prolapse (partial or pseudoprolapse), internal prolapse (rectal intussusception) and total prolapse (complete or true).2 Mucosal prolapse is generally the result of injuries such as hemorrhoids or polyps. Intussusception can be a full or partial thickness disorder, but the tissue does not extend beyond the anal canal, unlike total prolapse.
The condition usually develops progressively: it is initially spontaneously reducible, then manually reducible, and finally irreducible. At any stage, it can be complicated by incarceration or strangulation, which are very rare.
Incarcerated rectal prolapse is a surgical emergency,3 and urgent perianal rectosigmoidectomy is the treatment of choice in these cases.4
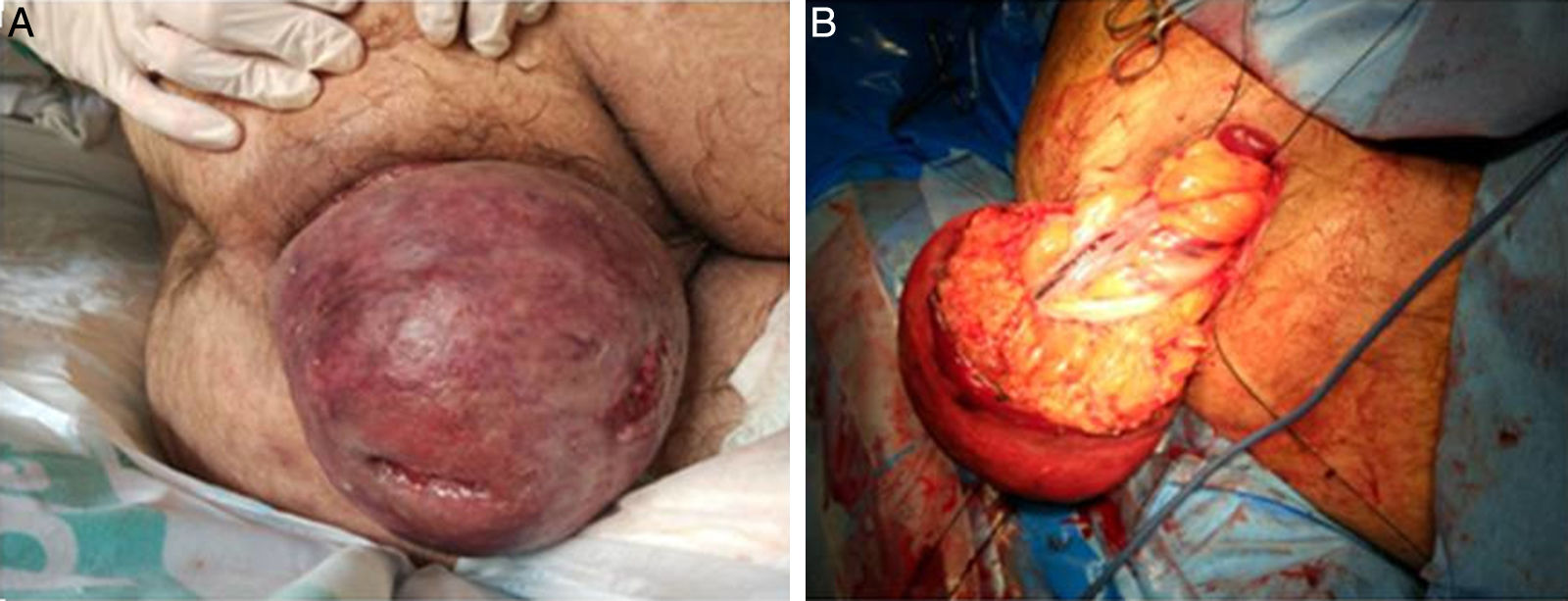
We present the case of a 42-year-old male with a history of erectile dysfunction and rectal prolapse secondary to a traumatic burst fracture of the L4 vertebral body 20 years earlier. In the context of admission for AMI, the patient complained of discomfort due to not having practiced regular manual reduction of the prolapse. He presented a complete rectal prolapse of 20cm, with edematous, violaceous mucosa and a surface that appeared to have chronic ulceration (Fig. 1).
After the failure of all conservative reduction procedures, hyperosmolar compresses, massage, and Trendelenburg under general anesthesia, we performed emergency perineal rectosigmoidectomy (Altemeier procedure).
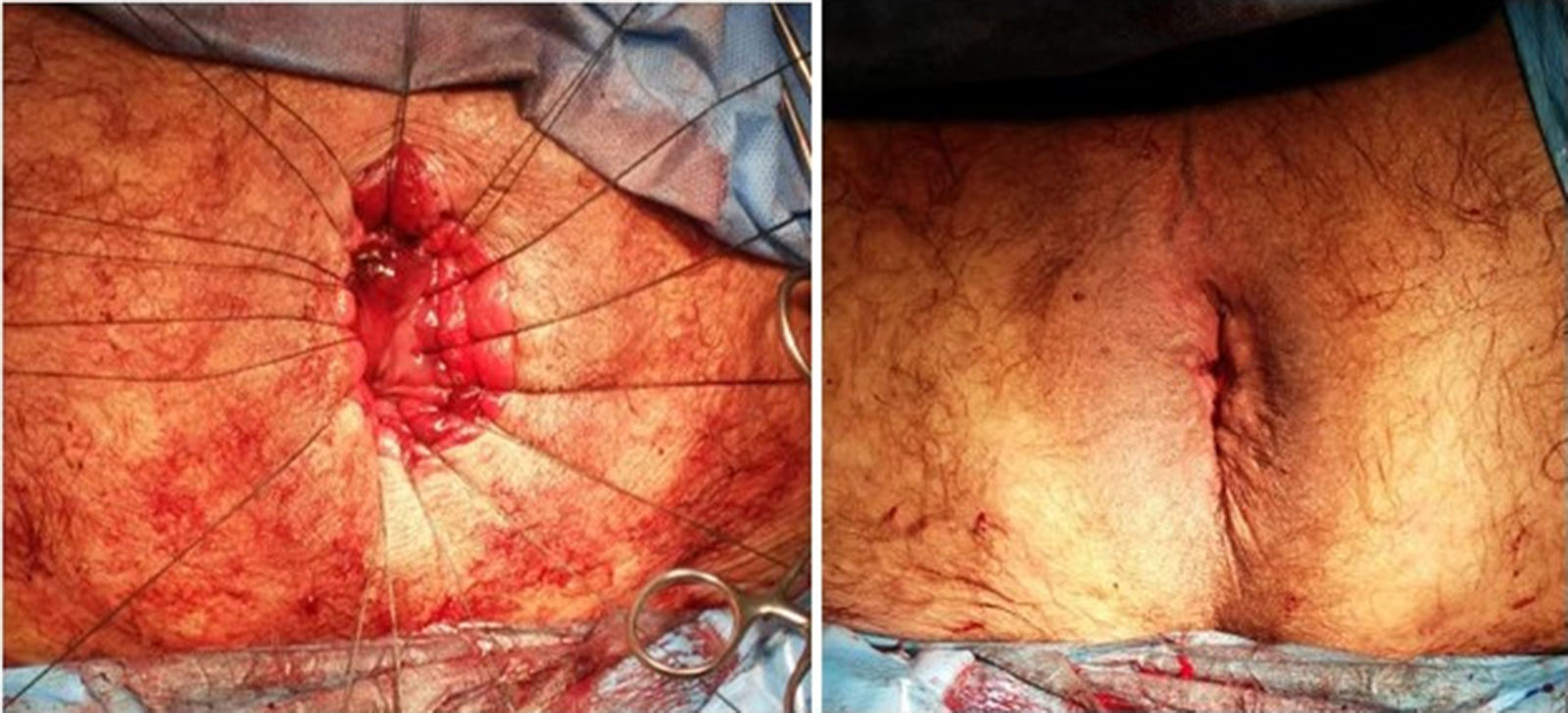
A complete rectal wall incision was made 2–3cm from the dentate line. The mesorectum and mesosigmoid vessels were controlled with a high-energy source; 15cm of the prolapsed rectum were resected (Fig. 1), and coloanal anastomosis was created manually (Fig. 2). We did not perform associated levator repair or colostomy.
The patient’s evolution was satisfactory, with no digestive or cardiological complications, and he was discharged on the 5th postoperative day. At the initial follow-up office visit, he reported correct continence and no recurrence.
There is still debate about the pathophysiological mechanism of rectal prolapse, but chronic abdominal strain is present in most cases. The most common form is the chronic course of the disorder, which is studied with diagnostic tests that include sigmoidoscopy, videodefecography, endoanal ultrasound, and anal manometry. In the context of incarceration, diagnostic tests are omitted since urgent surgical treatment is required.
Surgical treatment seeks to correct the anatomy of the prolapse, restore continence, and improve constipation and evacuation. Classically, 2 approaches are described (perineal and abdominal) for fixation, intestinal resection, or plication. The choice of technique is made based on the clinical and functional characteristics of the patient.
In urgent situations, when the prolapse cannot be reduced manually, certain techniques can help the intestine return to its anatomical position. Sedation, Trendelenburg position, and topical application of salt and sucrose can reduce intestinal edema and allow for reduction.5 However, when the prolapsed intestine is strangulated, it becomes a surgical emergency, as was the case in our patient. The technique of choice is perineal rectosigmoidectomy, either with or without associated colostomy.3,6
As this is a rare condition, we have found few published data in the literature. Most are from historical series, such as the article by Ramanujam et al., which described 8 cases of incarcerated rectal prolapse over a period of 9 years treated with perineal rectosigmoidectomy. All the patients were women over the age of 75, and 2 (25%) developed postoperative anastomotic leak with peritonitis that required reoperation to perform a colostomy.7
In recent years, there has been a trend to offer elective perineal rectosigmoidectomy in younger patients, especially in men.8 However, and despite being an adequate solution for urgent presentations, the recurrence rate after the Altemeier intervention is not negligible (3%–16%) and is still high compared to abdominal approaches.9 Furthermore, the restoration of continence after surgery is also unpredictable, so the addition of levator repair to the perineal rectosigmoidectomy (Prasad variation) has been suggested to achieve better results, although this factor has not been shown to prevent possible recurrence.10
Please cite this article as: Allué Cabañuz M, Gonzalo Rodriguez MA, Navarro Gonzalo AC. Prolapso rectal incarcerado: rectosigmoidectomía perineal urgente. Cir Esp. 2021;99:164–166.