Total bile acid (TBA) is associated with portal hypertension, a risk factor for post-hepatectomy liver failure (PHLF). We conducted this study to clarify whether TBA is also associated with PHLF in patients with hepatocellular carcinoma (HCC).
MethodsWe recruited patients with HCC and Child-Pugh class A, who underwent liver resection, and applied multivariate analyses to identify risk factors for PHLF.
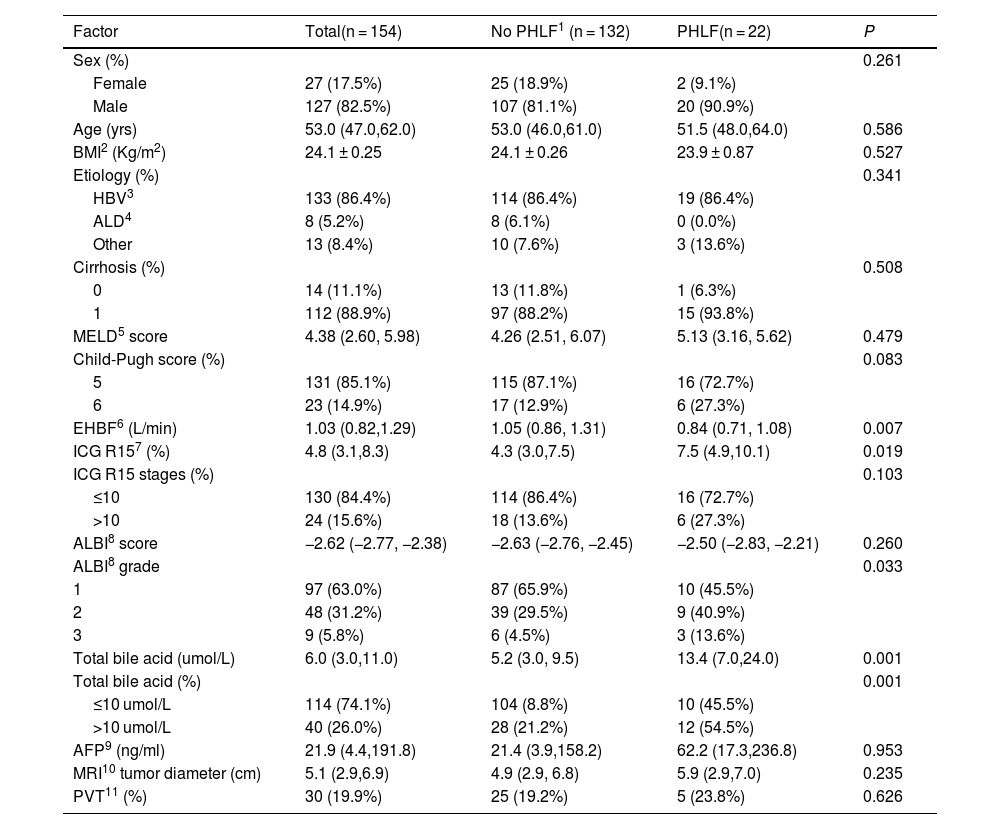
ResultsWe analyzed data from 154 patients. The prevalence of PHLF was 14.3%. The median maximum tumor diameter was 5.1 cm (2.9–6.9 cm). The proportions of patients with elevated TBA levels (P = 0.001), severe albumin-bilirubin (AIBL) grades (P = 0.033), and low platelet counts (P = 0.031) were significantly higher within the subgroup of patients with PHLF than in the subgroup without PHLF. The multivariate analysis results suggest that TBA level (OR, 1.08; 951.03–1.14; P = 0.003) and MRI tumor diameter (OR, 1.17; 95% CI, 1.01–1.35; P = 0.038) are independent preoperative risk factors for PHLF. The TBA levels correlated with the indocyanine green retention rate at 15 minutes (P = 0.001) and the effective hepatic blood flow (P < 0.001), two markers of portal hypertension. However, TBA levels did not correlate with tumor diameter (P = 0.536).
ConclusionsCompared to ICG R15 and AIBL score, preoperative TBA was risk factor for PHLF in Chinese patients with HCC, and it may impact PHLF through its potential role as a marker of portal hypertension.
Los ácidos biliares totales (ABT) están asociados con la hipertensión portal, un conocido factor de riesgo para la insuficiencia hepática post-hepatectomía (IHPH). Sin embargo, no está claro si el ABT está relacionado con la IHPH en pacientes con carcinoma hepatocelular (CHC). Por este motivo, realizamos este estudio.
MétodosSe reclutaron pacientes con CHC y Child-Pugh de clase A que se sometieron a resección hepática en un hospital de referencia. Se utilizaron análisis multivariantes para identificar los factores de riesgo de IHPH.
ResultadosSe incluyeron un total de 154 pacientes con CHC y Child-Pugh de clase A, con una prevalencia de IHPH del 14,3%. El diámetro máximo mediano del tumor fue de 5,1 (2,9, 6,9) cm. Los pacientes con IHPH presentaron un porcentaje significativamente mayor de niveles elevados de ABT (P = 0,001), grado severo de albúmina-bilirrubina (AIBL) (P = 0,033) y disminución del recuento de plaquetas (P = 0,031). El análisis multivariante mostró que el nivel de ABT (OR, 1,08, IC 95%: 1,03-1,14; P = 0,003) y el diámetro tumoral en la resonancia magnética (OR, 1,17, IC 95%: 1,01-1,35; P = 0,038) fueron factores de riesgo preoperatorios independientes para la IHPH. Los niveles de ABT se correlacionaron con el ICG R15 (P = 0,001) y el flujo sanguíneo hepático efectivo (P < 0,001), que son marcadores de hipertensión portal, sin embargo, los niveles de ABT no se correlacionaron con el diámetro tumoral (P = 0,536).
ConclusionesEn comparación con el ICG R15 y la puntuación AIBL, los ABT preoperatorios factores de riesgo de IHPH en pacientes chinos con CHC, y pueden afectar el IHPH a través de su posible papel como marcador de hipertensión portal.