Papillary thyroid microcarcinoma (PTMC) is a papillary carcinoma measuring ≤1cm, whose incidence has been increasing in recent decades.1–3 Due to its generally non-aggressive behavior, more conservative treatment of PTMC is being increasingly preferred, such as thyroid lobectomy.1 Even so, the surgical technique is still a cause for controversy, as total thyroidectomy has less persistence and recurrence2 yet lobectomy presents a lower percentage of postoperative complications.3,4 It is therefore important to identify the factors associated with malignancy of the contralateral thyroid lobe in patients with PTMC who initially underwent lobectomy to determine whether the original technique is sufficient or whether it should be completed. This would minimize the number of postoperative complications, persistence and recurrences.
The objective of this study is to analyze and compare the factors associated with malignancy of the contralateral lobe in patients with PTMC who initially underwent lobectomy.
The study population consisted of patients with PTMC treated in an endocrine surgery unit. We included patients with a minimum follow-up of 2 years who underwent initial lobectomy, followed by thyroidectomy completed within 6 months after surgery. Patients were excluded if the papillary thyroid carcinoma (PTC) was >1cm, or if the patients presented: carcinoma of another histological type in the contralateral thyroid lobe; other synchronous malignant extrathyroid pathologies; thyroidectomy more than 6 months after lobectomy (in this case, the presence of a PTMC would be considered a recurrence of the disease and not persistence).
Two groups were compared: patients in whom the thyroidectomy was completed and there was no evidence of malignancy in the contralateral lobe (group 1); and patients in whom the thyroidectomy was completed and there was evidence of malignancy in the contralateral lobe (group 2).
Data were analyzed for demographic variables (age and sex), clinical variables (history of PTC, body mass index [BMI], thyroid function, thyroid-stimulating hormone [TSH] and thyroxine [FT4] values, contralateral ultrasound nodules in the preoperative evaluation, and surgical indication for lobectomy), and histopathological values (size, number of tumor foci, histological subtype, accompanying pathology, capsular invasion, extracapsular invasion and metastatic lymphadenopathies).
The collected data were analyzed in a database. For categorical variables, data are expressed using frequencies and percentages, and were compared using Pearson's chi-squared test or Fisher's exact test, when appropriate. For continuous quantitative variables, the data are expressed as the mean±standard deviation. The normal distribution of the variables was verified using the Kolmogorov–Smirnov test. The quantitative variables of both groups were compared using the Student's t test for independent data when they followed normal distribution. If they did not follow normal distribution, the nonparametric Mann–Whitney U test was used. In cases where the quantitative variable reached statistical significance, the cut-off point was calculated from which good sensitivity (S) and specificity (Sp) were reached. A P value <.05 was considered statistically significant.
Out of the 161 patients with PTMC treated surgically, in 14.9% (n=24) a lobectomy was initially performed, 54.2% (n=13) of whom had thyroidectomy completed within 6 months after surgery. In the remaining 11 patients, the thyroidectomy was not completed, and no recurrences were observed after a mean follow-up of 116.8±58.5 months.
Out of the 13 patients analyzed, the surgical indication was a Bethesda system category III–IV thyroid nodule in 11 cases, the incidental finding of a thyroid nodule during the intervention of a parathyroid adenoma in one case, and the preoperative clinical diagnosis of PTMC by cytology of a thyroid nodule (Bethesda VI) in the remaining case.
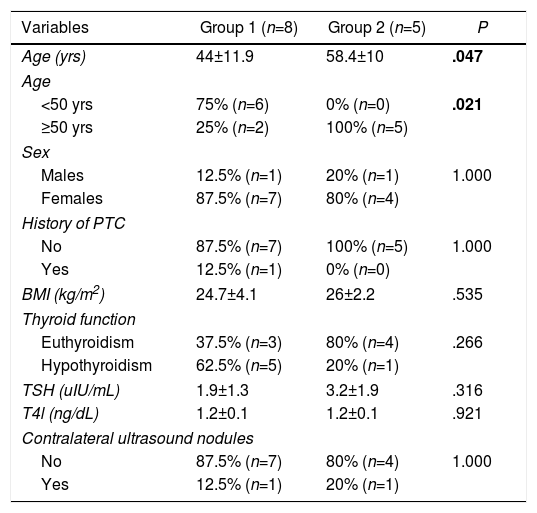
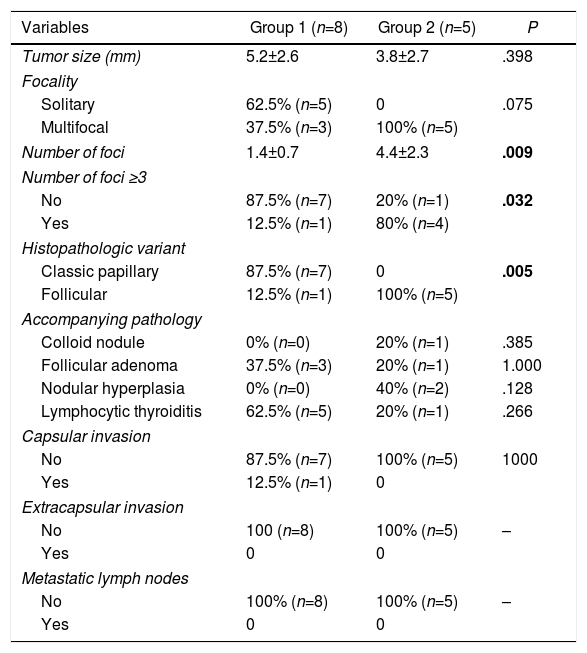
Malignancy in the contralateral thyroid lobe was observed in 38.5% (n=5) of patients. Patients of group 2 were older in age (44±11.9 vs 58.4±10 years; P=.047). Regarding age ≥50 (S 100% and Sp 75% for the diagnosis of contralateral malignancy), the percentage of patients was higher in group 2 (25% vs 100%; P=.021) (Table 1). PTMC with ≥2 tumor foci (S 100% and Sp 62.5%) showed no significant differences between the two groups (37.5% vs 100%; P=.075), but PTMC with ≥3 tumor foci (S 80% and Sp 87.5%) was more frequent in group 2 (12.5% vs 80%; P=.032). Furthermore, we found a greater frequency of the follicular variant of PTMC in group 2 (12.5% vs 100%; P=.005) (Table 2).
Demographic and Clinical Factors Associated With the Presence of Malignancy in the Contralateral Lobe in Patients With PTMC Initially Treated With Lobectomy.
| Variables | Group 1 (n=8) | Group 2 (n=5) | P |
|---|---|---|---|
| Age (yrs) | 44±11.9 | 58.4±10 | .047 |
| Age | |||
| <50 yrs | 75% (n=6) | 0% (n=0) | .021 |
| ≥50 yrs | 25% (n=2) | 100% (n=5) | |
| Sex | |||
| Males | 12.5% (n=1) | 20% (n=1) | 1.000 |
| Females | 87.5% (n=7) | 80% (n=4) | |
| History of PTC | |||
| No | 87.5% (n=7) | 100% (n=5) | 1.000 |
| Yes | 12.5% (n=1) | 0% (n=0) | |
| BMI (kg/m2) | 24.7±4.1 | 26±2.2 | .535 |
| Thyroid function | |||
| Euthyroidism | 37.5% (n=3) | 80% (n=4) | .266 |
| Hypothyroidism | 62.5% (n=5) | 20% (n=1) | |
| TSH (uIU/mL) | 1.9±1.3 | 3.2±1.9 | .316 |
| T4l (ng/dL) | 1.2±0.1 | 1.2±0.1 | .921 |
| Contralateral ultrasound nodules | |||
| No | 87.5% (n=7) | 80% (n=4) | 1.000 |
| Yes | 12.5% (n=1) | 20% (n=1) | |
Variables in bold are statistically significant.
Histologic Factors Associated With the Presence of Malignancy in the Contralateral Lobe in Patients With PTMC Initially Treated With Lobectomy.
| Variables | Group 1 (n=8) | Group 2 (n=5) | P |
|---|---|---|---|
| Tumor size (mm) | 5.2±2.6 | 3.8±2.7 | .398 |
| Focality | |||
| Solitary | 62.5% (n=5) | 0 | .075 |
| Multifocal | 37.5% (n=3) | 100% (n=5) | |
| Number of foci | 1.4±0.7 | 4.4±2.3 | .009 |
| Number of foci ≥3 | |||
| No | 87.5% (n=7) | 20% (n=1) | .032 |
| Yes | 12.5% (n=1) | 80% (n=4) | |
| Histopathologic variant | |||
| Classic papillary | 87.5% (n=7) | 0 | .005 |
| Follicular | 12.5% (n=1) | 100% (n=5) | |
| Accompanying pathology | |||
| Colloid nodule | 0% (n=0) | 20% (n=1) | .385 |
| Follicular adenoma | 37.5% (n=3) | 20% (n=1) | 1.000 |
| Nodular hyperplasia | 0% (n=0) | 40% (n=2) | .128 |
| Lymphocytic thyroiditis | 62.5% (n=5) | 20% (n=1) | .266 |
| Capsular invasion | |||
| No | 87.5% (n=7) | 100% (n=5) | 1000 |
| Yes | 12.5% (n=1) | 0 | |
| Extracapsular invasion | |||
| No | 100 (n=8) | 100% (n=5) | – |
| Yes | 0 | 0 | |
| Metastatic lymph nodes | |||
| No | 100% (n=8) | 100% (n=5) | – |
| Yes | 0 | 0 | |
In bold, statistical significance.
The main disadvantage of lobectomy in the treatment of PTMC is the significant number of recurrences (7.3%–26%),2,3 mostly in the contralateral lobe (84.6%–93.3%).2,5
Because multifocal PTMC is a risk factor associated with involvement of the contralateral lobe,6,7 some studies recommend primary total thyroidectomy to avoid persistence and recurrence.2 In this study, although multifocality was not associated with malignancy in the contralateral lobe, the number of tumor foci ≥3 correlated with malignancy. Therefore, in patients undergoing lobectomy for multifocal PTMC with 3 or more foci, complete thyroidectomy would be recommended, but it may not be necessary in patients with 2 foci of PTMC.
According to reports in the literature, other factors associated with bilateral PTMC include nodular hyperplasia,8 tumor size >5mm,6,7 and the presence of contralateral nodules in the preoperative ultrasound evaluation.7 On the other hand, since cervical lymphadenectomy was not performed in this study, the presence of metastatic lymph nodes could not be assessed. Nonetheless, in our unit, if there is suspicion or confirmation of metastatic lymph nodes in the preoperative evaluation, total thyroidectomy is carried out systematically.
Complete thyroidectomies in patients who had initially undergone lobectomy would not only be indicated to eliminate the possibility of residual disease in the contralateral lobe, but also to enable treatment with 131I in patients at higher risk of recurrence.9 Although the American Thyroid Association does not recommend routine 131I ablation of thyroid remnants in multifocal PTMC due to the number of recurrences (4%–6%),10 in this study 131I was administered in multifocal tumors (n=8).
The limitation of this study is its small sample size, which lowers the statistical power. For this reason, the results must be interpreted with caution.
In conclusion, age ≥50, number of tumor foci ≥3, and the follicular variant in patients with PTMC who initially underwent lobectomy could be considered factors associated with malignancy in the contralateral thyroid lobe, and completion with thyroidectomy should be evaluated in these cases.
Conflict of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Ruiz J, Ríos A, Rodríguez JM, Paredes M, Parrilla P. ¿Qué factores clínicos e histológicos deberían aconsejar que se complete la tiroidectomía en pacientes con microcarcinoma papilar de tiroides tratados inicialmente con una lobectomía? Cir Esp. 2020;98:297–299.