The Spanish Arteriosclerosis Society has accredited more than 70 lipid units across the country. The main criteria for patients to be referred to these units are presented. These are not only grouped by the type of dyslipidaemia or the lipid levels, but also on certain clinical characteristics suggesting primary hyperlipidaemia, a complex diagnosis, or difficult management due to inefficacy, or side effects.
La Sociedad Española de Arteriosclerosis tiene homologadas más de 70 unidades de lípidos repartidas por todo el país. Este artículo resume los principales motivos para remitir pacientes a nuestras unidades, agrupados no solo por niveles de lípidos o por el tipo de dislipidemia, sino además por determinadas características clínicas que hagan sospechar dislipidemias primarias, de diagnóstico complejo o de difícil tratamiento, bien por ineficacia, bien por aparición de efectos adversos.
The practice of treating dyslipidaemia is extremely widespread. As well as not being associated with one particular speciality, it is also part of the routine clinical practice of healthcare professionals regardless of the level of care provided, both in Primary Care and Hospitals. This can partly be explained by the unquestionable benefit that effective dyslipidaemia treatment has on the primary and secondary prevention of vascular disease.
The Spanish healthcare system refers children with dyslipidaemia to specialised endocrinology or gastroenterology units in paediatric hospitals. It is also common practice for patients with dyslipidaemia, sometimes severe, to be cared for at the same units where they are receiving treatment for another condition. For example, in transplant patients with secondary dyslipidaemia or in subjects with dyslipidaemia secondary to HIV and its treatment.
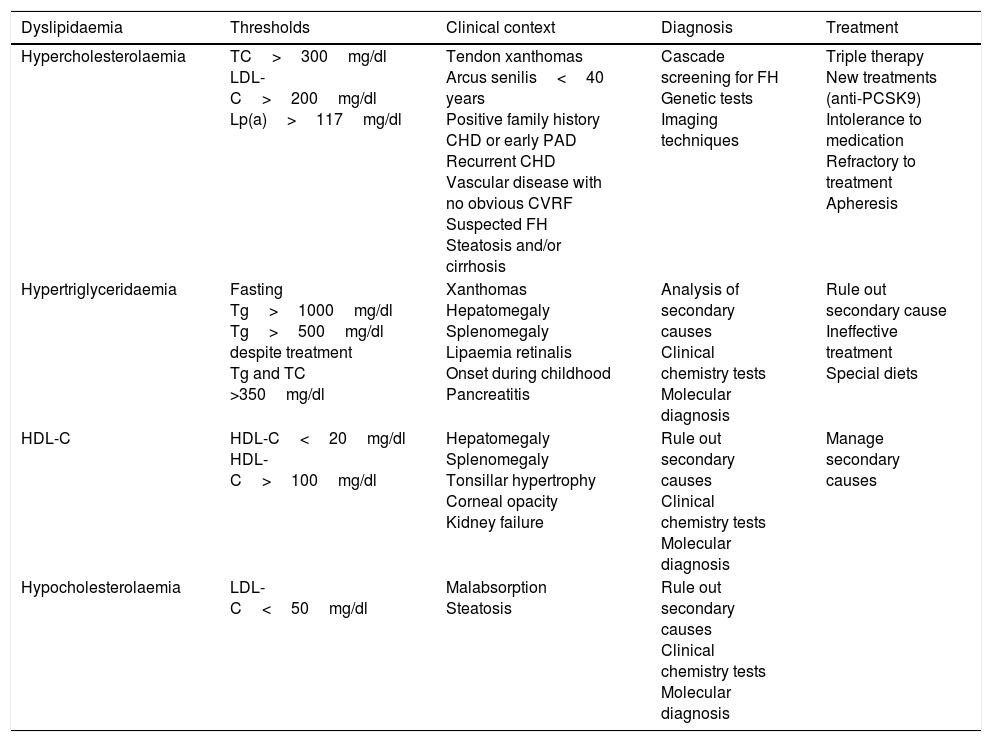
Notwithstanding the foregoing, it is not uncommon for a clinician to be overwhelmed by certain dyslipidaemia patients when they represent a diagnostic challenge, such as in the event of treatment inefficacy or intolerance, or when combination therapy or unusual treatments are required. This document presents the recommendations of the Spanish Atherosclerosis Society (Sociedad Española de Arteriosclerosis, SEA) concerning the types of patient that should be referred to a lipid unit (LU) and the associated clinical criteria. These recommendations are summarised in Table 1.
Criteria for referring patients to Spanish Atherosclerosis Society Lipid Units.
| Dyslipidaemia | Thresholds | Clinical context | Diagnosis | Treatment |
|---|---|---|---|---|
| Hypercholesterolaemia | TC>300mg/dl LDL-C>200mg/dl Lp(a)>117mg/dl | Tendon xanthomas Arcus senilis<40 years Positive family history CHD or early PAD Recurrent CHD Vascular disease with no obvious CVRF Suspected FH Steatosis and/or cirrhosis | Cascade screening for FH Genetic tests Imaging techniques | Triple therapy New treatments (anti-PCSK9) Intolerance to medication Refractory to treatment Apheresis |
| Hypertriglyceridaemia | Fasting Tg>1000mg/dl Tg>500mg/dl despite treatment Tg and TC >350mg/dl | Xanthomas Hepatomegaly Splenomegaly Lipaemia retinalis Onset during childhood Pancreatitis | Analysis of secondary causes Clinical chemistry tests Molecular diagnosis | Rule out secondary cause Ineffective treatment Special diets |
| HDL-C | HDL-C<20mg/dl HDL-C>100mg/dl | Hepatomegaly Splenomegaly Tonsillar hypertrophy Corneal opacity Kidney failure | Rule out secondary causes Clinical chemistry tests Molecular diagnosis | Manage secondary causes |
| Hypocholesterolaemia | LDL-C<50mg/dl | Malabsorption Steatosis | Rule out secondary causes Clinical chemistry tests Molecular diagnosis |
CHD: coronary heart disease; CVRF: cardiovascular risk factors; FH: familial hypercholesterolaemia; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; Lp(a): lipoprotein(a); PAD: peripheral artery disease; TC: total cholesterol; Tg: triglycerides.
Over the last 20 years, LUs have become an increasingly important part of Spain's health system, playing a prominent role in both Primary Care and Specialist Medicine.1 The SEA currently has more than 70 lipid units throughout the country. Their prominence in the healthcare setting has been consolidated thanks to the key role they play in three vital areas: care, teaching and research. In terms of care, the specialisation of LUs facilitates the diagnosis, management and specialised treatment of all clinical problems associated with overall cardiovascular risk. Such conditions include genetic or primary dyslipidaemia, secondary dyslipidaemia, treatment-resistant complex dyslipidaemia, treatment intolerance (myalgia, elevated transaminases), patients with atherosclerosis with no obvious risk factors and patients with premature cardiovascular disease.2 LUs also offer added value to the way in which the management of these health issues is approached, thanks to the physician's knowledge on everything to do with prevention: identification of family members with genetic hyperlipidaemia; overall cardiovascular risk assessment; lifestyle assessment and management; and assessment and follow-up of populations that are difficult to treat from a clinical perspective (children, pregnant women, etc.). Less relevant to the subject of this article, but no less important, is the role LUs play in teaching and research. Within the latter, networking among the various LUs should be noted, such as in the creation of dyslipidaemia registries,3 the significant number of scientific articles published in prestigious journals, their contribution to the greater understanding of dyslipidaemia and atherosclerosis, their collaboration in clinical trials and their conduct of important multi-centre projects. A survey to ascertain the needs, resources and scientific-technical production of the SEA was completed by several lipid units in 2017 (SEA 360° Project, data not published). It found that over the last five years, on average the LUs published nine original articles in international journals and contributed to 11 communications at international conferences. Finally, their recent innovative role within the development of concepts like “digital health”4 and “digitalisation”, and the difference that this will make to patients and medical professionals alike, is also worthy of mention.5 In fact, the doctor-patient relationship is undergoing significant changes as patients are increasingly using information and communication technologies to manage their health.
In short, networking, collaborating with national and international groups, the rise of clinical–experimental LUs with their own research laboratories and a wealth of experience accrued over a number of years make LUs the clinical unit par excellence for patients with dyslipidaemia in Spain.
What kinds of patient are referred to Spanish Atherosclerosis Society Lipid Units?In our setting, there is very little information available concerning the types of patient and conditions referred to LUs. A study by Mauri et al.,6 conducted in 10 LUs in Catalonia, Spain, recorded a total of 148 new patients and found the most common diagnosis to be familial hypercholesterolaemia, followed by mixed hyperlipidaemia. Some 53% of the patients were referred from Primary Care, with the remainder coming from Endocrinology (23%), Cardiology (17%), Internal Medicine (15%), Gastroenterology (14%), Neurology (13%), Gynaecology (9%), Angiology-Vascular Surgery (7%) and General Surgery (2%). A more recent study conducted by the SEA found that more than 50% of the LUs did not have locally-established referral criteria, and that most patients were referred from Primary Care and Cardiology (SEA 360°, data not published).
Referral due to hypercholesterolaemiaAll the documents consulted in the preparation of these criteria agree that the mere suspicion of familial hypercholesterolaemia is sufficient to refer patients to a specialist unit. For clinicians, the prior history, signs and symptoms that would support such a diagnosis are a history of early coronary heart disease in the family, cholesterol deposits (arcus senilis, xanthomas) and very high levels of total cholesterol and LDL cholesterol. There is little consensus on the levels of cholesterol required for a referral: some authors7 and health agencies8 recommended referring patients with total cholesterol levels >9mmol/l (>345mg/dl) or LDL cholesterol >7.5mmol/l (>290mg/dl). In Spain, while some agencies and scientific societies do not include cholesterol levels in their recommendations,9,10 others use the criteria of the CEIPC (Comité Español Interdisciplinario para la Prevención Cardiovascular [Spanish Interdisciplinary Committee for Cardiovascular Disease Prevention]), which recommend total cholesterol levels >400mg/dl and LDL cholesterol >260mg/dl.11
Lipoprotein a [Lp(a)] deserves special mention: it is well known that high levels of this lipoprotein increase the risk of suffering an ischaemic event, particularly in subjects with familial hypercholesterolaemia.12 Epidemiological studies conducted in Denmark found that the risk of vascular disease increases two-and-a-half-fold when Lp(a) levels are greater than 117mg/dl (p95),13 hence why we have chosen this cut-off point for patient referral to a LU, despite the fact that the only treatment currently available to reduce these levels is LDL apheresis.14
Referral due to hypertriglyceridaemiaThere is consensus amongst all of the guidelines that patients with fasting triglyceride levels >1000mg/dl, defined as severe hypertriglyceridaemia, should be referred to specialist units. Although most of these patients have hyperlipoproteinaemia type 5, and this phenotype is associated with environmental factors like alcohol consumption, type 2 diabetes, central obesity, oestrogen or pregnancy, in some cases these individuals are carriers of monogenic diseases that require molecular or biochemical diagnosis. The clinical context in these circumstances is the manifestation of eruptive xanthomas, abdominal pain and/or acute pancreatitis, lipaemia retinalis and frequent onset in childhood. Some guidelines and experts recommend referring patients to LUs with persistent triglyceride levels >500mg/dl despite appropriate treatment. Referral is also considered justified in patients with both high total cholesterol levels and triglycerides >350mg/dl. If a secondary cause is ruled out, such findings could be indicative of combined familial hyperlipidaemia15 or dysbetalipoproteinaemia,16 both associated with a high degree of atherogenic risk and which require diagnostic procedures that only specialist laboratories can provide.
Referral due to HDL cholesterol anomaliesBecause very low levels of HDL cholesterol have been epidemiologically associated with a greater risk of vascular disease, clinicians have become particularly vigilant. Low HDL cholesterol levels are often associated with hypertriglyceridaemia and metabolic syndrome. Levels can be extremely low in very rare cases. It is recommended to refer both male and female patients with HDL cholesterol levels <20mg/dl, as such low levels increase the likelihood of monogenic diseases, like Tangier disease, LCAT deficiency or apoA1 deficiency.17
High HDL cholesterol concentrations, which tend to be associated with a lower cardiovascular risk, have merited very little clinical study. However, recent data from population studies suggest that high and extremely elevated levels of HDL cholesterol are associated with a greater risk of cardiovascular and non-cardiovascular death.18,19 In light of this new epidemiological evidence, some patients with very high HDL cholesterol may be referred to a LU for study. The Denmark study identified HDL cholesterol levels >100mg/dl in men and 113mg/dl in women to have the greatest risk.18 The approach adopted by Spanish LUs with regard to hyperalphalipoproteinaemia will be to rule out any secondary causes and to investigate the monogenic diseases responsible for this phenotype.20
HypocholesterolaemiaAlthough not a common occurrence, patients with very low cholesterol levels (if not receiving a lipid-lowering treatment) are sometimes referred to a LU. These patients should be referred for further study once the most common causes have been ruled out, such as neoplasia, hormonal abnormalities, malnutrition, depression, HIV infection, etc. Having ruled out the above, the most common causes are hypobetalipoproteinaemia, due to APOB gene mutations that give rise to a truncated protein,21,22 or, in exceptional cases, PCSK9 loss-of-function mutations23 or angiopoietin-like 3 mutations.24 In hypobetalipoproteinaemia, which is relatively more common, the clinical context comprises an asymptomatic patient with possible clinical chemistry results suggestive of hepatic steatosis and, only in cases where apoB is shorter than B48, steatorrhoea may also be associated.
Special clinical situationsSome prevalent diseases in the general population that are characterised by high inflammation and vascular risk, such as rheumatoid arthritis and psoriasis,25 are associated with dyslipidaemia and often referred to LUs. Similarly, suspected adverse reactions to statins and hypertransaminasaemia, which is often associated with hepatic steatosis, also tend to be referred.
Conflicts of interestThe authors declare that they have no conflicts of interest.
The authors would like to thank Dr X. Pintó, Dr J. Ascaso, Dr J. Mostaza, Dr E. Ros and Dr L. Masana for their critical review of the original draft.
Emilio Ros (Barcelona), Sergio Martínez (Valencia), Ana Cenarro (Zaragoza), Miguel Ángel Sánchez (Malaga), Daiana Ibarretxe (Reus), Manuel Suárez (A Coruña), Ovidio Muñiz (Seville), Pablo Pérez (Cordoba), Agustín Blanco (Madrid), Angela Vea (Hospitalet de Llobregat), Rocio Toro (El Puerto de Santa María), Enric Serra (Igualada), Manuel Jesus Romero (Huelva), Carmen Rodriguez (San Fernando), Anna Pardo (Barcelona), Laura Márquez (Seville), Alberto de los Santos (San Fernando), Miguel Ángel Corrales (Malaga), Assumpta Caixàs (Sant Quirze del Vallès) and Marta Bueno (Lleida).
Please cite this article as: Sánchez-Chaparro MÁ, Pérez-Martínez P, Ibarretxe D, Suárez-Tembra M, Valdivielso P, en nombre del Grupo de Trabajo de las Unidades de Lípidos de la SEA. Criterios de derivación para pacientes a las unidades de lípidos de la Sociedad Española de Arteriosclerosis. Clin Investig Arterioscler. 2019;31:26–30