Non-alcoholic fatty liver disease (NAFLD) comprises a series of histologically lesions similar to those induced by alcohol consumption in people with very little or no liver damage. The importance of NAFLD is its high prevalence in the Western world and, from the point of view of the liver, in its gradual progression from steatosis to steatohepatitis, cirrhosis, and liver cancer. During the last decade it has been observed that NAFLD leads to an increased cardiovascular risk with acceleration of arteriosclerosis and events related to it, being the main cause of its morbidity and mortality. This review, updated to January 2016, consists of two parts, with the first part analysing the association of NAFLD with cardiovascular disease.
La enfermedad del hígado graso no alcohólico (EHGNA) comprende una serie de lesiones hepáticas histológicamente similares a las inducidas por el alcohol, en personas con un consumo del mismo muy escaso o nulo. La importancia de la EHGNA radica en su alta prevalencia en el mundo occidental y, desde el punto de vista hepático, en su progresiva evolución desde esteatosis a esteatohepatitis, cirrosis y cáncer de hígado. Durante la última década se ha observado que la EHGNA da lugar a un incremento del riesgo cardiovascular con aceleración de la arteriosclerosis y de los eventos a ella vinculados, principal causa de su morbimortalidad. Esta revisión actualizada a enero de 2016 consta de dos partes, analizando en esta primera parte la asociación de la EHGNA con la enfermedad cardiovascular.
Non-alcoholic fatty liver disease (NAFLD) covers a variety of histological lesions similar to those caused by alcohol abuse but without the consumption of alcohol, or with a consumption of less than 30–40mg/day for men, and less than 20mg/day for women. Simple steatosis is defined as a triglyceride deposit in the hepatocytes that is greater than 5% of the cellular weight, although from a practical point of view this diagnosis is made if more than 5% of the hepatocytes contain typically macrovesicular fat.1 If the disease progresses, the phenomena of hepatocellular ballooning and necrosis, as well as infiltration by inflammatory cells and fibrosis of the hepatic tissue are included in the histological spectrum, giving rise to non-alcoholic steatohepatitis (NASH). While only a small percentage of simple steatosis evolves into more severe advanced forms, the cirrhosis conversion rate for patients suffering from NASH is 25–30% within 4 years.2 Likewise, between 7% and 15% of those suffering from NASH or cirrhosis develop hepatocellular carcinoma.3,4
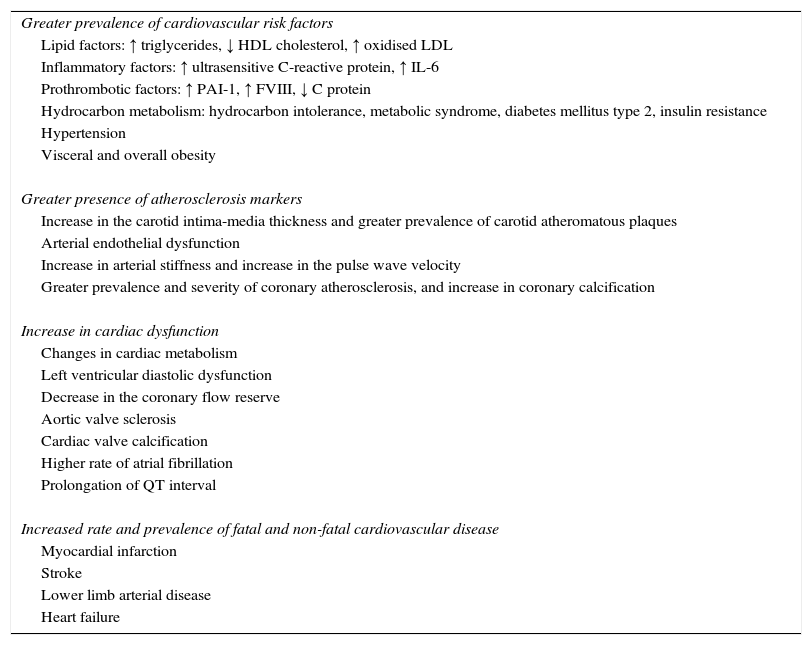
In the last decade, numerous tests in which NAFLD is linked with a greater risk of cardiovascular disease (CVD), which is the main cause of death in patients with NAFLD, have been added to the current evidence, displacing the old idea that hepatic steatosis is an innocuous disease (Table 1). It is estimated that in Europe the prevalence of NAFLD is between 2% and 44% of the general population5,6 and 26% in Spain.7 Given its association with excess weight and metabolic syndrome, growing problems that have reached epidemic proportions worldwide, it is expected that NAFLD will be an urgent public health issue in the not-too-distant future. This review will closely examine the relationship between NAFLD and CVD.
NAFLD is associated with a greater risk of cardiovascular disease.
| Greater prevalence of cardiovascular risk factors |
| Lipid factors: ↑ triglycerides, ↓ HDL cholesterol, ↑ oxidised LDL |
| Inflammatory factors: ↑ ultrasensitive C-reactive protein, ↑ IL-6 |
| Prothrombotic factors: ↑ PAI-1, ↑ FVIII, ↓ C protein |
| Hydrocarbon metabolism: hydrocarbon intolerance, metabolic syndrome, diabetes mellitus type 2, insulin resistance |
| Hypertension |
| Visceral and overall obesity |
| Greater presence of atherosclerosis markers |
| Increase in the carotid intima-media thickness and greater prevalence of carotid atheromatous plaques |
| Arterial endothelial dysfunction |
| Increase in arterial stiffness and increase in the pulse wave velocity |
| Greater prevalence and severity of coronary atherosclerosis, and increase in coronary calcification |
| Increase in cardiac dysfunction |
| Changes in cardiac metabolism |
| Left ventricular diastolic dysfunction |
| Decrease in the coronary flow reserve |
| Aortic valve sclerosis |
| Cardiac valve calcification |
| Higher rate of atrial fibrillation |
| Prolongation of QT interval |
| Increased rate and prevalence of fatal and non-fatal cardiovascular disease |
| Myocardial infarction |
| Stroke |
| Lower limb arterial disease |
| Heart failure |
The surrogate markers of atherosclerosis include arterial damage and the possibility of it developing into a symptomatic cardiovascular event. We will review the influence of NAFLD on these markers below.
Carotid ultrasoundNAFLD is associated with an early increase in the carotid intima-media thickness (IMT) and a greater prevalence of plaques, as was initially demonstrated by our group in patients of both sexes.8 Other cohort and population studies have ratified these findings.9–12 In a meta-analysis of all these studies, it was found that NAFLD is linked to an increase of 51–144% in the carotid IMT and that the presence of atheromatous plaques is 2–3 times greater.13 It was concluded that all patients with NAFLD should be evaluated using a carotid ultrasound.13 Another meta-analysis confirmed that NAFLD diagnosed using an ultrasound is associated with the presence of 2.8 times more carotid plaques, and 4.41 times more if diagnosed through a biopsy.6
The severity of the histologic lesion is correlated with the increase in the IMT, which is concordant with the fact that the patients with NASH have an increased cardiovascular risk (CVR) than those with simple steatosis.10 In fact, with hepatic fibrosis the IMT is much greater.14 Fracanzani et al. evaluated the risk factors that affect the progression of the IMT in patients with NAFLD and the CVD rate after more than 10 years of follow-up. In this period, the IMT of the patients with fatty liver was greater than that of the controls and the development of plaques progressed faster. A higher number of cardiovascular episodes occurred in patients with steatosis compared to the control population, and in the multivariate analysis the presence of plaques and steatosis were the main predictors. The degree of steatosis and the levels of alanine aminotransferase (ALT) and γ-glutamyl transpeptidase (GGT) were higher in patients who suffered a cardiovascular episode. For the authors, these results confirm that NAFLD should be included in the CVRFs and that the IMT is useful in predicting future episodes. They also signal the need for an evaluation of patients in order to diagnose NAFLD and the possibility of cardiovascular damage at an early stage.15
Finally, a pre-specified sub-study of the WELCOME trial16 was the first to show that when NAFLD improves, so does the IMT. This trial, which used a mix of omega-3 fatty acids ω(eicosapentaenoic [EPA] and docosahexaenoic [DHA]) at a dose of 4g per day for 18 months, showed that the improvement in the severity of NAFLD—expressed by the percentage decrease in liver fat, evaluated by nuclear magnetic resonance spectroscopy, and necroinflammation, evaluated according to cytokeratine-18 (CK-18) levels—was linked with a deceleration in the progression of the IMT. The ingestion of omega-3 did not affect the changes in the IMT. In the multivariate analysis, weight loss and an increase of DHA in the tissues was associated with a decrease in liver fat, but this was not the case with changes in the levels of CK-18.
Coronary angiographyThrough coronary angiography, it has been found that patients with hepatic steatosis have a higher prevalence and greater severity of coronary artery lesions after adjusting for other confounding factors.17–19 Similarly, this has been verified through computed tomography angiography, as NAFLD is associated with a more than threefold increase in the prevalence of ischaemic heart disease.6 Furthermore, the severity of the coronary artery calcium deposit (CAC) evaluated by angiography, which is associated with CAC scores greater than 100, increases independent of other CVRFs, including visceral adiposity.20 Moreover, there is a strong link between NAFLD and the presence of vulnerable plaques that increase the risk of serious cardiovascular episodes.21–23
Other markers: endothelial dysfunction and pulse wave velocityIt was verified that the patients with NAFLD suffer from endothelial dysfunction (measured by both brachial artery flow-mediated vasodilation and the presence of adhesion molecules), which is not dependent on obesity, or the presence of metabolic syndrome (MS), or any of its components.24,25 Patients with NAFLD also present an increased pulse wave velocity.26,27 A recent, extensive systematic review confirms the relationship between NAFLD and the subclinical atherosclerosis markers; 16 studies link it with an increase in the carotid IMT, seven with CAC, seven with endothelial dysfunction, and six with arterial stiffness. The studies showed significant increases in the carotid IMT among patients with NAFLD compared to the controls. These were independent of the traditional CVRFs and the MS components. The link was similar in the CAC studies, in which the presence of NAFLD was associated with the severity of the calcification. Endothelial dysfunction and arterial stiffness were significantly and independently linked to NAFLD, although in two studies limited to diabetic populations these were not significant. The authors concluded that there was sufficient evidence to support the link between NAFLD and subclinical atherosclerosis, independent of the traditional risk factors and MS. Nevertheless, they believe longitudinal studies need to be conducted to review this relationship in all ethnicities and determine its causality.28
Cardiac dysfunctionOther CVR detection techniques in asymptomatic people such as changes in the myocardial metabolism of the ATP, measured through a heart MRI with spectroscopy, have shown a greater prevalence of NAFLD anomalies.29,30
Patients with NAFLD also show signs of early left ventricular diastolic dysfunction, measured via a Doppler echocardiography, with there being a positive correlation between this dysfunction and the histologic severity.31
The presence of NAFLAD is, independent of other factors, associated with a reduction in the coronary flow reserve measured via echocardiography, which is notably decreased if there is fibrosis.32
Other cardiac disorders: aortic sclerosis in NAFLD, atrial fibrillation and prolongation of the QT interval.
Sclerotic valvular degeneration, especially of the aortic valve, is linked to the same CVRFs that occur in atherosclerotic coronary lesions.33 NAFLD is significantly linked to aortic sclerosis, independent of other CVRFs, in proportion to its ultrasonic severity assessment.34 Furthermore, in patients with type-2 diabetes, hepatic steatosis is a predictor, independent of the calcification of the mitral and aortic valves, which in turn predict a greater risk of cardiovascular episodes.35
Atrial fibrillation also seems to be linked to NAFLD. The cohort studies that used liver enzymes as NAFLD markers and those that used ultrasound to diagnose NAFLD have both shown that the presence of hepatic steatosis in patients, compared with people who do not suffer from a fatty liver, is independently linked with a greater risk of new-onset,36,37 greater persistent or permanent prevalence,38 and an increased likelihood of developing atrial fibrillation in follow-up periods of more than 10 years.39 This association between NAFLD and AF continues to be significant even after adjusting for the numerous arrhythmogenic risk factors.38,39 There also seems to be a relationship between the ultrasonic degree of severity of the NAFLD and the prolongation of the QT interval in diabetic patients, independent of other confounding factors.38,39
Non-alcoholic fatty liver disease and increased prevalence of CVDVarious studies have shown that patients diagnosed with NAFLD have a greater prevalence of coronary artery disease than the general population. The analysis of a Taiwanese cohort revealed that with an ultrasound consistent with steatohepatitis, the prevalence of ischaemic heart disease was higher, and that this relationship was independent of obesity and other prognostic factors.40 Wong et al., in Hong-Kong, through a coronary angiography, found that people with non-alcoholic fatty liver diagnosed using ultrasound have a greater risk of heart disease than those who do not suffer from steatosis.41 An Italian series involving diabetic patients produced similar results.42 It has also been verified that in patients with NAFLD and type-2 diabetes there is a greater prevalence, compared to the controls, of not only heart disease, but also cerebrovascular disease and peripheral artery disease, all independent of MS and its components.43,44 In patients with type-1 diabetes it was also observed that the presence of ultrasonic steatosis is linked to an eight-fold increase in the prevalence of CVD, defined as a combination of ischaemic heart disease diagnosed by electrocardiogram and clinical history, the results of a pathological carotid ultrasound, or the presence of peripheral artery disease in the lower limbs detected by Doppler ultrasound. The relationship is, once again, independent of the classic CVRFs, MS components and concomitant treatments.45 In a paediatric post-mortem examination series, the children who suffered from fatty liver had double the rate of coronary artery lesions.46 A meta-analysis of four studies using coronarography found that 80% of patients with NAFLD, compared to 60% in the controls, were identified as having heart disease, which is defined as the presence of plaques that lead to stenosis greater than or equal to 50%.6
In a review that included 3014 participants from the Framingham Heart Study, steatosis determined via ultrasound was significantly linked to the presence of CAC, while its link with CVD was close to the significance level (p=0.07), which was defined by the combined objective of prior fatal myocardial infarction, transitory/established ischaemic stroke, heart failure and peripheral artery disease.47
Non-alcoholic fatty liver disease and increase in the CVD rateSeveral studies show greater cardiovascular morbidity and mortality rates in patients with NAFLD than those who do not suffer from it, independent of the method used to diagnose said NAFLD.
Increase in liver enzymes and CVD rateIn studies where the increase in ALT or GGT, as secondary markers for NAFLD, were analysed, and which monitored large populations over periods of between 10 and 19 years, found that the patients with raised liver enzymes had higher rates of both CVD and CVD-related mortality compared to those who had normal levels, with this relationship being, for the most part, independent of other traditional factors, including age and weight.48–55 Furthermore, a meta-analysis showed that the increase in GGT in non-drinkers linearly increased the risk of ischaemic heart disease or stroke.56,57 However, it has not always been proven that the increase in liver enzymes is associated with increased CVR. As such, from the FIELD study data, Williams et al.,58 in their population, explain that lower levels of ALT predict an increased risk of a cardiovascular episode, and therefore, they could be a marker of systemic or hepatic fragility in patients with type-2 diabetes, instead of representing a healthy liver and the absence of NAFLD. For each decrease in the ALT in a standard deviation (−13.2U/L), an increase of 7% in the CVR was observed.
Non-alcoholic fatty liver disease diagnosed by ultrasound or biopsy and CVD rateIn the studies in which the presence of NAFLD was identified by a liver ultrasound, with a follow-up period of between 5 and 12 years, a higher rate of CVD was observed, with a five-fold increase in the percentage of recorded episodes.59–62
The liver biopsy is the most accurate procedure for diagnosing NAFLD. All the series that use this procedure3,63–68—except one69—found that in these patients, after an observation period of between 7.6 and 18 years, there was a decrease in the survival rate, the main reason for which was the increased rate of cardiovascular episodes and the increased cardiovascular mortality rate. Of the above publications, it is possible from the population cohort-based studies64–66 to define the relevance of the atherosclerotic morbidity and mortality rates as an element that shortens the life expectancy of those who suffer from this disease, even in diabetic patients.3 A meta-analysis2 confirms that NAFLD diagnosed by an ultrasound or a liver biopsy is linked with an overall risk of death that is 1.57 times greater than that of the general population. This risk mainly includes CVD, which, with a 2.05 times greater incidence rate, multiplies the risk of CVD-related death by 2.16. The patients most likely to die due to CVD are those between 45 and 55 years old, where the cardiovascular mortality rate and overall mortality rate is 8.15 and 4.4 times greater, respectively. In contrast with other studies, in this meta-analysis the cardiovascular mortality rate does not differ significantly between simple steatosis and NASH. Nevertheless, the physiopathological link between NAFLD and the cardiovascular mortality rate is clear when patients with cirrhosis as a result of NASH are compared with other cirrhotics infected with the hepatitis C virus. Although both have a similar hepatic mortality rate, the cardiovascular mortality rate at 10 years is 28% in the first group, while in the second it is under 2%.3 In another more recent meta-analysis the link between NAFLD and the risk of cardiovascular episodes was confirmed. In said analysis, NAFLD multiplied this risk by 1.5, independent of the concomitant treatments and MS and its components.70 In patients with a high degree of fibrosis, determined using scoring systems (NAFLD fibrosis score, Fibrosis-4 score), the probability of CVD triples, and can be up to 5 times more if they also develop type-2 diabetes.71,72
In 2015, around 20 retrospective or prospective studies were recorded that analysed the relationship between NAFLD and the risk of future cardiovascular episodes.73 The majority of these studies showed that NAFLD is associated with an increase in CVD mortality and morbidity rates, independent of the traditional CVRFs and MS. In these studies, it was observed that the overall and cardiovascular mortality rates are increasing, with the stage of fibrosis being the main predictor.74 Nevertheless, not all studies agree with the findings of this study. In the US National Health and Nutrition Examination Survey III, after a cohort follow-up period of between 14 and 17 years, no link between NAFLD and CVD was found,75 and if a link was found, this was associated with the risk of independently presenting a cardiovascular disease. There was no increase in the cardiovascular mortality rate, which was only observed in cases involving advanced fibrosis.76
Non-alcoholic fatty liver disease and calculation of cardiovascular riskThe quantification of CVR in patients with NAFLD is still a challenge. The traditional calculation tables and formulas were designed to evaluate CVR in individuals of the general population and, therefore, they may underestimate it in patients with NAFLD given that neither insulin resistance, nor hypertriglyceridemia, nor the subclinical inflammation present in this liver disease were taken into account in the CVR formulas. However, a recent longitudinal study of patients with NAFLD has validated Framingham's formula as a CVR predictor with a suitable level of accuracy in this population, advocating its use in stratifying the risk and guiding the treatment of the modifiable factors, including dyslipidaemia.77 Nevertheless, the lack of contrast between the results of this population and that of the control population who did not suffer from NAFLD limits the potential systematic use of the Framingham scale to evaluate the CVR in this liver disease.78 The QRISK2 algorithm may provide a slightly more accurate prediction of the risk in steatosic patients since its variables include obesity and diabetes.79
In order to be universally applicable, these prediction systems should be validated in the future through large-scale, prospective studies involving cohorts of patients with NAFLD.80
Some time ago, using the SCORE tables, our group showed that the majority of patients with NAFLD usually reach moderate or high CVR categories,81 which has been corroborated by larger, more recent studies.82–84 In these evaluations, the risk is also increased with the severity of the liver histology.82
ConclusionIn this updated review the evidence contributed by the studies evaluating the link between NAFLD and CVR and the structural or functional cardiac disorders was examined. The tests confirmed that there is a clear relationship between fatty liver and CVD, which is translated into an increase in the cardiovascular or overall morbidity and mortality rates. The causality of this phenomenon has still not been clarified as it must be verified through extensive, prospective, controlled trials and intervention studies. For clinical practice, recognising NAFLD as a CVD trigger or amplifier and before the chance detection of hepatic steatosis through a conventional ultrasound examination, the doctor should strive to explore the probable coexistence of underlying CVRFs. Control of these factors may prevent the possibility of a CVD event, unless this involves stopping the control of the possible progression of the liver disease.8,85,86
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were conducted on human beings or animals for this research.
Confidentiality of dataThe authors declare that no patient data is contained in this article.
Right to privacy and informed consentThe authors declare that no patient data is contained in this article.
Conflicts of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Brea Á, Pintó X, Ascaso JF, Blasco M, Díaz Á, González-Santos P, et al. Enfermedad del hígado graso no alcohólico, asociación con la enfermedad cardiovascular y tratamiento (I). Enfermedad del hígado graso no alcohólico y su asociación con la enfermedad cardiovascular. Clin Invest Arterioscler. 2017;29:141–148.