To determine the changes in the clinical and prognostic characteristics of patients admitted due to acute coronary syndrome (ACS) during the period between the years 2005 and 2015 in a provincial referral hospital.
Material and methodCross-sectional observational study was conducted comparing the characteristics of ACS between 2005 and 2015. An analysis was made of the cardiovascular risk factors, treatment at discharge, complications, and mortality.
ResultsThe incidence of ACS in 2015 was 15.3% lower. The incidence of hypertension, diabetes and dyslipidaemia was similar, but there were more smokers in 2015 (25.9% vs 18.3%, P = .005). Coronary reperfusion and the prescription of secondary prevention treatments increased compared to 2005. Hospital mortality was similar.
ConclusionThe incidence of ACS has decreased in the last decade, in parallel with an improvement in the prognosis related to a more frequent use of the treatments recommended in the guidelines.
Determinar el cambio en las características clínicas y pronósticas de pacientes ingresados por síndrome coronario agudo (SCA) durante un periodo de los años 2005 y 2015 en un hospital de referencia provincial.
Material y métodoEstudio observacional transversal que compara las características del SCA de los años 2005 y 2015. Se analizaron factores de riesgo cardiovascular, tratamientos al alta, complicaciones y mortalidad.
ResultadosLa incidencia de SCA en 2015 fue un 15,3% menor. La incidencia de hipertensión arterial, diabetes y dislipemia fue similar, pero hubo más fumadores en 2015 (25,9% vs 18,3%; P = 0,005. La reperfusión coronaria y la prescripción de tratamientos de prevención secundaria aumentaron respecto a 2005. La mortalidad hospitalaria fue similar.
ConclusiónLa incidencia de SCA ha disminuido en la última década en paralelo a una mejoría en el pronóstico relacionado con un uso más frecuente de los tratamientos recomendados en las guías.
Acute coronary syndrome (ACS) is the most common manifestation of heart disease (HD) and one of the main causes of morbidity and mortality, and healthcare expense in Spain.1 The changes in clinical management and treatment that have been included in clinical practice guidelines in recent years2,3 warrant the collection of updated information on the prognosis and management of ACS to thus compare it with previous data that provide information on the evolution over time of our clinical practice.
Our aim was to determine the change in clinical characteristics, management and hospital mortality of patients admitted due to ACS over a period of 6 months in 2005, and over the same period in 2015 in a provincial referral hospital in our setting.
Patients and methodsA cross-sectional observational study that included all consecutive patients admitted to our hospital with an established diagnosis of ACS in two specific time periods: from April 1 to September 30 (6 months) of 2005 and 2015. Evolution was recorded on admission.
ACS was defined as the elevation of myocardial damage marker enzymes above the normality limit in the centre’s laboratory (troponin I ≥ .04 ng/dl or ultrasensitive Troponin T > 14 ng/l) and/or alterations on the electrocardiogram indicating injury or myocardial ischaemia accompanying compatible chest pain.2,3
Risk factors, history, clinical presentation of ACS, treatments used and the main complications during the hospitalisation phase were recorded in all patients.
Continuous variables are described as means ± SD and categorical variables as percentages. We used the Student t-test to compare continuous variables and the χ2 test to compare categorical variables. Predictors of hospital mortality were studied by multivariate analysis. The analyses were performed with SPSS13.0.
ResultsFrom 2005 to 2015, there was a 15.3% reduction in the incidence of ACS (196 cases in 2005 and 166 in 2015).
With regard to the type of ACS, in 2005 there was 36.7% of ACSSTE compared to 63.3% of ASCWSTE (not taking unclassifiable ACS into account, which was included under ASCWSTE), and in 2015 41.6% of ACSWSTE, 51.8% of ACSSTE and 6.6% of unclassifiable ACS.
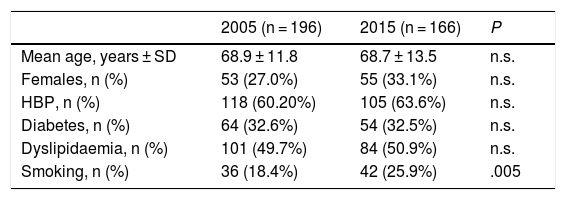
The percentage of women and age of presentation of ACS were similar in both periods, and in terms of cardiovascular risk factors (CVRF) there was a higher percentage of smokers in 2015 (25.9% vs 18.3%; P = .005), but high blood pressure, hyperlipidaemia and diabetes were similar (Table 1).
General characteristics of the patients of both registers.
| 2005 (n = 196) | 2015 (n = 166) | P | |
|---|---|---|---|
| Mean age, years ± SD | 68.9 ± 11.8 | 68.7 ± 13.5 | n.s. |
| Females, n (%) | 53 (27.0%) | 55 (33.1%) | n.s. |
| HBP, n (%) | 118 (60.20%) | 105 (63.6%) | n.s. |
| Diabetes, n (%) | 64 (32.6%) | 54 (32.5%) | n.s. |
| Dyslipidaemia, n (%) | 101 (49.7%) | 84 (50.9%) | n.s. |
| Smoking, n (%) | 36 (18.4%) | 42 (25.9%) | .005 |
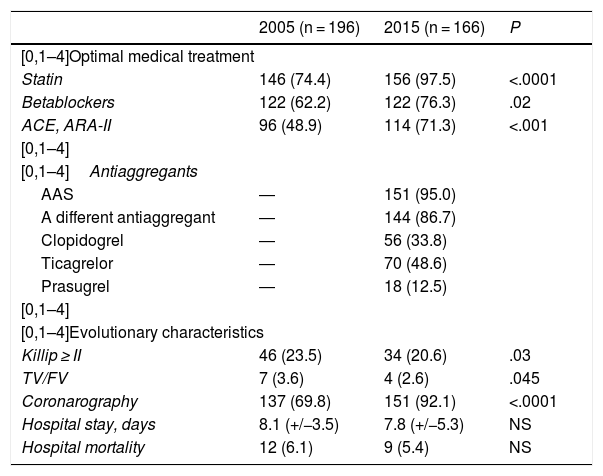
The use of medical treatment as recommended by clinical practice guidelines (statins, beta-blockers, and renin-angiotensin system inhibitors2,3 was significantly higher in 2015 than in 2005; the rate of double antiaggregant treatment was very high in 2015, but we have no data from 2005 to compare (Table 2). A much higher percentage of patients underwent coronary angiography in 2015 (Table 2), and more patients received reperfusion treatment: percutaneous treatment by angioplasty was performed in 44.5% in 2005 and 71.5% in 2015 (P = .001) and 6.3% were referred for surgery in 2005 and 4.3% in 2015 (P = n.s.). With respect to ASCWSTE, the rate of relapsed patients was 56.9% in 2005 and 86.7% in 2015. In 2015 there were fewer complications such as heart failure and malignant ventricular arrhythmias (Table 2).
Use of recommended drugs in ACS and evolutionary characteristics.
| 2005 (n = 196) | 2015 (n = 166) | P | |
|---|---|---|---|
| [0,1–4]Optimal medical treatment | |||
| Statin | 146 (74.4) | 156 (97.5) | <.0001 |
| Betablockers | 122 (62.2) | 122 (76.3) | .02 |
| ACE, ARA-II | 96 (48.9) | 114 (71.3) | <.001 |
| [0,1–4] | |||
| [0,1–4]Antiaggregants | |||
| AAS | ― | 151 (95.0) | |
| A different antiaggregant | ― | 144 (86.7) | |
| Clopidogrel | ― | 56 (33.8) | |
| Ticagrelor | ― | 70 (48.6) | |
| Prasugrel | ― | 18 (12.5) | |
| [0,1–4] | |||
| [0,1–4]Evolutionary characteristics | |||
| Killip ≥ II | 46 (23.5) | 34 (20.6) | .03 |
| TV/FV | 7 (3.6) | 4 (2.6) | .045 |
| Coronarography | 137 (69.8) | 151 (92.1) | <.0001 |
| Hospital stay, days | 8.1 (+/−3.5) | 7.8 (+/−5.3) | NS |
| Hospital mortality | 12 (6.1) | 9 (5.4) | NS |
VT/VF: ventricular tachycardia/ventricular fibrillation.
The mean LDL cholesterol (LDLc) tested on admission was 112.0 ± 32.6 mg/dl in 2005, while in 2015 it was 83.5 ± 33.0 mg/dl.
Hospital mortality was 6.1% in 2005 and 5.4% (7.9, 1.6 and 18.2% for ACSWSTE, ACSSTE and undetermined ACS, respectively) in 2015 (P = n.s.). The predictors of hospital mortality in all the patients from both registers in the multivariate analysis were age (odds ratio = 1.1; 95% confidence interval [CI95%]: 1.03–1.14), a Killip grade higher than I (odds ratio = 4.62; 95% CI: 4.12–7.58), the use of beta-blockers (odds ratio = .84; CI95%: .47–.95) and performing a coronary angiography (odds ratio = .73; 95% CI: .56–.99).
DiscussionWe noted a 15.3% decrease in the incidence of ACS in 2015 compared to the same period in 2005, while the population in our province in that period has remained constant, with a minimum decrease of 1.53%. It is known that the ACS incidence rates in Spain have been progressively reducing since 2005: discharges with a diagnosis of HD decreased from 146,809 in 2005 to 120,334 in 2015, 18% less.4
The two studies analogous to ours carried out in Spain are the MASCARA register, conducted in 2004–2005, and the DIOCLES register, in 2012.5,6 The characteristics of the population are very similar to those of previous studies, with an average age similar to the DIOCLES study and slightly lower than that of MASCARA.5,6
The age of presentation and the distribution by sex was similar in both periods of analysis; the classical CVRFs were similar, except for a higher percentage of smokers in 2015. Also in the MASCARA register smoking is somewhat lower than that described in the DIOCLES register a decade later.5,6 Improvements in the treatment of chronic HD and in the control of CVRFs in general have probably led to a decrease in the incidence of ACS over the last decade, but smoking may have gained much more weight than other CRFs as a pathogenic factor of ACS, since it is also often associated with other lifestyle changes that interact to favour a particularly atherogenic lipid profile (low HDL cholesterol and small, dense LDLc particles) and increased insulin resistance.
As in the MASCARA and DIOCLES registers,5,6 ACSSTE was the most frequent presentation; the patients on the register who underwent coronary angiography during admission increased from 69.8% in 2005 to 92.1% in 2015. The rate of angioplasty also increased (from 44.5% to 71.9%) in the two time periods studied, while the rates of surgical revascularisation were similar and remained relatively low. This increase in the number of percutaneous interventions does not surprise us, since our hospital’s haemodynamics theatre began operation in December 2005. It is logical that, following its implementation and the start of the primary angioplasty programme, the number of procedures has increased substantially. However, it was only in October 2018 that the infarction code was established in our autonomous community.
In 2015 compared to 2005 there was a significant increase in the prescription of beta blockers, renin-angiotensin system inhibitors and statins on discharge; here too the data from the MASCAR A5 register are similar to our 2005 data and the DIOCLES register shows results similar to ours in 2015.6
Complications such as heart failure and ventricular arrhythmias were less frequent in the 2015 register, probably in relation to the greater number of reperfusions performed in this period.
The decrease in mean LDLc levels of almost 30 mg/dl in 2015 compared to 2005 is indicative of greater awareness of physicians in the control of hyperlipidaemia and improved implementation of clinical practice guidelines in both primary and secondary prevention. In 2004 the National Cholesterol Education Programme (NCEP) Adult Treatment Panel III (ATP-III) published an update of the 2001 ATP-III guidelines, which already, for the first time, recommended achieving a target LDLc lower than 70 mg/dl.7
Hospital mortality due to ACS decreased in the period 2005 to 2015, and the failure to achieve statistical significance could be due to the small sample size. In the DIOCLES register, which collects data from 2012, hospital mortality due to ACS was 4.1%, somewhat lower than that of our 2015 register, although, as the authors themselves acknowledge, there may be an inclusion bias due to the inclusion of patients with suspected ACS, and therefore in the end 9% did not have ACS.5 All the patients included in our register were diagnosed with ACS, regardless of the initial admission department (ICU, cardiology, internal medicine, geriatrics or the emergency department). Overall, the independent factors related with better prognosis are the lower incidence of heart failure, the use of drugs recommended in the guidelines and the generalisation of coronary artery disease, which results in greater use of coronary reperfusion techniques.
The main limitation of our register is the small sample size, which is due to the characteristics of our hospital and the health area it serves.
ConclusionsThe incidence of ACS has reduced in the past decade in parallel with an improvement in prognosis related to more frequent use of the treatments recommended in the clinical practice guidelines, principally coronary reperfusion and the recommended optimal medical treatment.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Gómez-Barrado JJ, Ortiz-Cortés C, Gómez-Turégano P, Lezcano-Gort LE, Kounka Z, Romero-Castro MJ. Cambios en el síndrome coronario agudo en una década en un hospital de referencia provincial. Clin Investig Arterioscler. 2019. https://doi.org/10.1016/j.arteri.2019.07.001