To know the epidemiological, clinical and therapeutic characteristics of patients with a diagnosis of HF treated in primary care of two Health Areas of Albacete, Zone 5 A (characteristics of the Urban Center) and Casas Ibañez (characteristics of the Rural Center) as well as to highlight The main differences between the two.
MethodDescriptive and cross-sectional study, corresponding to the first phase of the ALBAPIC study. All patients in the area who met the inclusion criteria have been registered: Having a diagnosis of HF in the TURRIANO programme (consultation programme in Primary Care of Castilla la Mancha).
Demographic-anthropometric and clinical characteristics, analytical data, complementary diagnostic examinations, therapeutic guidelines and hospitalizations were recorded for 12 months prior to inclusion. A physical examination and electrocardiographic and biochemical controls were performed at the inclusion visit.
Results384 patients diagnosed with HF in both Health Zone (161 in urban areas and 223 in rural areas) have participated. Average age 82.24 +/− 10.51 years (81.24 +/− 9.59 years in urban areas and 83.37 +/− 11 years in rural areas with significant differences p < 0.005, 54.3 are women % (54% in urban areas and 54.7% in rural areas) We have an incidence of CI of 1% in urban areas and 1.8% in rural areas.
The prevalence of CVRF has that Hypertension above all and dyslipidemia are the most frequent, with differences depending on the environment in which they live.
In the rural environment there are higher rates of heart disease.
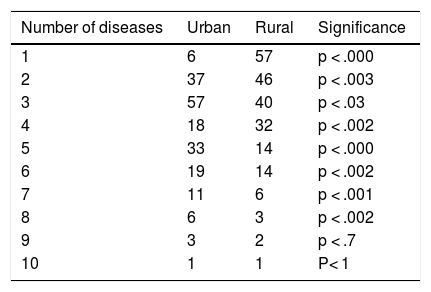
Patients with HF have a high number of concomitant chronic diseases, being between 4 and 6 > 60% of cases in the urban environment and between 1 and 4 in the rural environment.
Approximately 14% also have an oncological disease in the urban environment compared to 21% in the rural.
According to the exploration and analytical data, the main variables are acceptably controlled, the lipid parameters in the rural centre being worse controlled.
The average number of drugs prescribed by each patient was 6.3 in rural and 7.2 urban. As for the treatments they are taking, it is observed that diuretics and statins.
ConclusionsThere is an acceptable control of cardiovascular risk factors in both media, there being differences in the diagnostic methods and treatments used.
Conocer las características epidemiológicas, clínicas y terapéuticas de los pacientes con diagnóstico de IC atendidos en atención primaria de dos Zonas de Salud de Albacete, Zona 5 A (características de Centro urbano) y Casas Ibañez (características de Centro rural) asi como destacar las principales diferencias entre ambos.
MetodoEstudio descriptivo y transversal, correspondiente a la primera fase del estudio ALBAPIC. Se han registrado a todos los pacientes de la zona desde el 1 de Enero de 2018 hasta el 30 de Junio 2019 que cumplieran el criterio de inclusión: Tener diagnóstico de IC en el programa TURRIANO (programa de consulta clinica en Atención Primaria de Castilla la Mancha).
Se registraron las características demográfico-antropométricas y clínicas, los datos analíticos, las exploraciones diagnósticas complementarias, las pautas terapéuticas y las hospitalizaciones durante 12 meses previos a la inclusión. Se realizaron una exploración física y controles electrocardiográficos y bioquímicos en la visita de inclusión.
ResultadosHan participado 384 pacientes diagnosticados de IC en ambas Zona de Salud (161 en zona urbana y 223 en la rural). Edad Media 82,24+/-10,51 años (81,24+/-9,59 años en zona urbana y 83,37+/-11 años en rural con diferencias significativa p < 0,005, son mujeres un 54,3% (54% en zona urbana y 54,7% rural). Tenemos una incidencia de IC de 1% en medio urbano y 1,8% en medio rural.
La prevalencia de FRCV tenemos que la Hipertensión sobre todo y las dislipemias son los más frecuentes, existiendo diferencias según el medio en el que viven.
En el medio rural hay mayores tasas de Cardiopatías (principalmente isquémicas y por valvulopatía).
Los pacientes con IC tienen número alto de enfermedades crónicas concomitantes, siendo entre 4 y 6 más del 60% de los casos en el medio urbano y entre 1 y 4 en el medio rural.
Aproximadamente un 14% tienen también una enfermedad oncológica en el medio urbano frente a un 21% en el rural.
Según los datos de exploración y analítica las principales variables se encuentran aceptablemente controladas, estando peor controlados los parámetros lipídicos en el centro rural.
La media de fármacos prescritos por cada paciente fue de 6,3 en rural y 7,2 urbano. En cuanto a los tratamientos que están tomando se observa que los diuréticos y las estatinas son los más utilizados tanto en el medio rural como urbano.
ConclusionesExiste un aceptable control de los factores de riesgo cardiovascular en ambos medios, existiendo diferencias en cuanto a los métodos diagnósticos y tratamientos utilizados.
Heart failure (HF) is a major public health problem, and is largely responsible for the high rates of cardiovascular morbimortality which are the major cause of death in Western countries.1
In developed countries approximately 2% of the adult population presents with HF, a prevalence which increases exponentially with age, since it is under 1% before 50 years of age and later doubles with every decade, reaching up to 8% among those over 75.2 The high number of cases of HF in Spain is essentially determined by the progressive ageing of the population.3–5
HF is the primary cause of hospitalisation among the geriatric population6–9 and the third cause of cardiovascular death, after ischaemic heart disease and stroke.7,8 Mortality is 50% at 5 years6,9,10 and the frequency of hospital re-admittance is approximately 30% during the first 6 months.11–13
In one primary care study,14 it was observed that HF affects the quality of life of the individual more than any other chronic disease, observing that mortality in severe HF is worse than that of the most common cancers. 6,7,15
Improvements in cardiovascular disease treatment lead to greater survival of patients with ischaemic heart disease. This, together with an ageing population, and an increase in obesity and type 2 diabetes suggests that the rate of HF will increase and with it, medical care costs, disability and impairment in the quality of life.
The impact of HF requires innovative and cost effective strategies which should involve primary health care (PHC) in HF management, with consultation from specialists. This is because they have greater knowledge regarding the population they serve, and their cultural, social and economic differences. Also this is the health area which is capable of involving the population actively in the planning and control of their own disease for greater efficacy of control.16–19 It should also be considered that prevention is priority for PHC20 physicians and they should therefore be aware of the social factors that condition the disease. This line of thought takes us again to the PHC professional, as the main health agent in the management of HF. Due to its chronicity it requires continuous and comprehensive care, supported by the right consultations and guidance from the Cardiology or Internal Medicine specialist. This is in keeping with the situation in other countries, including the United Kingdom, where most patients with HF are treated by their GP.21 HF therefore requires control in its management and follow-up and coordination between the PC and Cardiology departments, and even Internal Medicine and Hospital emergency departments.22–24
Moreover, this care quality may be different in urban areas, with close hospitals and greater accessibility of specialists (Cardiology or Internal Medicine), than in rural areas, with less availability of doctors and additional diagnostic tests and treatment.
Other studies have already demonstrated that the use of cardiovascular medication is lower in rural areas and in populations with lower economic resources. Much disparity exists regarding life style habits and a healthy diet between rural and Urban areas.25,26
New technologies are now able to provide the means to rectify this inequality.27 Thus, researchers from the Hospital Universitario Charité of Berlin (Germany) have shown in the TIM study, published in The Lancet, that the use of telemedicine (TM) reduces hospital stays and prolongs the life of patients with HF, in both rural and metropolitan areas: 1538 patients with chronic HF (CHF), in a randomised study with participation from cardiologists and GPs were to receive regular treatment or intervention by TM. Hospital admissions were reduced from 24.2–17.8 days whilst the death rate dropped from 11 to 8.28,29
Therefore, apart from improving the general quality of medical care, TM may serve as a compensatory strategy for the difference between rural and urban areas, which are principally due to the lack of physicians.22 Telemonitoring of patients, the presence of symptoms and signs, electronic transfer of physiological data (electrocardiography, blood pressure, weight, pulse oximetry, and breathing rate) together with adherence to medication is a way in which people with HF may be controlled from a distance by their doctors synchronously and, asynchronously.28
Despite the fact the first trials applying telemonitoring in HF were carried out over 15 years ago, meta-analysis and systematic reviews such as that by Cochrane23–26,28 conclude that TM in HF:
- -
Reduces the use of health services.
- -
Improves health outcomes.
- -
Improves health-related quality of life (QoL).
- -
Increases patient satisfaction.
- -
Reduces mortality from all causes.
- -
Reduces HR-associated hospitalisations.
Results vary extensively because outcomes come from trials of variable quality, often with insufficient specification of the TM interventions adopted and therefore little discussion on the intervention itself, which is essential. On other occasions the level of the patients’ treatment adherence is not sufficiently specified over the study period.25,26,28,29 As a result, the European Society of Cardiology30 considers that the development of assessment criteria of electronic tools is a critical step.
We therefore conducted the ALBAPIC (for its initials in Spanish) heart failure in primary care in Albacete study, the first phase of which is presented in this article and which aimed to determine the epidemiological, clinical and therapeutic characteristics of patients diagnosed with HF attended in PC centres in 2 health areas of Albacete, Area 5 A (urban centre characteristics) and Casas Ibáñez (rural centre characteristics) and to highlight the main differences between the two. In the second phase we will proceed to the designing of a specific intervention in TM for this rural population aime at assessing not only clinical impact but also the impact on the patient’s quality of life, the professionals’ convenience and its cost effectiveness for the health system.
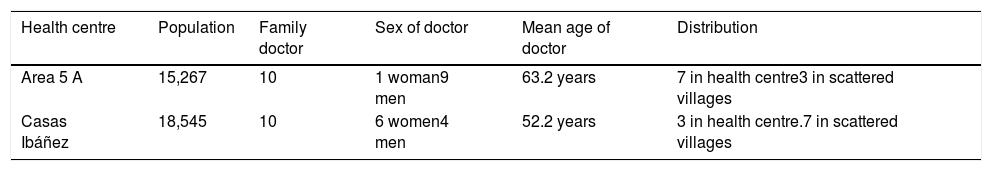
MethodStudy protocolAll the PC doctors of basic areas participated. The areas were dividied between 10 clinics in local rural medical practices and 10 clinics in urban health centres (HC), depending on the population and as a representative sample of the rural and urban area of Albacete. Casas Ibáñez with a population of 15,000 quite elderly inhabitants was divided into small population nuclei, and met with the characteristics of a rural population. HC area 5 A of Albacete was in an urban location and attended a population of 18,000 inhabitants (Table 1).
Distribution and characteristics of physicians in both health centres.
| Health centre | Population | Family doctor | Sex of doctor | Mean age of doctor | Distribution |
|---|---|---|---|---|---|
| Area 5 A | 15,267 | 10 | 1 woman9 men | 63.2 years | 7 in health centre3 in scattered villages |
| Casas Ibáñez | 18,545 | 10 | 6 women4 men | 52.2 years | 3 in health centre.7 in scattered villages |
All patients in the area who met with the inclusion criteria were registered. They had been given a diagnosis of HF, between 1 st January 2018 and 30th June 2019 in the TURRIANO programme (consultation programme in Primary Care of Castilla-La Mancha), which records the daily activity of family physicians and the CIE-10 diagnosis data. This was later correlated with the basic minimum aggregate data base of the Albacete Comprehensive Care Management.
Data were collected from the clinical file and in the actual medical practice, through an interview with the patient using an adhoc questionnaire designed for the study. The variables measured were socio-demographic (origin, age, sex), the aetiology of the CHF, comorbidities (any other chronic disease the diagnosis of which had been reported in the medical file), cardiovascular risk factors, cardiovascular medication and healthcare resource use (hospital admissions and emergency care). The NYHA scale was used to determine the severity of the disease. An ECG was performed on all patients and it was determined whether they had had an echocardiogram during the last year.
Variables analysedDemographic-anthropometric and clinical-analytical characteristics (BMI, baseline glycaemia and glycosated haemoglobin, systolic and diastolic blood pressure, tobacco and alcohol consumption), complementary diagnostic examinations, therapeutic guidelines and hospitalisations were recorded during the 12 months prior to inclusion and during the study itself. A physical examination and electrocardiographic and biochemical controls were performed at the inclusion visit.
Patients were considered hypertensive if they had been diagnosed as such, and controlled high blood pressure (HBP) was defined as under 130/80 mmHg. The most recent echocardiographic and coronariographic data from the patient’s medical file were collected. Treatment guidelines were recorded at the inclusion visit.
To determine aetiology, the following criteria were considered:
- -
Ischaemic when the patient was diagnosed with ischaemic heart disease.
- -
Valvular when there had been staged valve disease which was at least moderate, with no ischaemic heart disease.
- -
Hypertensive, in patients with high blood pressure and with no other data suggestive of heart disease.
The pharmacological groups studied were diuretics, angiotensin-converting enzyme inhibitors /angiotensin II receptor antagonists (ACE/ARA-II), beta blockers (BB), spironolactone (which was not classified as a diuretic), digoxine and oral anticoagulants. The adherence of each patient to the recommendations in the treatment guides were defined in keeping with the clinical profile of each patient following the GC-ESC.30
A global adherence index was designed for the 6 drugs studied, defined as the percentage of patients who take these medicines according to their clinical characteristics. The ACE or ARA-II, the BB and spironolactone are classified as evidence A with grade 1 recommendation (based on randomised clinical trials, with general consensus that they are useful and beneficial).
Statistical analysisIn this descriptive and cross-sectional study, corresponding to the first phase of the ALBAPIC study, the outcomes of the qualitative variables are expressed in absolute frequencies and percentages, and the results of the quantitative variables are expressed in the means ± standard deviation. Statistical treatment of data was performed using the SPSS programme for Windows, version 21.5. Descriptive statistical analysis was performed based on frequency tables of categorical variables, using the Pearson χ2 test to contrast the significance of association between qualitative variables. To compare the means between groups the Student’s t-test was used for independent samples. Differences with p values < .05 were considered statistically significant.
Ethical aspectsThe study was approved by the Area Research Commission and was carried out in accordance with recognised deontological and clinical best practice regulations. Data were protected from unlawful use by individuals outside the research and the confidentiality of personal data protection and Law 41 /2002, of 14th November, on the autonomy of patients and rights and obligations with regards to clinical information and documentation was respected. The participating parties have therefore considered the information generated by this study as strictly confidential.
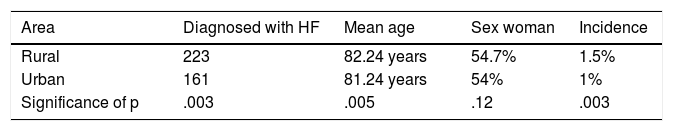
ResultsThree hundred and eighty four patients diagnosed with HF in both health areas were included (161 in the urban area and 223 in the rural area). Mean age was 82.24 ± 10.51 years (81.24 ± 9.59 years in the urban area and 83.37 ± 11 years in the rural area with significant p < .005) values. 54.3% of the patients were women (54% in the urban area and 54.7% rural). The rate of HF was 1% in the urban area and 1.8% in the rural area (Table 2).
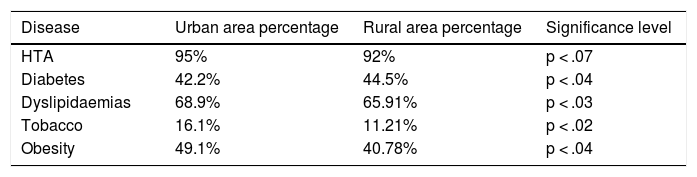
Regarding the prevalence of cardiovascular risk factors, we found that hypertension above all and dyslipidaemias were the most common, with the urban area standing out for a higher rate of hypertension, dyslipidaemia, smoking and obesity compared with rural area patients where there was a higher incidence of diabetes (Table 3).
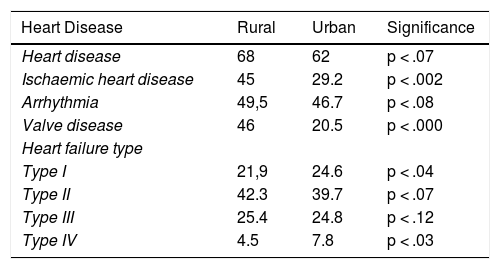
In the rural area there were higher rates of heart disease (68% compared with 62.2%), and the following were statistically significant: ischaemic heart disease (45% compared with 29.2%) and valve diseases (46% compared with 20.5%) (Table 4).
Heart disease.
| Heart Disease | Rural | Urban | Significance |
|---|---|---|---|
| Heart disease | 68 | 62 | p < .07 |
| Ischaemic heart disease | 45 | 29.2 | p < .002 |
| Arrhythmia | 49,5 | 46.7 | p < .08 |
| Valve disease | 46 | 20.5 | p < .000 |
| Heart failure type | |||
| Type I | 21,9 | 24.6 | p < .04 |
| Type II | 42.3 | 39.7 | p < .07 |
| Type III | 25.4 | 24.8 | p < .12 |
| Type IV | 4.5 | 7.8 | p < .03 |
Patients with HF had a higher number of chronic concomitant diseases: in 60% of cases in the urban area the number was between 4 and 6 y and in the rural area between 1 and 4 (Table 5).
Approximately 14% also had an oncological disease in the urban area compared with 21% in the rural area.
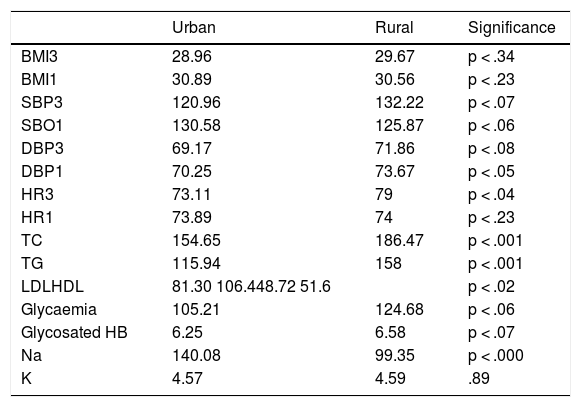
According to data from examination and tests, the main variables were acceptably controlled, with lipidaemic parameters being controlled less in the rural centre (Table 6).
Medical practice data.
| Urban | Rural | Significance | |
|---|---|---|---|
| BMI3 | 28.96 | 29.67 | p < .34 |
| BMI1 | 30.89 | 30.56 | p < .23 |
| SBP3 | 120.96 | 132.22 | p < .07 |
| SBO1 | 130.58 | 125.87 | p < .06 |
| DBP3 | 69.17 | 71.86 | p < .08 |
| DBP1 | 70.25 | 73.67 | p < .05 |
| HR3 | 73.11 | 79 | p < .04 |
| HR1 | 73.89 | 74 | p < .23 |
| TC | 154.65 | 186.47 | p < .001 |
| TG | 115.94 | 158 | p < .001 |
| LDLHDL | 81.30 106.448.72 51.6 | p < .02 | |
| Glycaemia | 105.21 | 124.68 | p < .06 |
| Glycosated HB | 6.25 | 6.58 | p < .07 |
| Na | 140.08 | 99.35 | p < .000 |
| K | 4.57 | 4.59 | .89 |
TC: total cholesterol; HR1: Heart rate in last year; HR3: Heart rate in last 3 months; HDL: HDL cholesterol; BMI1: last year; BMI3: last 3 months; LDL: LDL cholesterol; DBP1: diastolic blood pressure in last year; DBP3: diastolic blood pressure last 3 months; SBP1: systolic blood pressure in last year; SBP3: systolic blood pressure in last 3 months; TG: triglycerides.
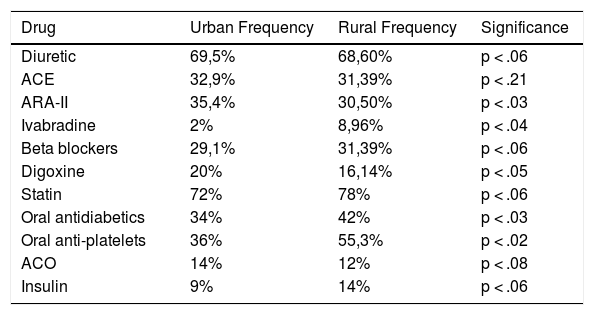
Treatments on study inclusion are contained in Table 7. The mean drugs prescribed for each patient was 6.3 in the rural area and 7.2 in the urban area.
Main treatments.
| Drug | Urban Frequency | Rural Frequency | Significance |
|---|---|---|---|
| Diuretic | 69,5% | 68,60% | p < .06 |
| ACE | 32,9% | 31,39% | p < .21 |
| ARA-II | 35,4% | 30,50% | p < .03 |
| Ivabradine | 2% | 8,96% | p < .04 |
| Beta blockers | 29,1% | 31,39% | p < .06 |
| Digoxine | 20% | 16,14% | p < .05 |
| Statin | 72% | 78% | p < .06 |
| Oral antidiabetics | 34% | 42% | p < .03 |
| Oral anti-platelets | 36% | 55,3% | p < .02 |
| ACO | 14% | 12% | p < .08 |
| Insulin | 9% | 14% | p < .06 |
Regarding treatments, it was observed that diuretics and statins were most commonly used, followed by ACE and ARA-II. In the urban area ARA-II and digoxine are the most used drugs, whilst in the rural area ivabradine, oral antidiabetics, and antiplatelet drugs are used more. Treatment adherence is good, with diuretics and insulin being the drugs with the poorest adherence percentage (Table 7).
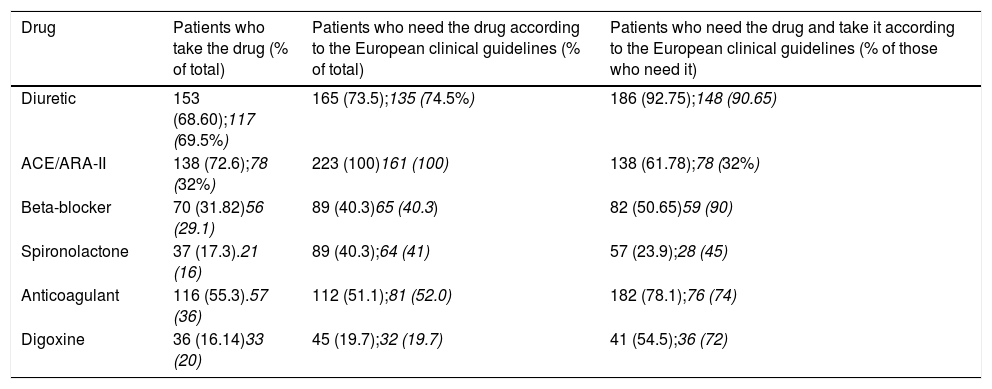
Table 8 shows an acceptable adherence to the GC-ESC for diuretics (68.60% in the rural area and 69.5% in the urban), whilst the ACE/ARA-II have an acceptable use in the rural area (72.6%) and in the urban area it is low (32%). This is similar to BB use, at 50.54% in the rural area and 29.5% in the urban centre and spironolactone, at 23.9% in the rural area and 16% in the urban area. Adherence is lower than the guidelines set down by GC-ESC in the treatment of CHF. ACE/ARA II and beta-blocker treatment was administered to 34 patients in the rural area and to 24 patients in the urban area (29.6%-32%).
Degree of drug adherence to GC-ESC.
| Drug | Patients who take the drug (% of total) | Patients who need the drug according to the European clinical guidelines (% of total) | Patients who need the drug and take it according to the European clinical guidelines (% of those who need it) |
|---|---|---|---|
| Diuretic | 153 (68.60);117 (69.5%) | 165 (73.5);135 (74.5%) | 186 (92.75);148 (90.65) |
| ACE/ARA-II | 138 (72.6);78 (32%) | 223 (100)161 (100) | 138 (61.78);78 (32%) |
| Beta-blocker | 70 (31.82)56 (29.1) | 89 (40.3)65 (40.3) | 82 (50.65)59 (90) |
| Spironolactone | 37 (17.3).21 (16) | 89 (40.3);64 (41) | 57 (23.9);28 (45) |
| Anticoagulant | 116 (55.3).57 (36) | 112 (51.1);81 (52.0) | 182 (78.1);76 (74) |
| Digoxine | 36 (16.14)33 (20) | 45 (19.7);32 (19.7) | 41 (54.5);36 (72) |
In bold, rural area; in italics, urban area.
HF hospital admissions had occurred for 34.25% of patients in urban HC and to 42% in rural HC, and of these 16.8% in urban HC and 25.4% in CS rural had been admitted once, 7.5% in urban HC and 15% in rural HC had been twice, 3.7% in urban HC and 1% in rural HC 3 times and 5% in urban HC and 2% in rural HC from 4 to 7 times.
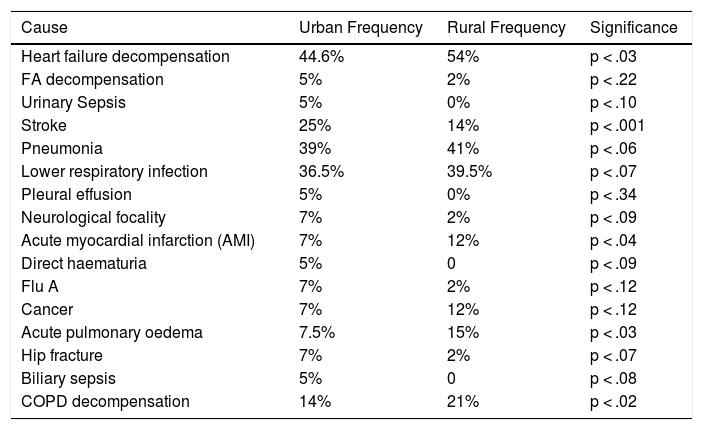
The main causes of admission and readmission were for cardiac decompensation and infection of the lower respiratory airways in both areas, with significant differences in the rural area for HF decompensation and chronic obstructive pulmonary disease (COPD) and AMI, and in the urban area for stroke (Table 9).
Causes of hospitalisation.
| Cause | Urban Frequency | Rural Frequency | Significance |
|---|---|---|---|
| Heart failure decompensation | 44.6% | 54% | p < .03 |
| FA decompensation | 5% | 2% | p < .22 |
| Urinary Sepsis | 5% | 0% | p < .10 |
| Stroke | 25% | 14% | p < .001 |
| Pneumonia | 39% | 41% | p < .06 |
| Lower respiratory infection | 36.5% | 39.5% | p < .07 |
| Pleural effusion | 5% | 0% | p < .34 |
| Neurological focality | 7% | 2% | p < .09 |
| Acute myocardial infarction (AMI) | 7% | 12% | p < .04 |
| Direct haematuria | 5% | 0 | p < .09 |
| Flu A | 7% | 2% | p < .12 |
| Cancer | 7% | 12% | p < .12 |
| Acute pulmonary oedema | 7.5% | 15% | p < .03 |
| Hip fracture | 7% | 2% | p < .07 |
| Biliary sepsis | 5% | 0 | p < .08 |
| COPD decompensation | 14% | 21% | p < .02 |
Flu vaccination is low, at 56% in the rural area and 48% in the urban area. Pneumococcal vaccination is lower, at 34% coverage in both areas.
From statistical comparison of variableswe may observe that age, sex and number of associated chronic diseases are statistically significant, with a higher number of admissions and mortality (p < .005).
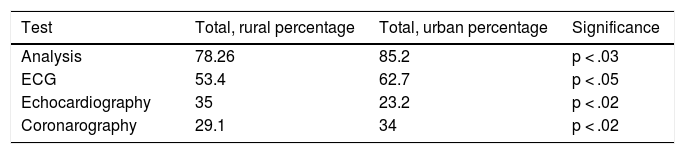
Regarding control with additional tests, there is a higher request for analysis and ECG in the urban area. There was a very low percentage of echocardiograms performed on these patients. However, it is striking that they are requested more in the rural area than the urban one.
Coronarography performed was in proportion to the ischaemic heart disease (Table 10).
DiscussionHF affects 1%-2% of the adult population in developed countries, and this percentage increases drastically with age up to 8%-10% in the group of patients aged from 70-80 years. In this study a HF rate of 1% in the urban population and almost 2% in the rural population was appreciated. Although this could be considered to match other published studies, the figures could be classed as low compared with other national studies which refer to rates of 5%. The difference could be due to under diagnosis or poor diagnostic codification in the clinical file.1–3
The patient profile with HF is characterised by advanced age, with the age in the rural area being higher than that in the urban area and with a predominance of women. For at least 50% of them the course of the disease was above 3 years. This disease uses many healthcare resources. The cardiologist is usually the hospital specialist referred to and under half of the patients required hospital admission during the last year, which was often directly related to HF.
The prevalence of HF with normal LVSF is significantly higher than HF with impairment in systolic function and is associated with a more advanced age and greater prevalence of HBP, auricular fibrillation and obesity. In our patients we found there was a high rate of HBP (95% and 92%, respectively) and heart disease (65% and 62%, respectively), which matches the existing physiopathological theories that both of these conditions impair the heart muscle, leading to HF.31,32
Although the use of diagnostic resources was significantly higher in men, no major differences between the sexes were observed in the use of drugs with recognised prognostic benefit.
The approach to HF involves complex coordinated care, mainly between PC, internal medicine and cardiology. PC is the first level of care for these patients globally and continuously, but diagnostic techniques and treatments involving hospital specialities such as cardiology and internal medicine, and sometimes hospital emergency departments, are required.
Clinical practice guidelines,30 with the highest level of recommendation and evidence (class i A), propose the creation of multi-disciplinary programmes to reduce the risk of hospitalisation and mortality caused by HF.
There are many ways around HF organisation but the essential aspects t consider are:
- -
Awareness of the initial situation
- -
Identification of indicator to be measured
- -
Inclusion of PC in the organisational model
TM is surely another means towards optimising coordination between levels of care that would provide changes to our organisational model and make it much more adapted to current demands. The Tárraga López et al. study brings to light what the baseline situation in their area of reference is, from the PC professional’s outlook.22,23 This study aimed at observing the relationship and differences between HF care in the health area of Albacete so as to introduce a non invasive TM programme which would unify both diagnostic care and control and treatment in 2 different areas. This would involve a rural area (small dispersed population groups with difficulty of access to the cardiologists and diagnostic tests) and an urban area (population concentrated in the HC with easy access in particular to tests). As we stated in the introduction, interventions vary greatly from some studies to others, and may even not be well specified in some. To design a TM programme it was essential to discover the demographic, socio-cultural and epidemiological characteristics of the population, and the health resources available to it. We believe it was vital to make these data available prior to proposing the telemetric intervention model.27
Apart from contributing to a better awareness of the disease, which up until now in the rural area especially has not been recognised, this study has also been able to evaluate strategies aimed at achieving more effective prevention and treatments, where coordination between PC and specialised care must be its keystone. This type of intervention have proven to improve patient quality of life as the need for hospitalisations are reduced and the use of drugs with a recognised prognostic benefit, together with treatment adherence, are optimised.11–13,22,23,31,32
We also believe that this type of initiative leads to the creation of stable HF records promoting awareness, improvement in care, research and continuous professional training.
Clinical and epidemiological characteristicsThere are 2 differentiated clinical profiles linked to the area in which patients are attended in the Spanish health system. The patients monitored in cardiology taken systematically from the Spanish ESC-HF-LT register and BADAPIC,33,34 are younger, mostly male and present with lowered ejection fraction in 2/3 of cases. In them, the predominant aetiology is ischaemic heart disease and its symptomatic level is higher. Compared with this population, the patients monitored in PC, taken from the CARDIOPRES35 and GALICAP24 studies are older (mean age > 70 years), with a higher proportion of women. These patients have more comorbidities, such as auricular fibrillation and HBP. The majority present with normal ejection fraction and the most common aetiology is hypertension and in general, they present with mild or moderate HF symptoms. Our study is more similar to these, although in the urban environment there is more HBP and less ischaemic heart disease in the rural environment. This finding has not been confirmed in other studies.
The European study on outpatient treatment of heart failure, conducted by cardiologists, reports similar results. It includes 1252 outpatient patients diagnosed in 3 European countries (Spain, France and Germ may) with very similar clinical characteristics to those of the BADAPIC33study, with the exception of presenting with a HBP prevalence similar to that observed in our study and above 60% in the 3 countries.16 This could be due to greater selection of patients in the BADAPIC33 study and to a higher survival of patients with HF and HBP compared to the group with ischaemic heart disease, and this may have affected the outpatient patient profile with this disease.
The INCA study includes somewhat fewer than 1000 patients hospitalised for HF in cardiology and internal medicine services in 12 Galician hospitals, although the mean age is higher than that described in the studies previously commented upon and is similar to that of the GALICAP study. The other clinical characteristics are very similar to those described in the studies and hospital registers.24,25
The CARDIOTENS18 study conducted in 1999 by cardiologists and PC doctors in Spain included 1420 patients diagnosed with HD, with a mean age of 71 years, predominantly women and a high prevalence of HBP. These were similar characteristics to those observed in similar studies conducted in Portugal (EPICA study)19 and in 15 member countries of the European Society of Cardiology (IMPROVEMENT study).20
One of the data we consider to be of greatest relevance in our study is the high prevalence of HF with normal LVSF: at 70.23% in the rural area and 71% in the urban area, and where there was an echocardiographic study LVSF was > 50%. This is one of the few times that a Spanish HF study has observed this with a normal systolic function, more commonly than that of a depressed systolic function, and this is probably indicating a change in the profile of these patients. In many previous studies the state of the left ventricular systolic (LVSF) function is not systematically described and in those where it is, HF with reduced LVSF always predominates.14–16,36 As we have mentioned, in the BADAPIC33 study 68% of patients had a LVSF < 45%, with similar results being observed in the hospital series, where HF cases with depressed systolic function predominated.15
Outpatient patients with HF have many comorbidities and the number of these has increased in recent years in parallel to the ageing of the population. A significant difference was found in the number of higher comorbidites in the urban area compared with the rural area and this has led to greater complexity in management. A significant statistical relationship was observed between the number of concomitant diseases and decompositions with the increase in hospital admissions, resulting in the need for early and multi-disciplinary treatment of HF in these patients.
The results of our study coincide with those described, except regarding therapeutic strategy, which was similar in both patient groups, both in the use of drugs that block the renin-angioitensin-aldosterone system and in the BBs.
Treatment optimisation is one of the main goals of care for patients with HF; it has been demonstrated to prolong life and reduce the need for hospitalisations, improving quality of life in general.26 Besides pharmacological treatment, correct treatment of these patients forces them to make changes to their lifestyle, plan percutaneous and surgical interventionist measures, use devices, etc. Simple management programmes for the disease, with PC medical intervention and nursing staff have been proven to have a favourable impact on all therapeutic objectives.11–13,31,32
In the ALBAPIC study, the use of drugs with recognised prognostic benefits coincides with that observed in the principal studies of this type published recently; in the Euro-Heart Failure Survey, the percentage of patients who received ACE or ARA-II was 66% and 37%33 for those receiving BB. In our study this was 68% in urban areass and 62% in rural areas for ACE/ARA-II, and 29.1% in urban areas and 31.2% in rural areas for BB, respectively.
These results compare very favourably with those of many registers and studies conducted, both in Spain and internationally. The results of the BADAPIC study offer similar drug use figures to those observed in clinical trials, with an 87% use of ACE or ARA-II, 59% of BB and 32% of spironolactone and surprisingly, good survival and a low rate of complications during follow-up.15 As the researchers recognise, the selection of patients with a low mean age (66 years), the relatively benign nature of the disease (only 68% of patients had been previously hospitalised for HF) and the follow-up characteristics (specialised HF units) significantly affect outcomes.
Treatment for HF with normal LVSF deserves special mention. Up until now, the use of drugs has been based on physiopathological considerations, since no clinical trials to guide treatment28,29 explicitly have been available.
Regarding patient treatment it was observed that diuretics and statins are the most commonly used drugs, followed by ACE and ARA-II. In the urban area ARA-II and digoxine are most commonly used, whilst in the rural area ivabradine, oral antidiabetics and antiplatelet drugs are used more. Treatment adherence is good, with diuretics and insulin being the drugs with the poorest adherence percentage. The use of sacubitril/valsartan is still minimal, since at the time of study they were starting to be marketed in Spain.
The medication adherence index with the highest level of evidence is 66%; this percentage is determined by the low prescription of BB and of spironolactone, because only 2 out of every 4 patients who need them take these drugs. It is possible that the PC physician’s ignorance of the LVSF value in over half of patients negatively affects the prescription of these drugs. The low usage of these 2 drugs has been widely reported,6,12,13,31 despite their high level of evidence of beneficial effects in morbimortality. One exception is a study conducted in Switzerland, also in the PC environment,15 where they obtained a percentage BB prescription of 67%, clearly higher than the majority of publications. However, only 25% are treated with aldosterone antagonists, with a result similar to other studies. Large scale clinical trials reported that BBs reduce mortality in patients with CHF,14,36 and these benefits also persist in patients who are over 65.15
The variables which are associated with a low BB prescription, particularly in the rural area are aged over 70 years, female and COPD,in keeping with other publications,16,17 whilst diabetes is associated with a higher prescription of BB, after adjustment due to logistic regression. Only age, heart disease and HBP help to explain BB adherence. Intolerance and adverse effects are the reasons most commonly given by professionals for not prescribing or for withdrawing them;31 however, the majority of adverse effects are mild and it is only necessary to withdraw this drug on few occasions. A PC physician with appropriate training can therefore safely prescribe BBs.18
There is a significant difference between anticoagulant treatments. In the urban area they are prescribed in approximately 36% and in the rural area 55.3%, and they are second drugs after diuretics with the best GC-ESC treatment adherence.
A significant proportion of patients receive cardiac glycosides (20% urban and 16.14% rural). This drug has no effect on survival, but improves symptoms. These findings are also in keeping with European studies.18–23
Youner patients, those who have a history of ischaemic heart disease, and those who were hospitalised during the last year demonstrate better use of ACE/ARA-II, BB and spironolactone.
Our patients were mostly elderly, mostly female, and HBP was the most common aetiology. The majority of patients had mild to moderate CHF, around 60%, and were in class ii of the NYHA, with several heart-failure-associated diseases. This profile matches other studies conducted in PC,21,22 but contrasts with that of studies conducted in the hospital environment.23,31 This context helps to explain the low adherence to the recommendations proposed in the GC-ESC.
Two recent studies have indicated that prognosis for this type of HF, unlike that of systolic dysfunction, has not improved during the last decade, despite the use of drugs which have demonstrated their usefulness in this condition.25,26 Research into treatment must therefore be broadened for this increasingly prevalent cardiovascular disease which presents with an extremely poor prognosis. The indications are that, although systolic HF from a therapeutic viewpoint behaves like a relatively homogeneous disease HF with normal LVSF involves highly diverse groups of patients with very different responses to therapeutic interventions.
There were hospitalisation due to HF for 34.25% of patients in urban HC and 42% in rural HC. This is relatively higher than other recently published studies, which in 2013 reported rates of 14.5% in the region of Murcia and 23.3% in Castile León.37,38 Hospitalisations occurred for elderly people with multiple baseline conditions (hypertension, diabetes mellitus, COPD, kidney disease). The main causes of admission and readmission were mainly for cardiac decompensation and pneumonia or infection of the lower respiratory airways in both areas, with significant differences in the rural area for HF (COPD) and AMI, and in the urban area for stroke. This matches other studies which report comorbidities as the main cause of readmission to hospital.39
Regarding control with additional tests, there is a higher request for analysis and ECG in the urban area. A very low percentage of echocardiograms are performed on these patients. However, it is striking that they are requested more in the rural area than the urban one.
Coronarography performed was in proportion to ischaemic heart disease. The main causes of readmission and mortality were respiratory failure aetiology. We observed that flu vaccination was low, at 56% in the rural area and 48% in the urban area. Pneumococcal vaccination is lower, at 34% coverage in both areas.
Based on these results the programme designed should contain a reminder of vaccination schedulers and the scaled use of drugs to improve prescription and the systemic practice according to echocardiography guidelines.
Implications and limitationsWe believe that the studies of these characteristics reflect the situation of HF better in a specific area, since practically all patients with firm diagnosis of the disease may be included. It is possible that a group of patients with HD did not require hospitalisation at any time during the course of the disease. However, if we take into account the nature of the disease we believe that this possibility is remote and we are convinced that the selection with this criteria avoids the inclusion of patients with doubtful diagnosis that often undermines HF study and register results.
Only 35% of patients in the rural area and 23.2% in the urban area had had an echocardiogram, which could have called into question HF diagnosis, although we could consider that the possibility of a false diagnosis is unlikely.
To conclude, the proposals put forward by the authors, together with PC specialists, internal medicine specialists, cardiologists, professions from the hospital emergency department for the optimisation strategies for HF management are to:
- -
Optimise clinical history recording.
- -
Increase hygiene and dietary recommendations.
- -
Increase coverage of flu and pneumococcal vaccination.
- -
Put into efect the relationship between PC and Cardiology using corporate electronic mail, telematic consultation, and joint development of an app enabling follow-up and activation of action plans, telephone plans and joint clinical sessions.
- -
TM plays an important role in all of this and has been proven to promote better control of HF, thereby reducing hospital admissions and mortality caused by HF.27–30,33–35
The authors have no conflict of interests to declare.
Please cite this article as: Tárraga López PJ, Perez Romero FJ, Panisello Royo JM, Simón Garcia MA, Villar Inarejos MJ, Madrona Marcos F, et al. Análisis comparativo del manejo de la insuficiencia cardiaca en 2 medios diferentes: rural versus urbano. (Estudio ALBAPIC). Clin Investig Arterioscler. 2020;525–167.