Given the progressive increase in the number of these products and their rising use by the population, the Spanish Society of Arteriosclerosis (SEA) has considered it appropriate to review the available information, select the results of the scientifically more robust studies and take a position on their usefulness, to recommend to health professionals and the general population their potential utility in terms of efficacy and their possible benefits and limitations. The following clinical scenarios have been identified in which these products could be used and will be analyzed in more detail in this document: (1) Hypolipidemic treatment in subjects with statin intolerance. (2) Hypolipidemic treatment "a la carte" in individuals in primary prevention. (3) Long-term cardiovascular prevention in individuals with no indication for lipid-lowering therapy. (4) Patients with optimized lipid-lowering treatment who do not achieve therapeutic objectives.
Para el tratamiento de la hipercolesterolemia, además de aconsejar una alimentación saludable, puede ser conveniente recomendar alimentos funcionales o nutracéuticos con efecto hipolipemiante. Dado el progresivo incremento en el número de estos productos y su creciente utilización por la población, la Sociedad Española de Arteriosclerosis (SEA) ha creído conveniente revisar la información disponible, seleccionar los resultados de los estudios científicamente más sólidos y posicionarse sobre la utilidad de los mismos, para recomendar a los profesionales sanitarios y a la población general su potencial utilidad en términos de eficacia y sus posibles beneficios y limitaciones. Se han identificado los siguientes escenarios clínicos en los que se podrían utilizar estos productos y que se analizarán con más detalle en este documento: (1) Tratamiento hipolipemiante en sujetos con intolerancia a estatinas. (2) Tratamiento hipolipemiante “a la carta” en personas en prevención primaria. (3) Prevención cardiovascular a largo plazo en personas sin indicación de tratamiento hipolipemiante. (4) Pacientes con tratamiento hipolipemiante optimizado que no alcanzan objetivos terapéuticos.
In addition to recommending a heart-healthy diet for hypercholesterolaemia control it may, in certain situations, be appropriate to use functional foods or nutraceuticals with a lipid-lowering effect. In addition to the macro- and micronutrients contained in foods, there are a number of biocomponents with important effects on health, known as nutraceuticals. These products, in turn, are related to functional foods and supplements.
“Functional foods" have specific characteristics that distinguish them from conventional foods, the best-known definition being that of the European Union project "Functional Food Science in Europe (FUFOSE)". According to this definition, a functional food is a food which, beyond its nutritional value, influences physiological functions in a measurable way in terms of health promotion or disease prevention.1 A functional food is a natural food, a food to which a component has been added, or a food from which an ingredient has been removed, a food to which components or their bioavailability have been modified, or any combination of these possibilities. In all events, functional foods are always foods (not tablets or capsules) and their health effects must be demonstrated in amounts that can normally be consumed in the normal diet. An example of functional foods, with a well-demonstrated effect on the reduction of total cholesterol and cholesterol carried in low-density lipoprotein (LDL-C) are dairy products and margarines fortified with phytosterols or stanols.2
In English-speaking countries, functional foods are also called "nutraceuticals", a term that denotes both their food origin and their similarity in function to pharmaceuticals. However, this can be confusing, as nutraceuticals are conceptually derived from food and are presented in the form of capsules, tablets, pills or other galenic preparations that are not food at all.3 An added complexity is that in the U.S.A. nutraceuticals are sometimes lumped together with dietary supplements, which is a distinct category of nutritional preparations. Despite the growing demand for these products, neither in Europe nor in the U.S.A. does any systematic regulation exist with regard to the medical properties, health claims and safety of nutraceuticals, which remain in a grey area between food and pharmaceuticals. The term "nutraceutical" does not appear in EU legislation.4 Red yeast rice, which is usually presented in capsule form (not as a food), is an example of a nutraceutical with total cholesterol and LDL-C-lowering properties.5
Finally, although not considered in this document, it should be noted that dietary supplements, according to the EU directive, are nutritional preparations designed to supplement the normal diet and consist of concentrates of nutrients, vitamins, minerals or other products of plant origin, alone or in combination, marketed in the form of capsules, tablets or similar in small fixed doses.6 Similarly, the Food and Drug Administration (FDA) defines them as "products in capsule, tablet or similar form containing a dietary ingredient such as a vitamin, mineral, amino acid or other substance of plant origin, intended to add nutritional value (supplement) to the diet.7 While there has been a massive uptake of vitamin and mineral supplements marketed as natural alternatives to protect general health and cardiovascular health in particular, particularly in the U.S.A., there is still no solid scientific evidence of a potential preventive effect on cardiovascular disease, cancer or total mortality.8
The consumption of functional foods and nutraceuticals, especially those aimed at lowering total cholesterol levels, has increased steadily over the last two decades. According to a market report by the pharmaceutical company AORA Health, the nutraceuticals market is estimated to grow by almost 50% until 2028, with an annual increase of 8.6%. The inclusion of a chapter on these products in the latest European Society of Cardiology/European Arteriosclerosis Society (ESC/EAS) guidelines for the management of dyslipidaemias highlights their importance in cholesterol control.9 Despite this increase, studies are multiple and highly variegated with respect to their design, results and scientific quality. Moreover, while some of these products significantly reduce cholesterol, data on their potential cardiovascular benefit are lacking and are unlikely to be available in the future, as large randomised clinical trials (RCTs) with outcome of major cardiovascular events after several years of follow-up would be required. Moreover, most of the data on their safety are limited as only short-term studies are available. As a result, recommendations on their use have many limitations.10
Given the increase in the number of products aimed at reducing cholesterolaemia and their growing consumption, the Spanish Society of Artherosclerosis (SEA) has considered it appropriate to review the available information, select the results of the most scientifically sound studies and take a position on them in different clinical scenarios, in order to recommend to health professionals and the general population their potential usefulness in terms of efficacy and their possible benefits and limitations.
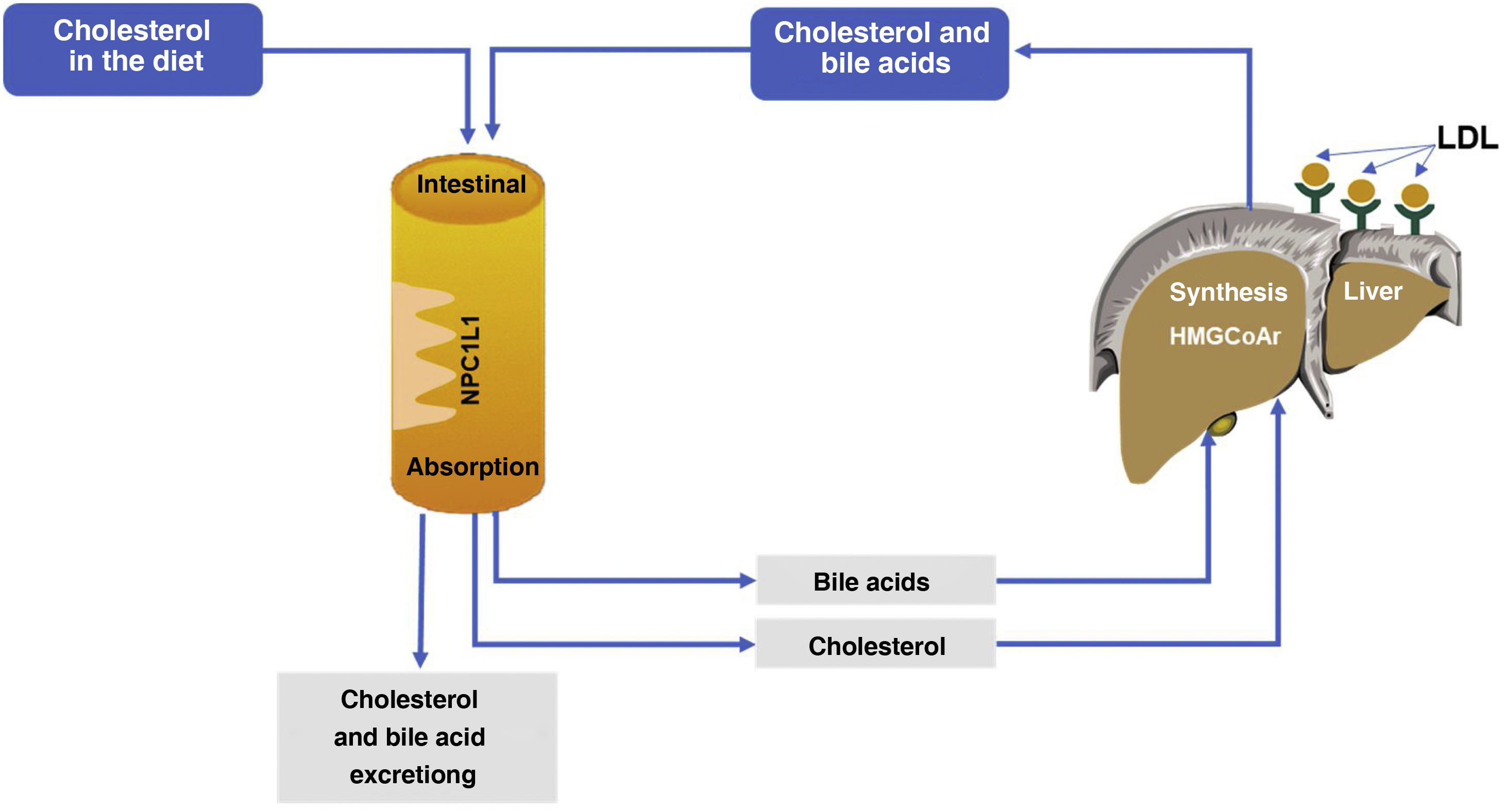
The importance of cholesterol in the development of cardiovascular diseaseCholesterol is essential for the proper functioning of the body due to its physiological functions, including being a structural component of cell membranes, a precursor of vitamin D, of steroid hormones (progesterone, oestrogen, testosterone, cortisol and aldosterone) and bile acids. Furthermore, humans are unable to metabolise cholesterol because they do not have metabolic pathways that catabolise the cyclopentane-perhydrophenanthrene ring, so it must be transported to the liver for elimination into the intestine via the bile, along with bile acids. This highlights the importance of cholesterol homeostasis, through the balance between endogenous synthesis, intestinal absorption and biliary secretion of bile acids and cholesterol. Since bile acids are efficiently reabsorbed and some biliary cholesterol is reabsorbed in the intestine, the overall cholesterol balance depends on inputs (synthesis and diet) being balanced by losses (faecal excretion) (Fig. 1). The amount of cholesterol excreted with faeces depends on the efficiency of intestinal absorption of intestinal cholesterol (biliary and dietary) into the enterohepatic circulation. This justifies the interest in the mechanisms of intestinal cholesterol synthesis and absorption as therapeutic targets for lowering cholesterolaemia.
Hypercholesterolaemia with increased LDL-C is associated with the accumulation of cholesterol in the arterial wall, which is the main factor in the development of atheromatous plaque, whose growth and eventual thrombosis leads to ischaemic syndromes. In this sense, cardiovascular disease (CVD) and especially coronary heart disease and atherothrombotic ischaemic stroke are the leading cause of mortality worldwide and one of the main contributors to disability. In Spain, according to data from the National Institute of Statistics, diseases of the circulatory system continue to be the leading cause of death in 2020 with 119,853 deaths, representing 24.3% of total deaths, with an increase of 2.8% over the previous year.11
Reduction in cholesterol as causal treatment for artherosclerosisThe pathophysiological understanding of atherosclerosis is becoming increasingly precise and has led to the identification of LDL-C as a primary aetiological agent, which stimulates inflammatory phenomena and cell proliferation in the vascular wall.12,13 The cardiovascular benefits of lipid-lowering drugs are due to their lowering effect on LDL-C concentrations. There is strong clinical evidence, extensively explored by the Cholesterol Treatment Trialist Collaboration (CTTC),14 showing that the reduction in CVD risk associated with statin therapy is mediated by the lowering of LDL-C concentrations in absolute terms. In addition, LDL-C lowering mediated by other drugs, such as ezetimibe or proprotein convertase subtilisin/kexin type 9 (iPCSK9) inhibitors, or even by non-pharmacological means, such as diet or ileal bypass surgery, leads to the same risk reduction per unit of reduced LDL-C.15 Subsequently, the benefit of cholesterol lowering, regardless of the mechanism by which it is achieved, has been corroborated by Mendelian randomisation studies.16
More recently, studies with iPCSK9 assessing the progression of coronary atherosclerosis using intravascular ultrasound and innovative image analysis techniques have shown that even decreases in LDL-C below those currently recommended are accompanied by a decrease in the atherosclerotic burden and beneficial effects on plaque composition.17 It can therefore be stated that in this clinical situation we are performing an aetiological treatment of the disease.
Unmet needs in the management of hypercholesterolaemia: the clincial usefulness of nutraceuticalsThe therapeutic arsenal for the management of hypercholesterolaemia includes potent, safe drugs with numerous scientific evidences of efficacy and safety, both in primary and secondary prevention of CVD. Drugs as varied as statins, ezetimibe, PCSK9 inhibitors, bempedoic acid and anion exchange resins are available. In monotherapy or in combination, these drugs achieve therapeutic goals in most patients with severe hypercholesterolaemia, with the exception of patients with homozygous familial hypercholesterolaemia (FH). However, in clinical practice, side effects, personal reasons or lack of efficacy, among other barriers, make it difficult to achieve optimal control of dyslipidaemia in many patients. In these circumstances, functional foods or nutraceuticals can play an important role.
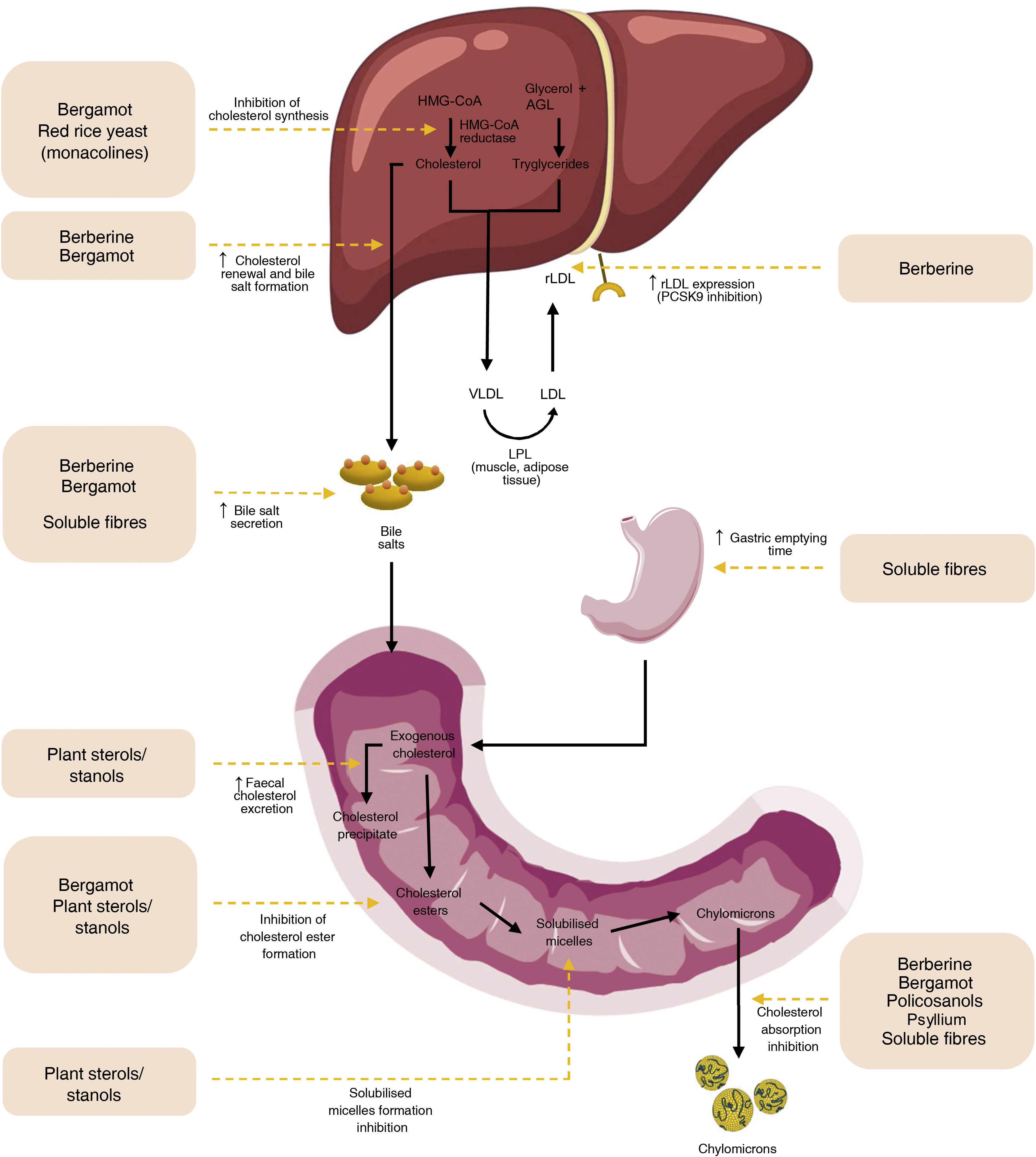
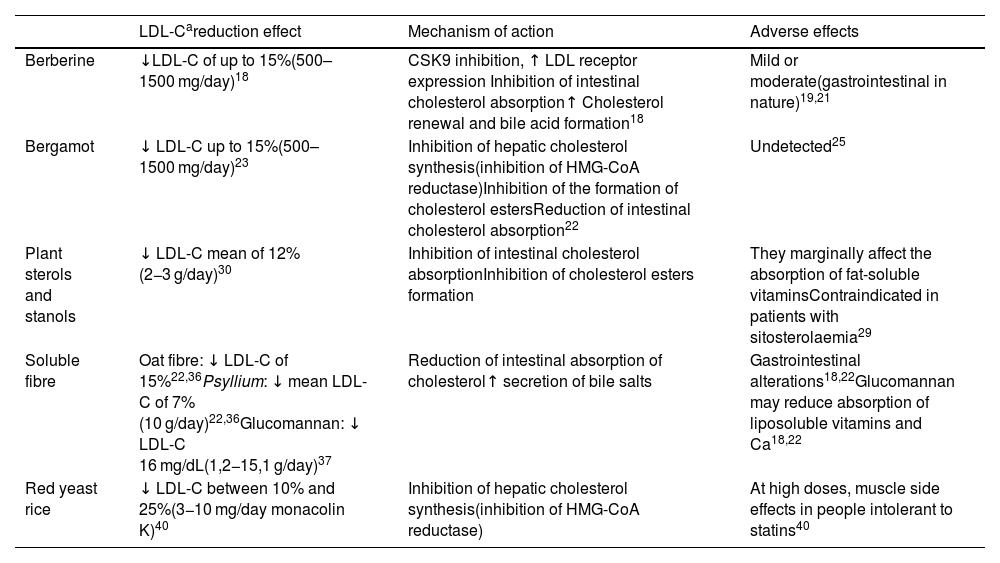
Cholesterol-lowering efficacy of nutraceuticalsThe functional foods and nutraceuticals with the greatest efficacy in reducing cholesterol levels are listed in Table 1, showing the expected cholesterol-lowering effect of each of them. Fig. 2 summarises their different mechanisms of action.
Cholesterol-lowering effect of different functional foods and nutraceuticals.
| LDL-Careduction effect | Mechanism of action | Adverse effects | |
|---|---|---|---|
| Berberine | ↓LDL-C of up to 15%(500–1500 mg/day)18 | CSK9 inhibition, ↑ LDL receptor expression Inhibition of intestinal cholesterol absorption↑ Cholesterol renewal and bile acid formation18 | Mild or moderate(gastrointestinal in nature)19,21 |
| Bergamot | ↓ LDL-C up to 15%(500–1500 mg/day)23 | Inhibition of hepatic cholesterol synthesis(inhibition of HMG-CoA reductase)Inhibition of the formation of cholesterol estersReduction of intestinal cholesterol absorption22 | Undetected25 |
| Plant sterols and stanols | ↓ LDL-C mean of 12%(2−3 g/day)30 | Inhibition of intestinal cholesterol absorptionInhibition of cholesterol esters formation | They marginally affect the absorption of fat-soluble vitaminsContraindicated in patients with sitosterolaemia29 |
| Soluble fibre | Oat fibre: ↓ LDL-C of 15%22,36Psyllium: ↓ mean LDL-C of 7%(10 g/day)22,36Glucomannan: ↓ LDL-C 16 mg/dL(1,2−15,1 g/day)37 | Reduction of intestinal absorption of cholesterol↑ secretion of bile salts | Gastrointestinal alterations18,22Glucomannan may reduce absorption of liposoluble vitamins and Ca18,22 |
| Red yeast rice | ↓ LDL-C between 10% and 25%(3−10 mg/day monacolin K)40 | Inhibition of hepatic cholesterol synthesis(inhibition of HMG-CoA reductase) | At high doses, muscle side effects in people intolerant to statins40 |
HMG-CoA reductase, 3-hydroxy-3-methyl-glutaryl-CoA reductase; LDL-C, LDL cholesterol; PCSK9, proprotein convertase subtilisin/kexin type 9.
Mechanisms of action of plant sterols and nutraceuticals. Modified from Cicero AFC, Colleti A, Bajraktari G, Descamps O, Djuric DM, Ezhov M, et al. Lipid lowering nutraceuticals in clinical practice: Position paper from an International Lipid Expert Panel. Arch Med Sci. 2017;13:965-1005. doi: 10.5114/aoms.2017.69326.
Berberine is a plant alkaloid from the isoquinoline group, the main active component of Rhizoma coptidis, a plant used in many formulas in traditional Chinese medicine. Its mechanism of action is related to inhibition of PCSK9 and reduction of lysosomal degradation of hepatic LDL receptors. Berberine also contributes to the reduction of cholesterolaemia by inhibiting intestinal absorption of cholesterol, increasing its faecal excretion and promoting hepatic cholesterol catabolism and bile acid formation. It also stimulates the adenosine monophosphate-activated protein kinase (AMPK) pathway, which promotes fatty acid oxidation and inhibits the expression of lipogenic genes such as acetyl coenzyme A carboxylase.18 Vasculoprotective, anti-inflammatory, oxidative stress-reducing, and insulin resistance-enhancing effects have been reported for berberine.19,20 A meta-analysis of 46 RCTs in patients with diabetes showed that berberine supplementation improved chronic inflammation status by reducing circulating concentrations of C-reactive protein, interleukin-6 and tumour necrosis factor-α.19
A systematic review and meta-analysis of RCTs evaluating the cardiometabolic therapeutic effect of berberine found benefits in the lipid profile, with reductions in total cholesterol, LDL-C and triglycerides, and increases in high-density lipoprotein cholesterol (HDL-C), as well as improvements in insulin resistance.21
The side effects of berberine are mild to moderate, mainly gastrointestinal (diarrhoea, constipation, meteorism, etc.), comparable to those seen in the control groups of RCTs. ECA.19,21 No nephrotoxicity or hepatotoxicity effects have been found, nor significant differences in transaminase and creatinine concentrations in berberine-treated patients compared to controls.19,21
Berberine treatment studies are heterogeneous in terms of design, treatment period and dose used, with limited evidence on its therapeutic effect. According to the most recent observations, the cholesterol-lowering effect is seen with consumption of between 500 and 1500 mg/day and is associated with a reduction in LDL-C concentrations of up to 15%.18 More good quality RCTs are needed to determine the role of berberine in the management of dyslipidaemia.18,22
BergamotBergamot is a citrus fruit (Citrus bergamia), native to southern Italy, whose composition is rich in various phytochemicals such as brutieridin, melitidine and other flavonoids (neoeriocitrin, naringin and neohesperidin). The high content of these constituents in bergamot appears to be implicated in its cholesterol-lowering action.23 The juice of this citrus fruit has the capacity to inhibit hepatic cholesterol synthesis. A fraction rich in brutieridin, melitidine and neoeriocitrin, extracted from bergamot peel, acts by inhibiting HMG-CoA reductase by a mechanism similar to that of statins and acyl-CoA:cholesteryltransferase, thereby reducing the formation of cholesterol esters. Other mechanisms of action possibly involved in the lipid profile effects of bergamot are the reduction of intestinal cholesterol absorption, inhibition of LDL particle oxidation, which is key to atheroma plaque formation, and stimulation of the AMPK pathway, which reduces cholesterol synthesis through inhibition of HMG-CoA reductase.22
A recent systematic review and meta-analysis including 14 RCTs shows that bergamot supplementation significantly reduces total cholesterol, triglycerides, and LDL-C concentrations and increases HDL-C levels.24
Another systematic review analysing 12 studies with bergamot (10 RCTs and 2 observational studies with a total of 870 participants) shows a reduction of 12.3%–31.3% in total cholesterol, 7.6%–40.8% in LDL-C and 11.5%–39.5% in triglyceridaemia. The large variability observed in the cholesterol-lowering effect among the studies analysed is probably due to the variegation of the designs and doses of bergamot used, with higher doses generally having a greater effect. In all the RCTs reviewed, which ranged in duration from 30 days to 6 months, bergamot showed a good safety profile, with no side effects detected.25
In short, clinical studies analysing the lipid-lowering properties of bergamot show that the polyphenols it contains, at doses of 500–1500 mg/day, reduce LDL-C by around 15%, depending on the dose, with a highly variable effect depending on the degree of purification of the extract.23 Further studies are needed to elucidate the most appropriate form of presentation and dosage, allowing a recommendation to be made with a higher level of evidence.
Plant sterols and stanolsOilseeds (cereals, legumes, nuts) contain steroid-type phytochemical compounds, the plant sterols or phytosterols, whose cholesterola-lowering properties have been known since the 1950s.26 Sitosterol and campesterol are the most abundant and on average comprise 65% and 30% of the usual dietary intake of phytosterols. The chemical structure of phytosterols differs from that of cholesterol by the presence of C:24 modified side chains. Stanols, which are less abundant in nature, are saturated sterols, i.e., they lack the double bond in the steroid ring.27 Although their molecular structure is almost identical, cholesterol and phytosterols are metabolised differently. Cholesterol absorption in the human intestine averages 50%, whereas absorption of phytosterols is no more than 5% and, once absorbed, they are rapidly excreted in the bile. In gram quantities in the intestinal lumen, phytosterols and stanols reduce the absorption of cholesterol, both from the diet and from bile, because they displace the steroid from the micelles that solubilise it as a step prior to its absorption by the NPC1L1 transporter. NPC1L1.27 Reduced absorption results in less cholesterol reaching the liver, which has two compensatory effects: increased synthesis and increased expression of LDL receptors (Fig. 2), two processes activated by the transcriptional factor SREBP-2 (Sterol-regulatory element-binding protein-2) sensitive to hepatic cholesterol concentration. The net effect is a reduction in serum LDL-C concentrations.28
Other mechanisms involved in the cholesterol-lowering effect of plant sterols include inhibition of enzymatic esterification of free cholesterol in the enterocyte, so that less cholesterol will be incorporated into the forming chylomicrons, and there will be increased synthesis of the ABCG5 and ABCG58 transporters, which facilitate the efflux of free cholesterol from the enterocyte back into the intestinal lumen.29 The amount of phytosterols provided by a plant-rich diet does not usually exceed 600 mg/day. These compounds have been introduced on the market as functional foods, enriching dairy products, margarines and other foods. The cholesterol-lowering effect appears to be dose-dependent up to intakes of 3 g/day, with an average reduction in LDL-C of 12%.30 Phytosterols can also reduce triglycerides, but only in individuals with elevated triglycerides at baseline.31 A meta-analysis of RCTs concluded that plant sterol supplementation significantly increases the concentration of anti-atherogenic apolipoproteins (Apo-AI, Apo-CII) and reduces the concentration of atherogenic apolipoproteins (Apo-B and Apo-E).32
Numerous studies have demonstrated their efficacy in patients treated with statins, in which the LDL-C lowering effect is additive. Although there are fewer studies, they also appear to be effective in combination therapy with ezetimibe or fibrates.29,33
The period of consumption of plant sterols required to observe their effect is at least 2−3 weeks and, to optimise their efficacy, they should be ingested during main meals, when gallbladder contraction discharges cholesterol-laden bile into the duodenum. Plant sterols interfere with the absorption of fat-soluble vitamins (beta-carotene, lycopene, alpha-tocopherol, etc.), and a reduction in serum concentrations of these vitamins has been reported without clinical relevance. However, it is advisable to consume a diet with plenty of fruit and vegetables rich in carotenoids.33 The consumption of plant sterols is contraindicated in patients with sitosterolaemia, a rare genetic disease in which there is intestinal hyperabsorption of sterols (15%–60%, compared to 5% absorbed by healthy individuals) leading to a high concentration of plasma sterols (not cholesterol) which could be related to the severe atherosclerosis in these subjects.29
Although plant sterols at a dose of 2−3 g daily are recommended in different guidelines as an adjunct to lifestyle modification to reduce cholesterolaemia, there are no RCTs showing cardiovascular benefits.34 Nor are they likely to be conducted given the cost, complexity and time involved in clinical trials with hard cardiac CVD events as the primary outcome. However, the concept that LDL-C reduction by any mechanism is associated with cardiovascular benefit is well established.35
In conclusion, sterols and stanols are incorporated into various functional foods in an ever-expanding market because they are safe and effective ingredients for lowering LDL-C, as adjuvants to a healthy diet or to treatment with various lipid-lowering drugs.
Soluble fibreDietary fibre, resistant to hydrolysis by human digestive enzymes, is an integral component of fruits, legumes, vegetables, nuts and whole grains. There are 2 distinct types of dietary fibre defined by their water solubility: insoluble fibre, abundant in whole grains, and soluble fibre, found mainly in legumes, vegetables, fruits and oats (beta-glucans).
The cholesterol-lowering effect of soluble fibre is due to the fact that, in contact with water, it forms a gel that increases the viscosity of the food bolus, and acts as a physical barrier reducing intestinal absorption of cholesterol. In addition, soluble fibre binds bile acids in the small intestine and promotes their faecal elimination, so that hepatic cholesterol is directed towards bile acid synthesis, increasing hepatic uptake of circulating cholesterol into the plasma, with a consequent reduction in cholesterolaemia, a mechanism of action similar to that of anion exchange resins. Another beneficial mechanism of fibre is the production of short-chain fatty acids (mainly butyric and propionic acids) resulting from the fermentation of fibre by the colonic microbiome as these acids can inhibit HMG-CoA reductase, reducing hepatic cholesterol synthesis and contributing to the hypocholesterolaemic effect of soluble fibre.2
Products rich in soluble fibre, such as beta-glucan (from oats or barley), glucomannan (extract from the plant Amorphophallus konjac) and psyllium (extract from Plantago ovata), have shown beneficial effects on the lipid profile. Daily doses that have shown a cholesterol-lowering effect vary between 3 and 30 g depending on the product, achieving a reduction in LDL-C of between 7% and 15%.18,22 The addition of oat fibre to a Mediterranean diet induced a reduction in LDL-C by 15%. Intake of 10 g/day of psyllium resulted in an average LDL-C reduction of 7%, with a greater effect in individuals consuming a high-fat diet.22,36
Glucomannan is a soluble fibre derived from konjac root, which decreases cholesterol absorption in the jejunum and bile acid absorption in the ileum, and increases the activity of hepatic 7-α-hydroxylase, a key enzyme in the synthesis of bile acids from cholesterol, contributing to the reduction of cholesterolaemia. A meta-analysis shows that glucomannan (at doses between 1.2 and 15.1 g/day) significantly reduces LDL-C and triglycerides, respectively by 15.9 mg/dL and 11.5 mg/dL (p < .05 for both) on average.37
In general, tolerance to soluble fibre intake is good, except for the occurrence of gastrointestinal symptoms such as meteorism and diarrhoea that may occasionally limit adherence. Glucomannan intake may reduce the absorption of fat-soluble vitamins, calcium and lipophilic drugs, so it is recommended to separate its intake from that of this compound.18,22
Red yeast riceRed yeast rice (Monascus purpureus) has been used as a dye, preservative, flavouring and as a remedy in traditional Chinese medicine to improve blood circulation. Rice fermented by the yeast takes on a reddish hue produced by pigments resulting from fermentative metabolism. It contains monacolin, a compound with a chemical structure similar to lovastatin and a cholesterol-lowering action through inhibition of HMG-CoA reductase,18 and other compounds such as plant sterols, isoflavones and monounsaturated fatty acids, with a potential beneficial effect on the lipid profile.38
Red yeast rice comes in capsule form (it is a nutraceutical, not a functional food) and its lipid-lowering efficacy is directly related to the amount of monacolin K it contains.39 Consumption of between 3 and 10 mg/day of monacolin K results in a 10%–25% reduction in LDL-C, which is accompanied by similar reductions in total cholesterol, apolipoprotein B, and high-sensitivity C-reactive protein. In a Chinese RCT involving 1445 subjects with a history of acute myocardial infarction, red yeast rice supplementation for 4 years versus placebo showed a reduction in the risk of ischaemic heart disease (31%; p = .04), all-cause mortality (31.9%; p = .01) and stroke (44.1%; p = .04), with a good safety profile.41
In general, the consumption of red yeast rice has few associated risks. In a meta-analysis, there was no increased risk of muscle symptoms with monacolin treatment. Monacolina.42 However, since monacolin is structurally identical to a synthetic statin, the use of high doses can cause myalgia in people intolerant to statins.40 In fact, recently the European Commission has established a limit concentration level of 3 mg of monacolin K per daily dose.43
Monacolin inhibits the activity of CYP P450 and P-gp enzymes. Therefore, the concomitant use of red yeast rice with strong inhibitors of CYP3A4 (imidazole antifungals, macrolides, protease inhibitors…) or CYP1A2 (for example, verapamil) may increase the risk of adverse reactions,42 which makes their association inadvisable, especially with high doses.
A potential danger of consuming red yeast rice in nutraceuticals is the lack of standardization of some of the preparations, which may present different concentrations of monacolin K. To avoid the use of low-quality products, companies that market nutraceuticals with monacolin K should list all the substances they contain and their doses.18
Other nutraceuticalsOther nutraceuticals such as green tea, which can interfere with the intestinal absorption of cholesterol, garlic, soy protein and spirulina have cholesterol-lowering effects, although with a lower level of evidence and/or efficacy than those described above.2 Also, artichoke leaf (Cynara colymus, Cynara cardunculus) extract can reduce cholesterolaemia through the inhibition of HMG-CoA reductase by the luteolin it contains.18 Finally, policosanols, used alone or in combination with other nutraceuticals, are a mixture of long-chain alcohols isolated from sugar cane wax. Although the initial clinical studies carried out by Cuban groups showed positive effects on the lipid profile, more recent RCTs, well controlled and carried out in Caucasian populations with hypercholesterolaemia, have not confirmed any benefits, either in monotherapy at doses between 10 and 80 mg/day or combined with statins.44
Combinations of nutraceuticals in hypercholesterolaemia managementThe combination of several nutraceuticals in a single formulation leads to obtaining a polypill, with several theoretical advantages. The first is greater colesterol-lowering efficacy, with a reduction in LDL-C concentrations, which range between 5% and 25%. Secondly, associating the combination with an already prescribed pharmacological therapy could avoid adding a second drug or using lower doses of it, minimizing the risk of side effects, improving adherence and avoiding the use of more expensive drugs, such as PCSK9i., offering cost-effective control. The basic principle of combinations of nutraceuticals is that each of them has a different hypolipidaemic action to achieve a synergistic effect, in such a way that, with lower doses than those used of each of them separately, a similar cholesterol-lowering effect is achieved. Furthermore, by consuming smaller amounts of a nutraceutical, an attempt is made to reduce the occurrence of adverse effects.22 A systematic analysis that provides accurate information on the effectiveness of nutraceuticals is a recent meta-analysis of 148 studies that included 13,062 participants. In it, the cholesterol-lowering effect of these products was compared, in isolation and in different combinations. The association of red yeast rice rich in monacolin K with berberine was the most effective and this effect was not modified with the addition of policosanols.45
Regarding the results obtained in RCT, the only nutraceutical formulation with class I evidence is a product that includes a combination of berberine (500 mg), red yeast rice (200 mg, including 2.8 mg of monacolins), policosanols (10 mg), coenzyme Q10 (2 mg), astaxanthin (.5 mg) and folic acid (.2 mg), although the only components of this combination that have been shown to be effective in reducing LDL-C are berberine and red yeast rice. This product was evaluated in the context of a low-fat diet in a parallel RCT of 16 weeks duration, carried out in 751 patients with moderate hypercholesterolaemia in 248 centres in Italy. A reduction in total cholesterol of 19.1% was observed in the nutraceutical group associated with the diet compared to 9.4% in the group with the isolated diet (p < .001), with a reduction in LDL-C of 23.5% compared to 10.8% (p < .001) and triglycerides of 17.9% compared to 11.3% (p < .001) respectively, with an increase in HDL-C of 4% compared to 1.6% (p < .001).46 The doubt remains as to whether this product is more effective than one of its isolated components, red yeast rice. Although there are no clinical trials in which both have been compared directly, in a review that collects data from several meta-analyses, it was shown that the product derived from the combination of 6 components containing red yeast rice with a dose of monacolin K of 3 or 10 mg reduced LDL-C by 15% and 25%, respectively. In turn, in the existing RCTs, the isolated red yeast rice used with the same doses of monacolin K, 3 and 10 mg, reduced LDL-C identically, 15% and 25% respectively.
In conclusion, consumption of the product containing 6 nutraceuticals (with the recommended amount of monacolins K of less than 3 mg/day) has a colesterol-lowering effect significantly greater than that of a low-fat diet. However, there are no RCTs that demonstrate that this combination, containing red yeast rice equivalent to 3 mg of monacolins, is more effective than the use of isolated red yeast rice, with the same monacolin content.
The degree of scientific evidence for the use of combined therapy of functional foods or nutraceuticals with statins or ezetimibe is limited, given that the existing clinical trials are scarce, with populations of small sample size, short duration, variegated design and suffer from frequency of low systematisation in the doses of nutraceuticals used. The result of all of this is that the scientific quality of the information we have is not optimal.
Functional foods and nutraceuticals whose lipid effects have been examined in combination therapy with lipid-lowering drugs are berberine, soluble fibre, plant sterols, bergamot, red yeast rice and mixtures of several of these, especially berberine and red yeast rice. Berberine, which in monotherapy is attributed with an LDL-C reduction capacity of between 20 and 50 mg/dL, has been used in combination with statins, although few clinical trials exists and they are of low methodological quality, which has prevented a meta-analysis from being carried out. There is a systematic study of 4 RCTs with berberine, all carried out in China, and published in little-known journals in that country. Berberine added to low or moderate doses of statins resulted in an additional decrease in total cholesterol of 10.4 mg/dL and LDL-C of 4.25 mg/dL, with an increase in HDL-C of 7.7 mg/dL. dL.47 In an RCT designed to examine the effect of soluble fibre added to statins, 68 participants were randomized into 3 groups. They received treatment for 8 weeks with simvastatin 20 mg associated with placebo, simvastatin 10 mg associated with placebo, or 10 mg of simvastatin associated with 15 g of psyllium. The combination of simvastatin with soluble fibre had the same efficacy in reducing LDL-C as monotherapy with 20 mg of simvastatin.48 Similar data were obtained in another RCT with 36 volunteers, randomized for 4 weeks to receive 10 mg of lovastatin associated with 15 g of psyllium or 20 mg of lovastatin in monotherapy. The benefit was the same in both groups of participants.49 In another RCT, 30 g of total fibre (equivalent to 6 g of soluble fibre) associated with 40 mg of rosuvastatin was compared with statin monotherapy. The result was a similar decrease in LDL-C in both groups, which would indicate that the additive effect is only evident when soluble fibre is associated with low or moderate intensity statins.50 Another nutraceutical, bergamot (1 g daily), was studied in association with 10 mg of rosuvastatin, compared with 20 mg of rosuvastatin in monotherapy. The regimen in which the nutraceutical was included was accompanied by a 53% decrease in LDL-C, similar to that obtained with 20 mg rosuvastatin monotherapy. The decrease in triglycerides and the increase in HDL-C were greater with the presence of the nutraceutical.51
Regarding the combination therapy of statins with phytosterols or stanols, data from a meta-analysis of 15 RCTs comprising a total of 500 participants indicate that phytosterols/stanols at doses of 2−3 g/day, in combination with statins, compared with statins in monotherapy, produce significant additional reductions in total cholesterol and LDL-C of 11.6 mg/dL (95% CI, −13.5 to −9.7), without changes in HDL-C or triglycerides.52 Therefore, the colesterol-lowering effect of phytosterols/stanols added to statins is similar to that of these functional foods administered alone. Taken together, and in the absence of more information, the available studies indicate that the nutraceuticals studied could be used to reduce the dose of statins by half.
Other studies have examined the efficacy of various combinations of nutraceuticals associated with different lipid-lowering therapies. In one of them, carried out in 45 people with diabetes mellitus and hypercholesterolaemia with intolerance to statins, berberine (500 mg/day) and silymarin (105 mg/day) were associated. The participants were distributed into 3 groups: those who had abandoned previous treatment with statins, those who had stopped statins but started treatment with ezetimibe, and those who had reduced the dose of statins to tolerance. In all of them, an additional decrease in LDL-C was observed at 6 months, which was 15% in the statin group, 20% in the ezetimibe group, and 17% in the control group that only received nutraceuticals. Tolerance was good in all cases.53 In another RCT, statins at moderate doses were compared against an association of ezetimibe, red yeast rice (200 mg/day, containing 3 mg of monacolines), berberine (500 mg) and policosanol (10 mg), in 26 patients with FH who refused statins. The efficacy on LDL-C was similar in both groups, which implies that the combination of ezetimibe with nutraceuticals, in these individuals, achieves an effect similar to moderate doses of statins.54
Of all the combinations of nutraceuticals, the most studied is the one already mentioned, which includes berberine (500 mg), red yeast rice (200 mg, including 2.8 mg of monacolines), policosanols (10 mg), coenzyme Q10 (2 mg), astaxanthin (.5 mg) and folic acid (.2 mg). The effectiveness of this product associated with ezetimibe, statins or multiple therapy has been studied in 3 RCTs carried out by the same group of researchers, with certain limitations, such as the use of different types and doses of statins or the lack of control groups in some of them. Each one was carried out in 100 patients with ischaemic heart disease intolerant to statins, and with diverse designs. In one of them they were randomized to receive treatment with ezetimibe or the aforementioned combination of nutraceuticals. At 3 months, only 14 of the participants in the nutraceutical group reached the LDL-C goal ≤ 100 mg/dL. Ezetimibe was then added to the nutraceutical combination for the 86 participants who had not reached this goal, so that the LDL-C goals were achieved in 58 of the 86 participants (72.5%) after one year.55 A second RCT was carried out in 100 patients with coronary heart disease, similar to the previous ones and who had not achieved a 50% decrease in LDL-C with low doses of statins. Fifty of them were randomized to continue with the same doses of statins (10−20 mg/day of simvastatin or 5−10 mg/day of atorvastatin or 5 mg/day of rosuvastatin) and the remaining 50 began treatment with the same dose of statin in combination with the same combination of nutraceuticals. At 3 months, 68% of those treated with the combination reached the goal of LDL-C< 70 mg/dL, while no patient in the control group, with low doses of statins in monotherapy, achieved it. Three patients in each group had to drop out due to mialgia.56 The remaining 36 patients who did not reach the goal (<70 mg/dL LDL-C) were started on triple therapy with low-dose statins, ezetimibe, and nutraceuticals, with 28 of them reaching the previously indicated LDL-C goal at 6 months. To sum up, 92% were controlled with double or triple therapy, with few notable side effects.57 Finally, in a study by another group of researchers, carried out in 30 patients with FH on stable treatment with statins at the maximum tolerated doses, in monotherapy or associated with ezetimibe, the addition of the nutraceutical containing berberine, policosanol and red yeast rice induced a slight additional effect of reduction of total cholesterol, LDL-C, non-HDL-C and triglycerides of 8.1%; 10.5%; 9.7% and 5.4%, respectively.54
In short, the available studies that explore the cholesterol-lowering effect of different functional foods or nutraceuticals in combination with statins or ezetimibe are scarce, variegated in design, include few participants, and are published in journals that are not always of proven quality. In general, these studies confirm the capacity of the functional foods and nutraceuticals reviewed in this work to reduce LDL-C in a similar way to that of statin dose doubling. The tolerance described is generally good, but the lack of replication of the studies and the aforementioned methodological limitations prevent these treatments from being recommended with sufficient certainty. Results need to be confirmed by improving the methodology and size of the populations studied. Regarding the combinations of various nutraceuticals, the most studied is that of berberine and red yeast rice, which is marketed together with other components. With all their limitations, the results of the existing RCTs would support the cholesterol-lowering effect of the combination and its good tolerance, offering an alternative to high doses of statins when combined with ezetimibe and/or moderate doses of statins. The lack of clinical evidence studies forces us to be cautious with its recommendation.
Recommendations by different scientific societiesCurrently, there is no internationally accepted consensus on the role of functional foods and nutraceuticals in the treatment of hypercholesterolaemia. However, the positioning of the main scientific societies is briefly reviewed.
The latest version of the 2019 guidelines of the European Society of Cardiology (ESC)/European Artherosclerosis Society (EAS) for the treatment of dyslipidaemia summarises the existing evidence on the most effective functional foods and nutraceuticals for the treatment of hypercholesterolaemia.9 According to these guidelines, with the aim of achieving the LDL-C target and given that there are no contraindications derived from their safety, "plant sterols/stanols can be considered: (a) in individuals with high cholesterol concentrations with an intermediate or low overall risk of CVD, not meeting the requirements for pharmacotherapy; (b) as a complement to pharmacological treatment in patients at high and very high cardiovascular risk who do not reach LDL-C goals with statins or who cannot be treated with statins; and (c) in adults and children (>6 years) with FH. These guidelines also point out that "nutraceuticals containing purified red yeast rice are an option to consider in people with high cholesterol concentrations who do not meet the indication for treatment with statins in view of their overall cardiovascular risk".9
The approach of the U.S.A. recommendations is different. In the 2018 guideline of the AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA, nutraceuticals are not mentioned and the importance of paying special attention to the diet58 is only mentioned in passing. In 2018, the International Lipid Expert Panel (ILEP) published a position paper defining the use of nutraceuticals in the management of statin intolerance.46 In this case it is established that "nutraceuticals, such as red yeast rice, bergamot, berberine, artichoke, soluble fibre and plant sterols and stanols alone, in combined treatments or associated with ezetimibe, could be considered a lipid-lowering alternative or an additional therapy to statins.”46
The ESC 2021 guideline on CVD prevention in practice indicates the potential benefit of nutraceuticals, noting that “their use could improve the quality of lipid-lowering treatment, including therapeutic compliance and achievement of LDL-C goals in clinical practice.” 59 However, the ESC document warns about the lack of evidence showing that nutraceuticals prevent morbidity and mortality from CVD. Therefore, they are positioned on their usefulness as a possible treatment option in mild dyslipidaemia, indicating the low level of evidence regarding its benefit on cardiovascular clinical episodes.
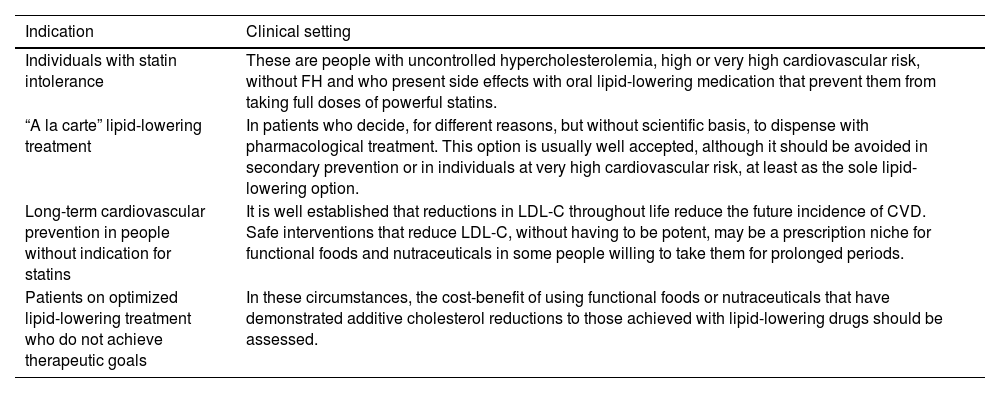
Recommendations by the Spanish Society of ArtherosclerosisThe SEA emphasizes that there are no cardiovascular morbidity and mortality studies with nutraceuticals or functional foods, and that there are few or limited long-term safety data. Both aspects should be discussed with the patient before proceeding to recommend their use. Likewise, it is understood that the functional foods and nutraceuticals that have the greatest amount of scientific evidence are phytosterols and red yeast rice. According to the data reviewed, the SEA considers that the use of nutraceuticals could be recommended in the following situations (Table 2).
Potential clinical usefulness of functional foods and nutraceuticals in people with hypercholesterolaemiaa.
| Indication | Clinical setting |
|---|---|
| Individuals with statin intolerance | These are people with uncontrolled hypercholesterolemia, high or very high cardiovascular risk, without FH and who present side effects with oral lipid-lowering medication that prevent them from taking full doses of powerful statins. |
| “A la carte” lipid-lowering treatment | In patients who decide, for different reasons, but without scientific basis, to dispense with pharmacological treatment. This option is usually well accepted, although it should be avoided in secondary prevention or in individuals at very high cardiovascular risk, at least as the sole lipid-lowering option. |
| Long-term cardiovascular prevention in people without indication for statins | It is well established that reductions in LDL-C throughout life reduce the future incidence of CVD. Safe interventions that reduce LDL-C, without having to be potent, may be a prescription niche for functional foods and nutraceuticals in some people willing to take them for prolonged periods. |
| Patients on optimized lipid-lowering treatment who do not achieve therapeutic goals | In these circumstances, the cost-benefit of using functional foods or nutraceuticals that have demonstrated additive cholesterol reductions to those achieved with lipid-lowering drugs should be assessed. |
CVD, cardiovascular disease; FH, familial hypercholesterolemia; LDL-C, LDL cholesterol.
Although individual intolerance to statins is a frequently questionable fact, the reality is that a significant number of patients present intolerable side effects, real or fictitious, with these drugs. In a recent meta-analysis, statin intolerance was analysed in a total of 176 studies (112 RCTs and 64 cohort studies) with a total of 4, 143,517 patients.60 Its global prevalence was 9.1% (95% CI, 8.0–10%), being higher in primary prevention, women, older people and patients with obesity or diabetes. The indication for using nutraceuticals would be in individuals with a high or very high cardiovascular risk, including patients with established CVD and/or FH, who present intolerable side effects to conventional medication (almost always statins), which would prevent them from achieving therapeutic goals. These patients should be carefully informed of the importance of taking lipid-lowering drugs to reduce the rate of cardiovascular complications, as well as the questionable nature of intolerance to statins. If intolerance persists, existing lipid-lowering drugs (iPCSK9, ezetimibe, bempedoic acid, resins, etc.) that have been well tolerated should be combined with the maximum tolerated dose of the statin, or with statin regimens every other day or every several days. An attempt should also be made to achieve acceptance of iPCSK9 in those patients who do not strictly comply with the indications approved by the Spanish Medicines Agency (AEMPS). In any case, many of these patients are able to tolerate statins in the future, and should therefore be periodically re-evaluated.
If the therapeutic objectives are not achieved with the indicated strategies, there could be an indication to start treatment with nutraceuticals and evaluate their tolerance, mainly phytosterols and/or red yeast rice, associated or not with other compounds.
“A la carte” lipid-lowering treatmentOne of the characteristics of healthcare today is the responsibility of the patient themself in making decisions that affect their health, including taking medications. For different reasons, often legitimate, but without scientific basis, some patients decide to dispense with a certain pharmacological treatment and opt for other therapeutic measures. There is strong media pressure, especially on social networks, calling into question the effectiveness and safety of conventional lipid-lowering medication. If after reasoned scientific information about the usefulness of lipid-lowering drugs the individual persists in their refusal to take them, functional foods and nutraceuticals could be a therapeutic alternative, and are usually well accepted.61 However, this indication should be avoided in patients undergoing secondary prevention or at very high cardiovascular risk, at least as the sole lipid-lowering option.
Long-term cardiovascular prevention in people without indication for lipid-lowering treatmentThe lipid-lowering treatment recommendations of the main scientific societies limit pharmacological treatment to those individuals at high cardiovascular risk in the medium term or to those who have very high LDL-C concentrations.58,62,63 However, it is well established that maintaining low LDL-C throughout life has a large impact on the rate of cardiovascular complications, as has been seen in people with loss-of-function genetic variants in PCSK9.12,64 Safe, but low-potency, interventions that reduce LDL-C may be a prescription niche for nutraceuticals in people willing to purchase and take them for long periods.
Patients on optimised lipid-lowering treatment who do not achieve therapeutic goalsUnder these circumstances, the cost-benefit of using nutraceuticals that have demonstrated additive cholesterol reductions to those achieved with lipid-lowering drugs should be assessed. As already noted, red yeast rice and plant sterols or stanols have recognized but limited effectiveness in this situation.
FundingThis document was prepared independently and was not funded by any pharmaceutical company or corporation.
Conflict of interestsPP-M received fees for scientific advice, lectures and educational activities from Ferrer, Novo-Nordisk, Boehringer Ingelheim, Amgen, Esteve, Menarini, Daiichi-Sankyo, Servier and Viatris. ER received scientific consulting fees from Alexion and the California Walnut Commission. JP-B received fees for speaking engagements and educational activities from Amarin, Amgem, Daiichi-Sankyo, Esteve, Ferrer, MSD, Sanofi, and Viatris. FC received fees for speaking engagements and educational activities from Ferrer, Amgen, Sanofi, and Novartis. VP-F received fees for lectures and educational activities from Adamed, Amarin, Almirall, Astra-Zeneca, Daichii-Sankyo, Esteve, Ferrer, Novartis, Sanofi-Aventis, Servier, Viatris. CG does not receive fees for conferences or training activities from the pharmaceutical or food industry. RS received fees for educational activities from Viatris and scientific projects with Rottapharm/Madaus. FP-J does not receive fees for conferences or training activities from the pharmaceutical or food industry. JMM received fees for speaking engagements and educational activities from Amgen, Sanofi, Novartis, Ferrer, Daiichi Sankyo, Servier, and Viatris.