Comprehensive biopsychosocial care for people with gender incongruence (ICD 11) who are transgender (trans) or gender diverse is a complex process in which the quality of the medical transition can only be guaranteed after a multidisciplinary approach, through teams that integrate professionals with training and experience not only in medicine but also in diversity and gender identity. Based on this, the Gonad, Identity and Sexual Differentiation working group of the Spanish Society of Endocrinology and Nutrition (GT-GIDSEEN) has established minimum care requirements that aim to guarantee adequate health care for these people by professionals. A position paper has been produced and is available at https://www.seen.es/portal/documentos/estandares-calidad-gidseen-2024.
La atención biopsicosocial integral a personas con incongruencia de género (CIE 11) transgénero (trans) o de género diverso, es un proceso complejo en el que sólo se puede garantizar la calidad de la transición médica tras un abordaje multidisciplinar, mediante equipos que integren a profesionales con formación y experiencia no solo en medicina sino también en diversidad e identidad de género. En base a ello, el grupo de trabajo de Gónada, Identidad y Diferenciación Sexual de la Sociedad Española de Endocrinología y Nutrición (GT-GIDSEEN) ha establecido unos requisitos asistenciales mínimos que pretenden garantizar una adecuada atención sanitaria a estas personas por parte de los profesionales. Se ha realizado un documento de posicionamiento que puede consultarse en https://www.seen.es/portal/documentos/estandares-calidad-gidseen-2024.
Health care during gender transition for people with sexual and gender diversity should be based on the following general principles 1–3:
- 1
Respect for free gender self-determination (endorsed in Código de Deontología Médica 2022, chapters 67.1 and 67.2, and in compliance with the International Declaration of Human Rights).
- 2
Avoidance of pathologisation or "psychiatrisation" of trans realities (ICD 11).
- 3
Evaluation of the demand and psychological support, especially in minors, together with supportive psychotherapy in cases where it is required.
- 4
Exploration of alternative psycho-educational pathways in mutual agreement with the user.
- 5
Autonomy in decision-making (Law 41/2002 on patient autonomy).
- 6
Adequately informed consent.
- 7
Comprehensive and high-quality healthcare support according to the best existing international standards and the maximum possible scientific evidence.
- 8
Rights-based and equitable health care provided by expert professionals with certified training in identity.
- 9
Community-based care without segregation and without losing quality.
Currently, in the Spanish State there is great heterogeneity and fragmentation in the organisation of health care for people with sexual and gender diversity.4,5 In addition, users demand community-based health care provided by qualified and experienced specialists.6 Based on the above, the Spanish Society of Endocrinology and Nutrition (Sociedad Española de Endocrinología y Nutrición, SEEN) has considered it necessary to establish minimum care requirements that guarantee adequate health care by endocrinologists, without generating disparities between individuals and territories.
Given the significant increase in the demand for experienced health care in our country.7 and regardless of the existence of regional-level reference units, the emergence of specialised consultation units in endocrinology and nutrition services aimed at supporting trans people is becoming increasingly frequent. In these consultation units or care units, there are not always uniform criteria that allow for the provision of rights-based health care in accordance with minimum quality standards, which is why this document is particularly necessary.
The following recommendations aim to improve health care for trans people in Spain and are not intended to interfere with the organisation of existing regional health care networks.
In order to achieve this goal, the following is deemed necessary:
- -
To establish minimum quality standards to serve as a guide for endocrinology professionals.
- -
To unify guidelines for action and treatment in the care of trans people with a view to reducing variability among practices in different areas of care.
- -
To ease and promote the development of new care units by establishing collaborative care networks.
- -
To encourage the collection of care activity data at the national level.
- -
To ensure the appropriate training and skills of professionals in different units.
- -
To promote teaching in the area of transgender medicine and collaborative research among units.
This document does not refer directly to paediatric units, which should have much more specific considerations and requirements and, therefore, will not be analysed. It is only proposed that, if paediatric care is available at a given centre, then close collaboration among paediatricians and endocrinologists should be forged, and transition from paediatric to adult care should be made easier by means of specific protocols.
MethodologyThe GT-GIDSEEN has outlined a set of criteria and quality standards in health care of trans people, after reviewing the documents covering general principles of health care for these people,1–3 as well as existing scientific literature on the subject, especially in relation to our country,3–7 classified according to the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) model.8 In addition, experience gained in the main national reference centres has also been considered. It is acknowledged that the regional protocol should be followed and taken into account on an individual basis, but efforts should be made to maintain, as much as possible, a uniform model in our actions. A position paper and supporting presentation have been drafted and are available at https://www.seen.es/portal/documentos/estandares-calidad-gidseen-2024.
Types of unitsConsidering the growing demand for high-quality community-based health care as well as the geographical dispersion in most Autonomous Communities, it has been deemed useful to define two types of care units. By working as a network and in coordination with reference units, where they exist, they will be able to provide community-based care without losing quality. These care units belong to two types depending on the quality standards they achieve: (1) basic or elementary care units and (2) excellent care units.
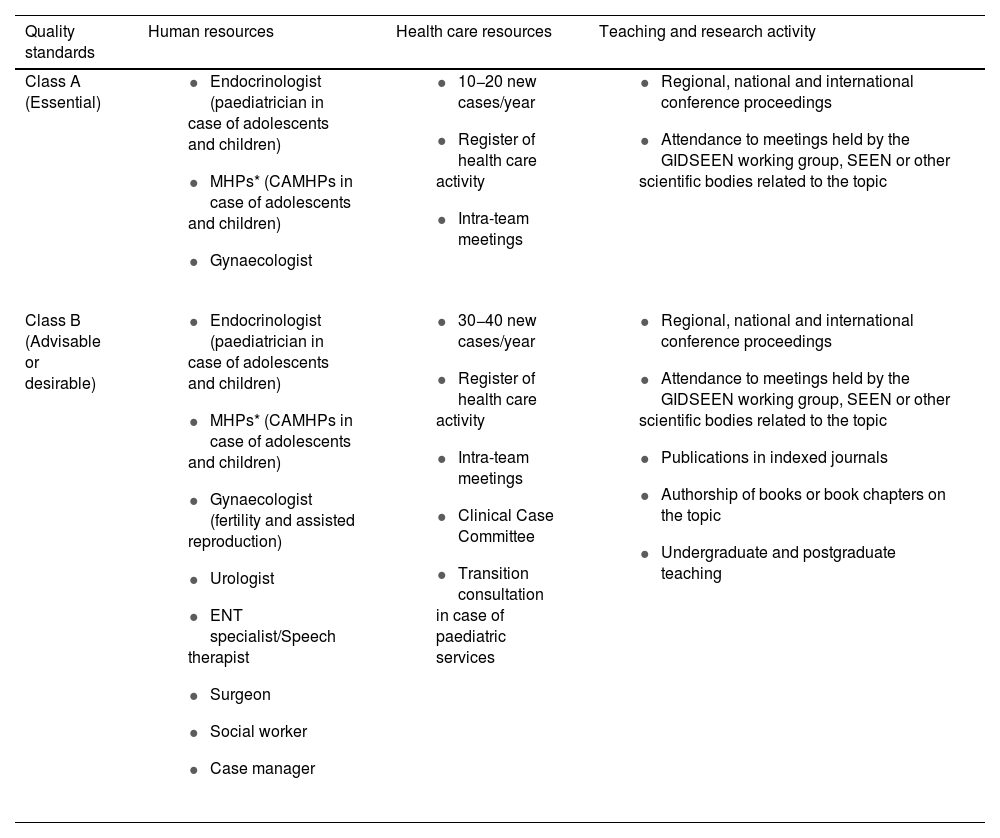
Quality standards and criteriaAdopted standards refer to human resources, health care resources and teaching and research activities, and they are grouped into two types: Class A and Class B. Class A standards are regarded as essential or basic, whereas Class B standards are advisable or desirable.
Tables 1 and 2 specify the quality standards and criteria that should be met by transgender care units. Some standards differ depending on the existence of paediatric services at a given centre.
Types of resources and quality standards.
| Quality standards | Human resources | Health care resources | Teaching and research activity |
|---|---|---|---|
| Class A (Essential) |
|
|
|
| Class B (Advisable or desirable) |
|
|
|
MHP: Mental Health Professional.
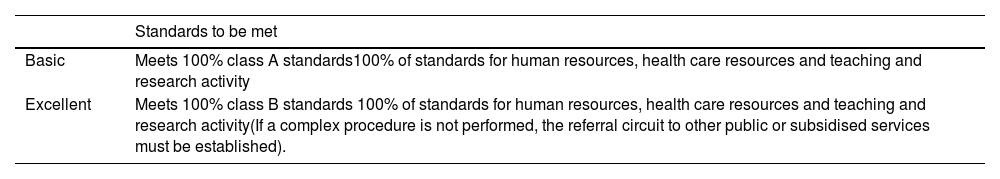
Type of care units proposed according to compliance with standards.
| Standards to be met | |
|---|---|
| Basic | Meets 100% class A standards100% of standards for human resources, health care resources and teaching and research activity |
| Excellent | Meets 100% class B standards 100% of standards for human resources, health care resources and teaching and research activity(If a complex procedure is not performed, the referral circuit to other public or subsidised services must be established). |
Endocrinological care for trans people must be carried out within multidisciplinary teams of experts and must be based not only on strictly medical aspects but also on psychoeducational and social aspects (level of evidence: low).1–3 Only in this way can we guarantee that our procedures improve quality of life for these people, which will be the ultimate goal of our actions. Care must be comprehensive and holistic. For this, psychosocial aspects shall be concurrently addressed if required. This is all the more true when it comes to young or vulnerable populations.
Endocrinology professionals should receive adequate training in gender diversity care (level of evidence: low1 by taking a master's degree or postgraduate degree issued by a university or a specific scientific society. Otherwise, they should complete training in continuing education activities provided by relevant scientific societies. The position document sets out the current portfolio of professional education activities in Transgender Medicine as well as the most relevant references for clinical practice (https://www.seen.es/portal/documentos/estandares-calidad-gidseen-2024). In turn, it is recommended to be an active member of the GT-GIDSEEN.
Mental health professionals (MHPs) should be certified and experienced in gender identity (level of evidence: low).1 Their vision should be non-pathologising and their support should be extended to families who require or request it (level of evidence: low).1 They must be qualified to inform, support and assist throughout the transition process (Law 4/2023, of February 28, Article 59, https://www.boe.es/eli/es/l/2023/02/28/4). In cases with confounding situations, working together with the MHP will be the best guarantee that our actions will benefit the user.
Gynaecological professionals should be aware of the key characteristics of screening and management of gynaecological pathologies in transgender men and transgender women with vaginoplasty (level of evidence: low).1 Furthermore, they must be experienced in performing hysterectomy and double adnexectomy. In order to meet Class B standards, subjects should be counselled on fertility preservation and assisted reproduction techniques, which must be performed in the relevant unit. Otherwise, practitioners must know the procedures and participate in the process of assigning the most complex techniques to external centres with greater experience or to subsidised private centres.
Urology professionals should be aware of the key characteristics of screening and management of prostate pathologies in transgender women (level of evidence: low).1 Moreover, they should be willing to perform orchidectomy in cases where appropriate.
ENT professionals must be familiar with the process of voice feminisation with speech therapy support (level of evidence: low).1 In order to meet Class B standards, at least voice feminisation activities should be performed.
Plastic surgeons must be experienced in chest masculinisation surgery and augmentation mammoplasty (level of evidence: low).1 In order to meet Class B standards, plastic surgery practitioners should perform genital reassignment surgery techniques. If they do not perform these surgeries themselves, then they should be aware of the procedures and participate in the process of assigning them to external centres.
It is also advisable to have the assistance of social work specialists with specific training who can provide support if necessary (level of evidence: low) (expert recommendation).
A case manager or a member of the unit shall be in charge of organizing reception protocols and scheduling multidisciplinary clinical coordination meetings.
Health care resourcesWith regard to the health care activity and in order to ensure an adequate level of experience, the number of subjects to be treated according to Class A standards will be 10−20 new cases per year, including the follow-up of known cases, based on the population in the health area. According to Class B standards, the recommended minimum number of new cases per year will be 30−40, including the follow-up of known cases, except for subjects who wish and/or can be followed up in a basic level unit (level of evidence: low) (expert recommendation).
In order to provide rights-based and high-quality health care, it is necessary to develop clinical management tools such as those described below (level of evidence: low) (expert recommendation):
- 1
Intra-team meetings for better clinical and administrative coordination.
- 2
A Clinical Case Committee to make decisions in complex cases.
- 3
Paediatric transition consultations if there is a paediatric service in place.
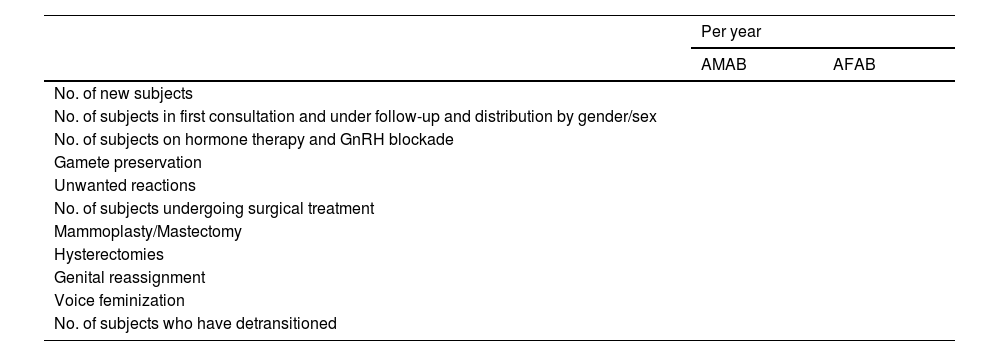
At the same time, it is recommended to keep a register of health care activity including at least the items specified in Table 3.
Minimum register of health care activity.
| Per year | ||||||
|---|---|---|---|---|---|---|
| AMAB | AFAB | |||||
| No. of new subjects | ||||||
| No. of subjects in first consultation and under follow-up and distribution by gender/sex | ||||||
| No. of subjects on hormone therapy and GnRH blockade | ||||||
| Gamete preservation | ||||||
| Unwanted reactions | ||||||
| No. of subjects undergoing surgical treatment | ||||||
| Mammoplasty/Mastectomy | ||||||
| Hysterectomies | ||||||
| Genital reassignment | ||||||
| Voice feminization | ||||||
| No. of subjects who have detransitioned | ||||||
AMAB (assigned male at birth); AFAB (assigned female at birth); GAHT (gender-affirming hormone therapy).
On the other hand, units should have a protocol for the care of people with sexual and gender diversity. This should be written and signed by the professionals who are responsible for the unit, as well as the centre managers, and endorsed by the regional-level competent authorities. Such protocol should include the entire process of care provided to these subjects in the unit (level of evidence: low) (expert recommendation):
- -
Referral circuit from primary care.
- -
Referral circuit among specialities.
- -
Health care activity to be carried out in the first consultation or reception consultation.
- -
Health care activity to be carried out in the second consultation (indications and contraindications for gender-affirming hormone therapy and pubertal blockade with GnRH analogues, together with a description of guidelines, according to national consensus and clinical practice guides) and subsequent consultations. It is recommended that the clinical guidelines used have the highest level of evidence available at any given time and can be adapted to the specific characteristics of each centre or health system.
- -
Fertility techniques conducted in the unit should be specified.
- -
The number and type of surgeries undertaken in the unit should be specified.
- -
There should be informed consent or waiver forms to be signed, as well as documents covering psychological evaluation, use of GnRH analogues, gender-affirming hormone therapy, surgical interventions or fertility preservation techniques. These must be validated by the competent official body.
- -
Adequately informed consents must be signed after an adequate and detailed assessment of each individual case, weighing the risks and benefits of all actions required for the transition. General informed consents are discouraged. In order for them to be valid, the existence of a minimum capacity for judgement must be ensured, but this is sometimes difficult and complex, and lies beyond the scope of endocrinology. In case of doubt and in order to guarantee the validity of such consent, the relevant specialists should be consulted. This is particularly important in the case of minors and irreversible interventions.
- -
Protocols for basic care units should include the criteria and referral circuit to excellent units, both for more complex cases and for surgeries not undertaken there.
- -
It is advisable to have specific action protocols to support people who detransition, avoiding stigmatisation and offering all the required psychological and endocrinological assistance.
- -
Basic and excellent units must be capable of periodically evaluating or auditing their results, for which the appropriate clinical management tools will be implemented.
- -
Both basic and excellent care units will provide access to social resources and support networks for those who require them.
In terms of research activity, conference proceedings/presentations at congresses and scientific meetings held by various scientific societies, as well as publications in journals and the writing of book chapters, are established as quality standards.
At the same time, it is recommended that excellent care units encourage applied clinical research projects, allowing them to evaluate the health care provided and to generate new scientific knowledge. It is suggested to disseminate them via presentations in GT-GIDSEEN and to report research results through scientific publications and conference proceedings, including the National Congress of the Spanish Society of Endocrinology and Nutrition.
In relation to teaching, it is recommended that excellent reference units collaborate on undergraduate and postgraduate training programmes to disseminate knowledge on transgender health (level of evidence: low) (expert recommendation). With regard to postgraduate education (especially for Endocrinology and Nutrition residents), it is the responsibility of these excellent care units to guarantee adequate training in the care of transgender people, either at the unit itself or, in its absence, at an associated teaching facility. This will ensure compliance with the Endocrinology and Nutrition specialty curriculum.
LimitationsAs these are new recommendations on the delivery of high-quality health care for subjects with sexual and gender diversity, and there is hardly any scientific literature on the subject, the level of scientific evidence according to the GRADE system is not as high as desired. However, their benefit has been objectively demonstrated in clinical practice at national reference centres. Therefore, these recommendations should not be undermined.
Conflicts of interestThe authors have no conflicts of interest.
We acknowledge the support of the Spanish Society of Endocrinology and Nutrition, as well as the contributions of the other members of the GIDSEEN group.