High-intensity interval training (HIIT) has been widely used to fight cardiovascular risk factors in adolescents and adults, but no data are available on its applicability in children.
ObjectiveTo assess the effects of HIIT on different anthropometric and cardiovascular parameters of overweight and obese children aged 7–9 years.
Subjects and methodsFour groups were formed: 1) an overweight control group (OWCG, n = 30, BMI = 21.60 ± 3.72 kg/m2), 2) an obesity control group (OCG, n = 34, BMI = 23.92) ± 3.11 kg/m2), 3) an overweight intervention group (OWIG, n = 69, BMI = 20.01 ± 1.88 kg/m2), and 4) an obesity intervention group (OIG, n = 141, BMI = 24.12 ± 2.66 kg/m2). BMI, body fat (BF), waist circumference, height-waist ratio, systolic (SBP) and diastolic (DBP) blood pressure and cardiorespiratory fitness (CRF, were assessed before and after intervention.
ResultsThere were significant differences in BMI (P < 0.001), BF (P < 0.001), and CRF (P < 0.001) between the groups (control vs intervention) before and after intervention (OWCG vs OWIG and OCG vs OIG). BMI decreased in the OWIG (BMI, 20.01 ± 1.88 at baseline vs 19.00 ± 2.02 after HIIT, P < 0.001) and OIG (BMI, 24.12 ± 2.66 at baseline vs 23.23 ± 3.23 after HIIT, P < 0.001) groups. Similarly, BF decreased in the OWIG (BF, 21.84 ± 4.97 at baseline vs 19.55 ± 4.81 % after HIIT, P < 0.001) and OIG (BF, 30.26 ± 11.49 at baseline vs 26.81 ± 6.80 % after HIIT, P < 0.001) groups. CRF improved in both intervention groups (P < 0.001). There was a significant decrease in the prevalence rate of schoolchildren with obesity (from 66.4% to 49.6%) (P < 0.001).
ConclusionThe intervention conducted in the school setting improved the anthropometric and cardiovascular parameters of schoolchildren, and also allowed for reducing the proportion of schoolchildren with obesity.
El ejercicio intervalado de alta intensidad (HIIT) ha sido utilizado ampliamente para combatir los factores de riesgo cardiovascular en población adolescente y adulta, existiendo un vacío de su aplicabilidad en población infantil.
ObjetivosDeterminar los efectos de un HIIT sobre distintos parámetros antropométricos y cardiovasculares de niños con sobrepeso y obesidad de entre 7 y 9 años de edad.
Material y métodosCuatro grupos fueron formados: 1) grupo control con sobrepeso (GCS, n = 30, IMC = 21.60 ± 3.72 kg/m2), 2) grupo control con obesidad (GCO, n = 34, IMC = 23,92 ± 3,11 kg/m2), 3) grupo intervención con sobrepeso (GIS, n = 69, IMC = 20,01 ± 1,88 kg/m2) y 4) grupo intervención con obesidad (GIO, n = 141, IMC = 24,12 ± 2,66 kg/m2). El IMC, grasa corporal (GC), circunferencia de cintura, razón cintura estatura, presión arterial sistólica (PAS), diastólica y capacidad cardiorrespiratoria (CRF), fueron evaluadas Pre y Post intervención.
ResultadosExistieron diferencias significativas en las variables IMC (P < 0,001), GC (P < 0,001) y la CRF (P < 0,001) en la comparación entre grupos (control vs intervención) en Pre y Post intervención (GCS vs GIS y GCO vs GIO). El GIS (IMC; Pre = 20,01 ± 1,88 vs Post = 19,00 ± 2,02, P < 0,001) y GIO (IMC; Pre = 24,12 ± 2,66 vs Post = 23,23 ± 3,23, P < 0,001) disminuyeron su IMC. De igual forma, en GIS (GC; Pre = 21,84 ± 4,97 vs Post = 19,55 ± 4,81%, P < 0,001) y GIO (GC; Pre = 30,26 ± 11,49 vs Post = 26,81 ± 6,80%, P < 0,001) la GC disminuyó. Ambos grupos intervenidos mejoraron su CRF (P < 0,001). Existió una disminución significativa de escolares con obesidad (Pre = 66.4%, vs. Post = 49.6%) (P < 0,001).
ConclusiónLa intervención realizada en el contexto escolar mejora los parámetros antropométricos y cardiovasculares de los escolares, permitiendo además disminuir la proporción de escolares con obesidad.
Obesity is a chronic, non-transmissible disease that is common in both developed and developing countries.1 The World Health Organization (WHO) points to childhood obesity as the most serious public health problem of the present century.2 In Chile, the National Physical Education Study indicates that 45 % of all students are overweight or obese.3 The causes of obesity include an inadequate diet, an excessively sedentary lifestyle, and insufficient physical activity levels, among others.4 In addition, childhood obesity is associated to the development of cardiovascular risk factors such as arterial hypertension and insulin resistance,5 with low cardiorespiratory fitness (CRF).6
Changes in the amount of physical activity at school have shown beneficial effects in relation to body composition, physical condition, cardiovascular health and insulin sensitivity.7 In this regard, high-intensity interval training (HIIT), which is mainly characterized by short intervals of vigorous activity separated by periods of rest or low-intensity exercise,8 has been reported to be effective in improving body composition and cardiometabolic risk factors in obese young people.9 It has also been seen to have a positive impact on vascular function10 and on CRF11 — the latter being a key component of a healthy lifestyle in children.12
The available evidence suggests that HIIT programs could be carried out in conjunction with physical education (PE) class activities or in specific periods during the school day.13 However, it is important to determine the physiological effects of HIIT in children with overweight and obesity,14 and to assess its applicability in the school setting with a view to defining it as a cost-efficient tool for combating school age obesity and its comorbidities. The present study was thus carried out to determine the effects of HIIT upon different anthropometric and cardiovascular parameters in overweight and obese children between 7–9 years of age. The study comprised an intervention with two control groups (overweight and obese) and two experimental groups (overweight and obese), in the absence of randomization.
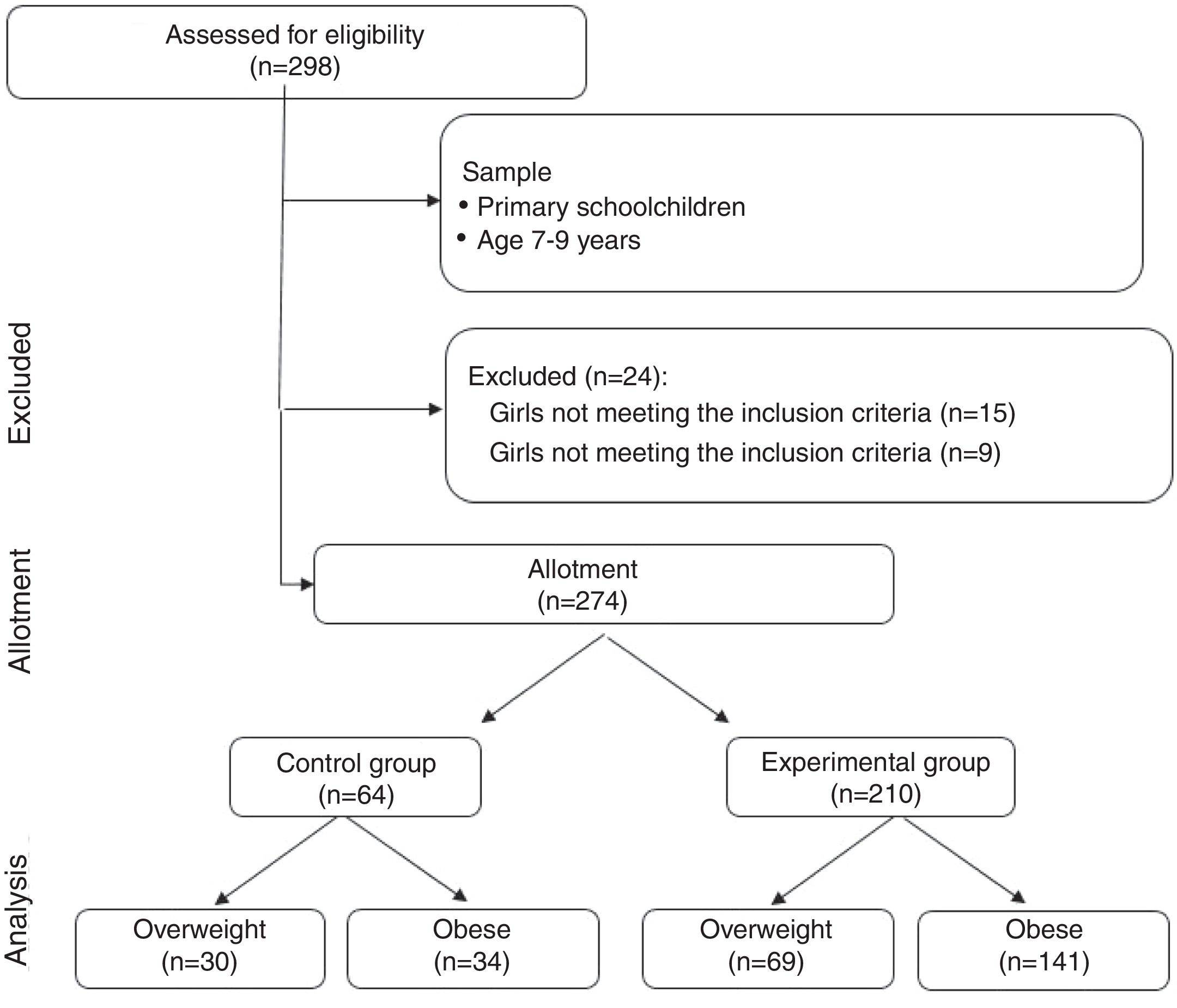
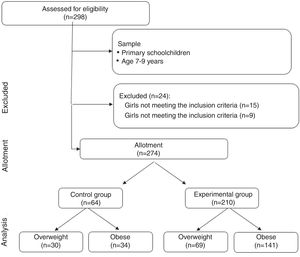
Material and methodsParticipantsStudy participation was voluntary, and nonrandomized, convenience sampling was carried out. We recruited girls (n = 154, 7.99 ± 1.47 years) and boys (n = 120, 8.29 ± 1.53 years) between 7–9 years of age in public schools of the region of Araucanía (Chile) (n = 274).
The inclusion criteria were: a) medical qualification for physical exercise; b) informed consent from the parents and also individual assent; c) registration in public school; and d) subject age 7–9 years. Exclusion criteria were: a) the presence of musculoskeletal disorders or any other medical condition that could affect the health of the participants; and b) physical, sensory or intellectual disabilities.
Four groups were established: 1) overweight control group (OWCG, n = 30, body mass index [BMI] = 21.60 ± 3.72 kg/m2); 2) obese control group (OCG, n = 34 IMC = 23.92 ± 3.11 kg/m2); 3) overweight intervention group (OWIG, n = 69, IMC = 20.01 ± 1.88 kg/m2), and 4) obese intervention group (OIG, n = 141, IMC = 24.12 ± 2.66 kg/m2) (Fig. 1). The schoolchildren in the control groups (OWCG and OCG) belonged to a public school, and the children in the two intervention groups (OWIG and OIG) belonged to two public schools.
The study abided with the principles of the Declaration of Helsinki (2013), and was approved by the Ethics Committee of Universidad de La Frontera (Temuco, Chile). All participants received verbal explanations of the program and tests before the start of the study.
Materials and proceduresAnthropometric assessmentBody mass (kg) was recorded using a scale (TANITA, model Scale Plus UM – 028, Tokyo, Japan). The children were weighed barefoot and with as little clothing as possible. Height (m) was estimated with a stadiometer (Seca®, model 214, Hamburg, Germany) graded in mm. Body mass index, defined as the ratio between body weight and height squared (kg/m2), was used to estimate the degree of obesity. Body weight status of the participants was assessed using the following CDC rating criteria according to percentile (p): overweight: BMI between p 85 and < p 95; obesity: IMC > p 95.14 Waist circumference (WC) in turn was measured using a measuring tape (Seca®, model 201, Hamburg, Germany) at navel level.15 The waist-height ratio (WHR) was obtained dividing WC by height, and was used as a tool to estimate fat accumulation in the central body region. Percentage body fat (BF) was assessed from the tricipital and subscapular folds, with use of the Slaughter formula.16
Cardiovascular assessmentSystolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured on two occasions spaced 15 min apart, under resting conditions, using widely recognized classification standards for children and adolescents.17 A digital monitoring system was used for the measurements (OMRON®, model HEM 7114, IL, USA).
Cardiorespiratory fitnessThe 6-minute walk test (6MWT) was used to evaluate cardiorespiratory fitness (CRF). This test is increasingly used in children,18 and evaluates the ability of a subject to perform physical exercise, measuring the maximum distance walked in 6 min. The 6MWT was performed in a closed space on a flat surface 30 m in length, with two reflective cones placed at either end indicating the limit of the path. The subjects repeatedly walked from one end to the other and back again. Visible marks were placed every 3 m along the path for recording of the distance walked. The test was conducted by PE teachers during the classroom hours, and motivation was provided based on the statements indicated in the protocol.
InterventionThe overweight and obese schoolchildren performed HIIT during 28 weeks (twice a week) in the course of the school period (April-October), one month after return from the summer holidays. All activities were performed in the school setting, in PE class, with a total of 56 sessions lasting 40−50 min each. The control group consisted of schoolchildren from a school other than that of the study intervention subjects, but with students of similar characteristics who performed the traditional activities of the official PE program, with low intensity activities and scant effort encouragement.19 This program alternates collective sports, dances and recreational games, in line with the Chilean national curricular specifications for PE in school.20
The exercises of the intervention groups were of high intensity, with playing as the main strategy, combined with recreational activities. Use was also made of exercise machines (bicycle, treadmill), together with activities in the open air such as running, basic motor skills in the form of jumping and throwing, with the application of strategies similar to those used in other studies.21,22
The HIIT program had two parts: 1) In the first part the stimuli lasted 30 s to 1 min, with a recovery time from 1 to 2 min, working progressively over a period of 15−20 min of the session. 2) In the second part, the stimuli lasted 4 min, with high intensity playing and a recovery time of 1−2 min (3–4 series), during 15−20 min. The activities were programmed in time and intensity following recent recommendations regarding HIIT in schoolchildren.13 The participants were asked to make physical effort equivalent to a score of 8–10 on the modified 10-point Borg scale for the pediatric population.23 The program started with a warm-up period of 5 min of running and chasing games and joint mobility exercises, and ended with 5 min of return to resting conditions.
Statistical analysisData analysis was performed using the SPSS version 23.0 statistical package (SPSS™ IBM Corp., NY, USA). Statistical significance was considered for p < 0.05. Descriptive statistics (mean and standard deviation [SD]) were calculated. Normal data distribution and the equality of variances were checked using the Kolmogorov-Smirnov test and Levene test, respectively. One-way analysis of variance (ANOVA) was performed for inter- and intra-group comparisons, and repeated measures two-way ANOVA was used to determine the effect of the intervention. Additionally, Cohen’s d test was used to determine effect size, using threshold values of ≤ 0.49, 0.50–0.79 and ≥ 0.80 for defining small, moderate and large effects, respectively.24 The observed pre- versus post-intervention differences in overall weight status were assessed using the Gamma test.
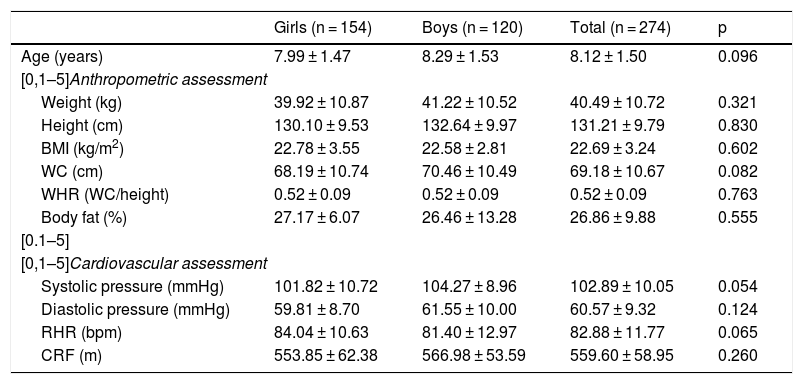
ResultsTable 1 shows the baseline characteristics of the study sample. There were no gender differences in relation to the anthropometric and cardiovascular variables (Table 1).
Baseline characteristics of the study sample.
| Girls (n = 154) | Boys (n = 120) | Total (n = 274) | p | |
|---|---|---|---|---|
| Age (years) | 7.99 ± 1.47 | 8.29 ± 1.53 | 8.12 ± 1.50 | 0.096 |
| [0,1–5]Anthropometric assessment | ||||
| Weight (kg) | 39.92 ± 10.87 | 41.22 ± 10.52 | 40.49 ± 10.72 | 0.321 |
| Height (cm) | 130.10 ± 9.53 | 132.64 ± 9.97 | 131.21 ± 9.79 | 0.830 |
| BMI (kg/m2) | 22.78 ± 3.55 | 22.58 ± 2.81 | 22.69 ± 3.24 | 0.602 |
| WC (cm) | 68.19 ± 10.74 | 70.46 ± 10.49 | 69.18 ± 10.67 | 0.082 |
| WHR (WC/height) | 0.52 ± 0.09 | 0.52 ± 0.09 | 0.52 ± 0.09 | 0.763 |
| Body fat (%) | 27.17 ± 6.07 | 26.46 ± 13.28 | 26.86 ± 9.88 | 0.555 |
| [0.1–5] | ||||
| [0,1–5]Cardiovascular assessment | ||||
| Systolic pressure (mmHg) | 101.82 ± 10.72 | 104.27 ± 8.96 | 102.89 ± 10.05 | 0.054 |
| Diastolic pressure (mmHg) | 59.81 ± 8.70 | 61.55 ± 10.00 | 60.57 ± 9.32 | 0.124 |
| RHR (bpm) | 84.04 ± 10.63 | 81.40 ± 12.97 | 82.88 ± 11.77 | 0.065 |
| CRF (m) | 553.85 ± 62.38 | 566.98 ± 53.59 | 559.60 ± 58.95 | 0.260 |
Data shown represent the mean ± SD. P-values < 0.05 were considered statistically significant.
WC: waist circumference; CRF: cardiorespiratory fitness; RHR: resting heart rate; BMI: body mass index; WHR: waist-height ratio.
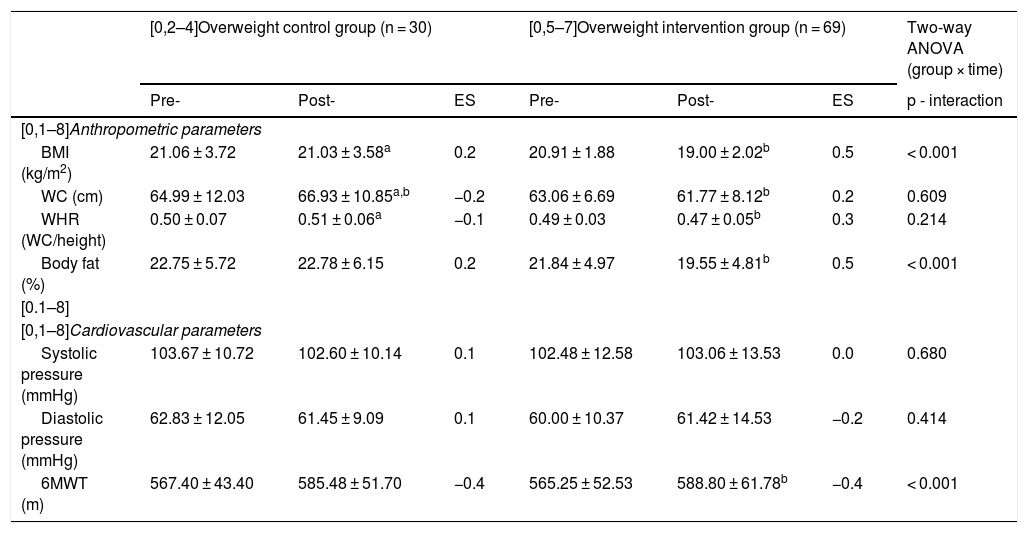
Table 2 in turn compares the overweight control and intervention groups (OWCG versus OWIG). There were no baseline differences in age, BMI, WC, WHR, BF, CRF, SBP or DBP (p > 0.05). However, two-way ANOVA revealed significant differences in the variables BMI (p < 0.001), BF (p < 0.001) and the 6MWT (p < 0.001) on comparing the control and intervention groups (pre- versus post-intervention). On the other hand, the OWIG showed significant changes in BMI (pre- = 20.01 ± 1.88 kg/m2 vs. post- = 19.00 ± 2.02 kg/m2, p < 0.001, effect size [ES] = 0.5) and BF (pre- = 21.84 ± 4.97 % vs. post- = 19.55 ± 4.81 %, p < 0.001, ES = 0.5). Likewise, CRF improved significantly (6MWT pre- = 565.25 ± 52.53 m vs. post- = 588.80 ± 61.78 m, p < 0.001, ES = 0.4).
Anthropometric and cardiovascular parameters before (pre-) and after (post-) the HIIT program in children with overweight.
| [0,2–4]Overweight control group (n = 30) | [0,5–7]Overweight intervention group (n = 69) | Two-way ANOVA (group × time) | |||||
|---|---|---|---|---|---|---|---|
| Pre- | Post- | ES | Pre- | Post- | ES | p - interaction | |
| [0,1–8]Anthropometric parameters | |||||||
| BMI (kg/m2) | 21.06 ± 3.72 | 21.03 ± 3.58a | 0.2 | 20.91 ± 1.88 | 19.00 ± 2.02b | 0.5 | < 0.001 |
| WC (cm) | 64.99 ± 12.03 | 66.93 ± 10.85a,b | −0.2 | 63.06 ± 6.69 | 61.77 ± 8.12b | 0.2 | 0.609 |
| WHR (WC/height) | 0.50 ± 0.07 | 0.51 ± 0.06a | −0.1 | 0.49 ± 0.03 | 0.47 ± 0.05b | 0.3 | 0.214 |
| Body fat (%) | 22.75 ± 5.72 | 22.78 ± 6.15 | 0.2 | 21.84 ± 4.97 | 19.55 ± 4.81b | 0.5 | < 0.001 |
| [0.1–8] | |||||||
| [0,1–8]Cardiovascular parameters | |||||||
| Systolic pressure (mmHg) | 103.67 ± 10.72 | 102.60 ± 10.14 | 0.1 | 102.48 ± 12.58 | 103.06 ± 13.53 | 0.0 | 0.680 |
| Diastolic pressure (mmHg) | 62.83 ± 12.05 | 61.45 ± 9.09 | 0.1 | 60.00 ± 10.37 | 61.42 ± 14.53 | −0.2 | 0.414 |
| 6MWT (m) | 567.40 ± 43.40 | 585.48 ± 51.70 | −0.4 | 565.25 ± 52.53 | 588.80 ± 61.78b | −0.4 | < 0.001 |
Data shown represent the mean ± SD. P-values < 0.05 were considered statistically significant.
6MWT: six-minute walk test; WC: waist circumference; HIIT: high-intensity interval training; BMI: body mass index; WHR: waist-height ratio; ES: effect size.
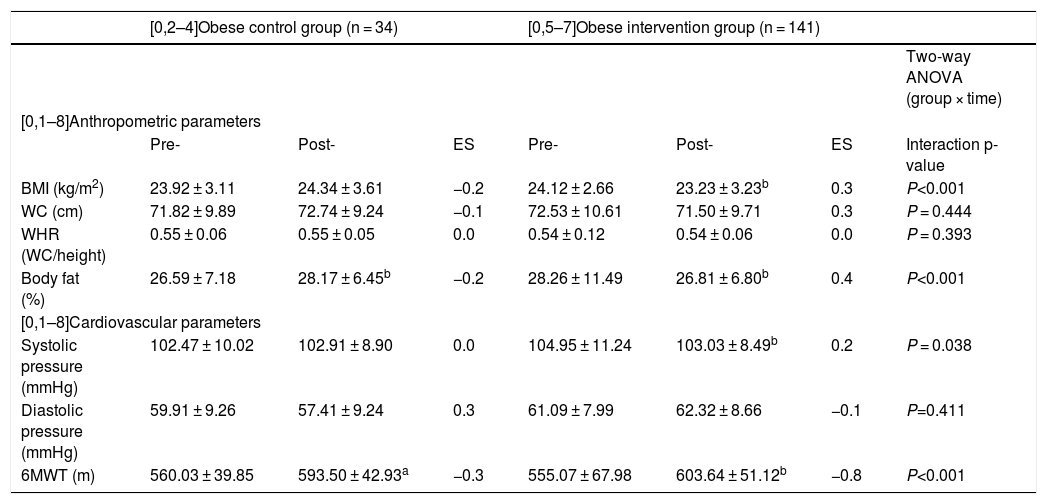
Table 3 compares the obese control and intervention groups (OCG versus OIG). There were no baseline differences in age, BMI, WC, WHR, BF, CRF, SBP or DBP (p > 0.05). However, two-way ANOVA revealed significant differences in the variables BMI (p < 0.001), BF (p < 0.001), SBP (p = 0.038) and the 6MWT (p < 0.001) on comparing the control and intervention groups (pre- versus post-intervention). The OIG showed a significant decrease in BMI (pre- = 24.12 ± 2.66 kg/m2 vs. post- = 23,23 ± 3.23 kg/m2, p < 0.001, ES = 0.3) and BF (pre- = 30.26 ± 11.49 % vs. post- = 26.81 ± 6.80 %, p < 0.001, ES = 0.4). The same group also showed a decrease in SBP (pre- = 104.95 ± 8.49 mmHg vs. post- = 103.03 ± 11.24 mmHg, p = 0.038, ES = 0.2), and CRF improved significantly (6MWT pre- = 555.07 ± 67.98 m vs. post- = 603.64 ± 51.12 m, p < 0.001, ES = −0.8).
Anthropometric and cardiovascular parameters before (pre-) and after (post-) the HIIT program in children with obesity.
| [0,2–4]Obese control group (n = 34) | [0,5–7]Obese intervention group (n = 141) | ||||||
|---|---|---|---|---|---|---|---|
| Two-way ANOVA (group × time) | |||||||
| [0,1–8]Anthropometric parameters | |||||||
| Pre- | Post- | ES | Pre- | Post- | ES | Interaction p-value | |
| BMI (kg/m2) | 23.92 ± 3.11 | 24.34 ± 3.61 | −0.2 | 24.12 ± 2.66 | 23.23 ± 3.23b | 0.3 | P<0.001 |
| WC (cm) | 71.82 ± 9.89 | 72.74 ± 9.24 | −0.1 | 72.53 ± 10.61 | 71.50 ± 9.71 | 0.3 | P = 0.444 |
| WHR (WC/height) | 0.55 ± 0.06 | 0.55 ± 0.05 | 0.0 | 0.54 ± 0.12 | 0.54 ± 0.06 | 0.0 | P = 0.393 |
| Body fat (%) | 26.59 ± 7.18 | 28.17 ± 6.45b | −0.2 | 28.26 ± 11.49 | 26.81 ± 6.80b | 0.4 | P<0.001 |
| [0,1–8]Cardiovascular parameters | |||||||
| Systolic pressure (mmHg) | 102.47 ± 10.02 | 102.91 ± 8.90 | 0.0 | 104.95 ± 11.24 | 103.03 ± 8.49b | 0.2 | P = 0.038 |
| Diastolic pressure (mmHg) | 59.91 ± 9.26 | 57.41 ± 9.24 | 0.3 | 61.09 ± 7.99 | 62.32 ± 8.66 | −0.1 | P=0.411 |
| 6MWT (m) | 560.03 ± 39.85 | 593.50 ± 42.93a | −0.3 | 555.07 ± 67.98 | 603.64 ± 51.12b | −0.8 | P<0.001 |
Data shown represent the mean ± SD. P-values < 0.05 were considered statistically significant.
6MWT: six-minute walk test; WC: waist circumference; HIIT: high-intensity interval training; BMI: body mass index; WHR: waist-height ratio; ES: effect size.
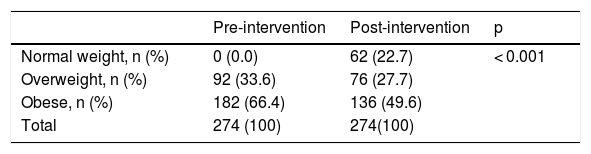
Table 4 shows the pre- and post-intervention changes. A significant decrease was seen in the proportion of schoolchildren with obesity (pre- = 66.4 % vs. post- = 49.6 %), and the number of schoolchildren with normal weight increased (pre- = 0 % vs. post- = 22.7 %) (p < 0.001).
Pre- and post-intervention proportion of schoolchildren in the normal weight, overweight and obese categories.
| Pre-intervention | Post-intervention | p | |
|---|---|---|---|
| Normal weight, n (%) | 0 (0.0) | 62 (22.7) | < 0.001 |
| Overweight, n (%) | 92 (33.6) | 76 (27.7) | |
| Obese, n (%) | 182 (66.4) | 136 (49.6) | |
| Total | 274 (100) | 274(100) |
Values are n (proportions).
The purpose of this study was to determine the effects of HIIT on different anthropometric and cardiovascular parameters in overweight and obese children between 7–9 years of age. The main findings are: 1) in the OWIG, the intervention resulted in significant improvements in BMI, BF and 6MWT; 2) in the OIG, improvements were recorded in BMI, BF, SBP and 6MWT; and 3) the proportion of schoolchildren with obesity decreased after the intervention.
In our study, the intervention had a positive effect in terms of the reduction of BMI in both experimental groups (OWIG, OIG) in the between-group comparison. A study of overweight schoolchildren enrolled in a 6-month HIIT program involving 60 min sessions twice a week reported reductions in BMI, though statistical significance was not reached.25 In contrast, a 12-week HIIT program involving 40 min sessions twice a week resulted in no significant changes in BMI in schoolchildren.26 Therefore, in order for relevant changes in weight status to be obtained using HIIT protocols, longer interventions over time may be needed to observe changes similar to those recorded in our study.
After the 28-week intervention, percentage BF decreased significantly in both intervention groups (OWIG, OIG). These results are similar to those reported in a another study where HIIT was applied twice a week during 6 months.25 A study in overweight children reported a decrease in the sum of skin fold scores, resulting from an exercise protocol comprising 12 cseries of 15 s with an intensity of 120 % of maximal aerobic speed (MAS) and a passive recovery interval of 15 s.27 Similarly, 12 weeks of exercise with two sessions a week was seen to reduce BF in adolescents participating in HIIT.28 A 12-week HIIT program in obese children, with work sessions at an intensity between 85–95 % of maximum heart rate, followed by 3 min of active recovery, did not significantly modify the visceral or subcutaneous adipose tissue.11 The dissimilar results described above in relation to BF could be explained by the variety of HIIT protocols in terms of intensity, volume and duration of the program. Furthermore, a systematic review concluded that the effects of HIIT in preadolescents have not been clearly established to date.29
Cardiorespiratory fitness improved in both intervention groups; however, SBP only decreased significantly in the OIG. On the other hand, it is necessary to take into account that the schoolchildren had a healthy CRF score before the intervention.17 A three-month exercise protocol with work sessions at 90 % of maximum heart rate resulted in significant increments in maximum oxygen consumption (VO2max).30 A high-intensity play program reported improvements in children with normal weight and obesity in terms of VO2max and maximum running speed.31 A 7-month program applied during the PE class improved performance in the 6MWT, and moreover reduced the number of hypertensive students.32 In a 6-month intervention comprising HIIT and low-intensity aerobic training, the participants in both study groups showed a significant decrease in DBP and SBP (p < 0.05); however, heart rate and heart variability showed beneficial changes only in the HIIT group (p < 0.05).33 A high-intensity exercise protocol with a duration of 13 weeks, applied in obese adolescents, yielded significant improvements in terms of systolic and diastolic heart function.34 High-intensity interval training protocols with a duration of 4–12 weeks produce important changes in SBP and increments in VO2max; HIIT therefore may be regarded as a time-efficient intervention strategy in obese young people.35
Limitations and strengths of the studyThis study has some limitations. Firstly, the same methodology was applied to all schoolchildren, and in this regard it may have been more interesting to compare HIIT with other training methods such as aerobic training. Secondly, objective measures of intensity were not considered; only a subjective rating scale was used. The main strength of the study was the large number of schoolchildren enrolled and the duration of intervention; this allows projection of the method to the school system, as a valid alternative for combating the pandemic of childhood obesity.
ConclusionsThe present study shows that long-term HIIT significantly decreases the number of schoolchildren with obesity, and increases the proportion of schoolchildren with normal body weight. Likewise, the intervention was efficient in improving CRF and in reducing percentage BF in children with overweight and obesity. The results therefore suggest that the HIIT protocol used in our study reduces cardiometabolic risk as compared to the control group, which tended to increase or maintain its anthropometric parameters.
Financial supportThe present study was funded by the Universidad de La Frontera, Project DI11-0038, Temuco (Chile).
Conflicts of interestThe authors declare that they have no conflicts of interest.
The research team is grateful to the intervention plan in motricity as a learning and nutritional status enhancer of the Municipal Department of Education of Temuco (Chile).
Please cite this article as: Espinoza-Silva M, Latorre-Román P, Párraga-Montilla J, Caamaño-Navarrete F, Jerez-Mayorga D, Delgado-Floody P. Respuesta en escolares con obesidad al ejercicio intervalado de alta intensidad aplicado en el contexto escolar. Endocrinol Diabetes Nutr. 2019;66:611–619.