Imprecision in terms used in the field of clinical nutrition may lead to misinterpretations among professionals.
ObjectiveFor this reason, the Spanish Society of Endocrinology and Nutrition (SEEN) promoted this document on the terms and definitions used in clinical artificial nutrition (enteral and parenteral), establishing an agreement between Spanish experts of this specialty.
MethodsForty-seven specialists in endocrinology and nutrition, members of the Nutrition Area of the SEEN, participated between April and September 2016. After a systematic literature review, 52 concepts were proposed. The coordinators included two additional concepts, and 57 were finally selected by the working group: 13 of a general nature, 30 referring to enteral nutrition and 14 to parenteral nutrition. The degree of agreement was subsequently determined using a two-round Delphi process. It was finally ratified by consistency and concordance analysis.
ResultsFifty-four of the 57 terms had a very consistent agreement and were concordant. Only three showed no concordance, of whom two were very consistent and one inconsistent. In conclusion, there was consensus in the definition of 54 basic terms in the practice of clinical nutrition.
La imprecisión en la terminología dentro de la nutrición clínica puede acarrear malas interpretaciones entre los distintos profesionales.
ObjetivoPor esta razón, la Sociedad Española de Endocrinología y Nutrición (SEEN) ha promovido la realización del presente trabajo, el primero sobre terminología y definiciones en nutrición artificial clínica (enteral y parenteral) publicado en castellano.
MétodosUn total de 47 especialistas en Endocrinología y Nutrición expertos en la materia, miembros del Área de Nutrición de la SEEN, han participado entre los meses de abril y septiembre de 2016. Tras una revisión bibliográfica sistematizada fueron propuestos 52 conceptos, ampliándose a 54 por las coordinadoras y finalmente a 57 por el grupo de trabajo: 13 de carácter general, 30 referidos a la nutrición enteral y 14 a la parenteral. En una fase posterior se determinó el grado de acuerdo mediante un proceso Delphi de 2 circulaciones. Finalmente fue ratificado mediante un análisis de consistencia y concordancia.
ResultadosEn 54 de los 57 términos hubo un acuerdo muy consistente y resultaban concordantes. Solo 3 no presentaron concordancia, de los que 2 eran muy consistentes y uno inconsistente. En conclusión, queda consensuada la definición de 54 términos básicos en la práctica de la nutrición clínica.
Artificial nutrition is a relatively modern discipline undergoing continuous development. From its origins, this has been a multidisciplinary field involving professionals from different healthcare settings. Daily practice in clinical nutrition in Spain makes use of a broad range of terms and concepts with different definitions. Their use is not homogeneous, however: depending on personal preferences, the professionals involved, or the geographical setting, a given term can have different meanings or connotations. Some of the concepts and terms, of direct Anglo-Saxon origin, can be used in different situations, giving rise to possible misunderstandings or even contradictions.
Terminological imprecision can pose serious problems in clinical practice; it therefore makes sense for attempts to be made to establish common criteria. However, as a prior step to the generation of clinical practice guides, diagnostic or treatment protocols, or documentation for communication with public health authorities, it is essential that a precise and unified definition of the terms most commonly used by the various professionals dedicated to clinical nutrition be established.
For this reason, the Spanish Society of Endocrinology and Nutrition (Sociedad Española de Endocrinología y Nutrición [SEEN]) has promoted the present study with the purpose of precisely defining the most common basic terms and concepts which refer to artificial nutrition (enteral and parenteral).
Material and methodsThe project was implemented between the months of April and September 2016, within the setting of the activity carried out by the Nutrition Area of the SEEN. The SEEN invited all the members of the nutrition working area to participate via e-mail. A total of 46 members were inscribed (Annex), in addition to the coordinators.
The first phase involved a combined systematic literature search in PubMed, Google Scholar, the websites of the SEEN, the Spanish Society of Enteral and Parenteral Nutrition (Sociedad Española de Nutrición Enteral y Parenteral [SENPE]), the European Society of Clinical Nutrition and Metabolism (ESPEN), and the American Society of Parenteral and Enteral Nutrition (ASPEN), as well as the clinical practice guides published by each of these medical bodies. A total of 1682 references were obtained. Reading of the abstracts identified 195 publications referring to terminology, concepts, definitions and classification in enteral and parenteral nutrition. Following the review of these 195 publications, we proposed the inclusion of 54 terms, classified into three sections: 11 corresponded to general aspects, 29 to enteral nutrition, and 14 to parenteral nutrition.
The second phase involved circulating the pre-selected terms among those inscribed, for due review. Even though the initiative was of a voluntary character, the responses of 71.7% of the participants were recorded. A total of 41 terms (75.9% of those proposed) were accepted without change, while 13 were modified (24%) and three new terms were incorporated. Thus, a total of 57 terms finally entered into discussion (Tables 1–3).1–24
Degree of agreement, consistency and concordance of the selected clinical nutrition concepts: general aspects.
| Term | Concept | m | SD | M | IQR | CV | Degree of consistency | Concordance |
|---|---|---|---|---|---|---|---|---|
| Nutritional support | The supply of nutrients required to cover the needs (basal and/or derived from the patient disease condition) via the oral, enteral or parenteral route, with the purpose of improving or maintaining nutritional status. | 9 | 0.28 | 9 | 0 | 0.03 | Very consistenta | Yes |
| Nutritional requirements | The series of reference values regarding the intake of energy and nutrients considered optimum in order to maintain correct nutritional status, prevent the appearance of disease, and (in children) secure normal development and growth rate. | 9 | 0.31 | 9 | 0 | 0.04 | Very consistenta | Yes |
| Standard nutritional formula | A nutritional preparation containing the macro- and micronutrients capable of covering the requirements of most of the population without specific metabolic or digestive disorders, according to age and physical activity. | 9 | 0.48 | 9 | 0 | 0.05 | Very consistenta | Yes |
| Special or specific nutritional formula | A product containing macro- and/or micronutrients adapted to the needs of a patient with a certain disease and/or metabolic or digestive disorder. | 9 | 0.28 | 9 | 0 | 0.03 | Very consistenta | Yes |
| Complete nutritional formula | A formula capable of covering 100% of the macro- and micronutrient requirements. | 9 | 0.25 | 9 | 0 | 0.03 | Very consistenta | Yes |
| Incomplete nutritional formula or nutritional supplement | An incomplete mixture of macro- and micronutrients that serves to reinforce or modify the composition of a diet. | 8 | 1.28 | 8 | 1 | 0.16 | Very consistent | No |
| Continuous nutrition | Administration of nutrition (enteral or parenteral) made as a continuous infusion using a pump or under gravity, and usually for 24 hours. | 9 | 0.28 | 9 | 0 | 0.03 | Very consistenta | Yes |
| Cyclic nutrition | Continuous infusion for periods of under 24 hours (normally 8–16h, allowing rest intervals at night or during the day). | 9 | 0.40 | 9 | 0 | 0.04 | Very consistenta | Yes |
| Intermittent nutrition | Nutrition infusion at regular intervals for short periods of time. | 9 | 0.52 | 9 | 0 | 0.06 | Very consistenta | Yes |
| Organ-specific nutrition, system-specific nutrition or disease-specific nutrition | The use of nutrient formulas containing specific nutrients with the purpose of not only nurturing but also intervening in the therapeutic management of the background disease. | 9 | 0.42 | 9 | 0 | 0.05 | Very consistenta | Yes |
| Specialized nutritional support (SNS) | The administration of nutrients via the oral, enteral or parenteral route, with therapeutic intent. This includes, but is not limited to, enteral or parenteral nutrition to maintain and/or restore optimum nutritional status and health. | 9 | 0.56 | 9 | 1 | 0.06 | Very consistenta | Yes |
| Soluble or fermentable fiber | Substances of plant origin, carbohydrates or their derivatives, that are resistant to hydrolysis by human enzymes and reach the intestine intact, where some may be hydrolyzed and fermented by the flora. Fiber retains water and acquires a gel form during digestion, thereby slowing digestion and the absorption of nutrients. It is composed of pectin, mucilages and gums. | 9 | 0.61 | 9 | 0 | 0.07 | Very consistenta | Yes |
| Insoluble or non-fermentable fiber | Substances of plant origin, carbohydrates or their derivatives, that are resistant to hydrolysis by human enzymes and reach the intestine intact. This type of fiber undergoes little fermentation and is insoluble, though it absorbs water, accelerating food transit and adding volume to stools. It is composed of cellulose, hemicellulose, non-digestible starch and lignin. | 9 | 0.52 | 9 | 0 | 0.06 | Very consistenta | Yes |
CV: coefficient of variation; SD: standard deviation; m: mean; M: median; IQR: interquartile range.
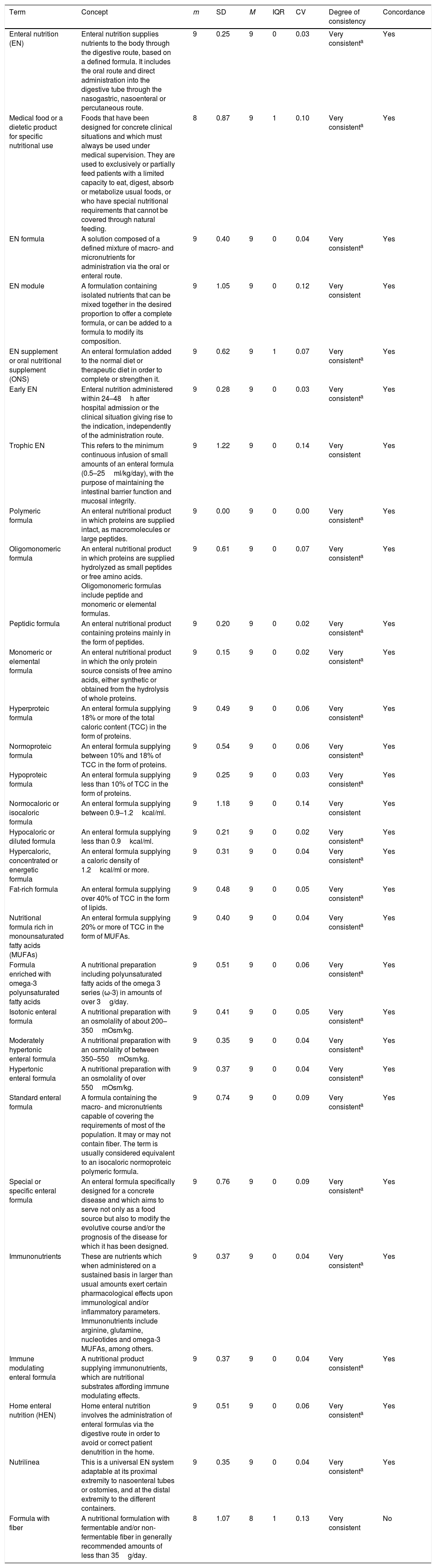
Degree of agreement, consistency and concordance of the selected enteral nutrition concepts.
| Term | Concept | m | SD | M | IQR | CV | Degree of consistency | Concordance |
|---|---|---|---|---|---|---|---|---|
| Enteral nutrition (EN) | Enteral nutrition supplies nutrients to the body through the digestive route, based on a defined formula. It includes the oral route and direct administration into the digestive tube through the nasogastric, nasoenteral or percutaneous route. | 9 | 0.25 | 9 | 0 | 0.03 | Very consistenta | Yes |
| Medical food or a dietetic product for specific nutritional use | Foods that have been designed for concrete clinical situations and which must always be used under medical supervision. They are used to exclusively or partially feed patients with a limited capacity to eat, digest, absorb or metabolize usual foods, or who have special nutritional requirements that cannot be covered through natural feeding. | 8 | 0.87 | 9 | 1 | 0.10 | Very consistenta | Yes |
| EN formula | A solution composed of a defined mixture of macro- and micronutrients for administration via the oral or enteral route. | 9 | 0.40 | 9 | 0 | 0.04 | Very consistenta | Yes |
| EN module | A formulation containing isolated nutrients that can be mixed together in the desired proportion to offer a complete formula, or can be added to a formula to modify its composition. | 9 | 1.05 | 9 | 0 | 0.12 | Very consistent | Yes |
| EN supplement or oral nutritional supplement (ONS) | An enteral formulation added to the normal diet or therapeutic diet in order to complete or strengthen it. | 9 | 0.62 | 9 | 1 | 0.07 | Very consistenta | Yes |
| Early EN | Enteral nutrition administered within 24–48h after hospital admission or the clinical situation giving rise to the indication, independently of the administration route. | 9 | 0.28 | 9 | 0 | 0.03 | Very consistenta | Yes |
| Trophic EN | This refers to the minimum continuous infusion of small amounts of an enteral formula (0.5–25ml/kg/day), with the purpose of maintaining the intestinal barrier function and mucosal integrity. | 9 | 1.22 | 9 | 0 | 0.14 | Very consistent | Yes |
| Polymeric formula | An enteral nutritional product in which proteins are supplied intact, as macromolecules or large peptides. | 9 | 0.00 | 9 | 0 | 0.00 | Very consistenta | Yes |
| Oligomonomeric formula | An enteral nutritional product in which proteins are supplied hydrolyzed as small peptides or free amino acids. Oligomonomeric formulas include peptide and monomeric or elemental formulas. | 9 | 0.61 | 9 | 0 | 0.07 | Very consistenta | Yes |
| Peptidic formula | An enteral nutritional product containing proteins mainly in the form of peptides. | 9 | 0.20 | 9 | 0 | 0.02 | Very consistenta | Yes |
| Monomeric or elemental formula | An enteral nutritional product in which the only protein source consists of free amino acids, either synthetic or obtained from the hydrolysis of whole proteins. | 9 | 0.15 | 9 | 0 | 0.02 | Very consistenta | Yes |
| Hyperproteic formula | An enteral formula supplying 18% or more of the total caloric content (TCC) in the form of proteins. | 9 | 0.49 | 9 | 0 | 0.06 | Very consistenta | Yes |
| Normoproteic formula | An enteral formula supplying between 10% and 18% of TCC in the form of proteins. | 9 | 0.54 | 9 | 0 | 0.06 | Very consistenta | Yes |
| Hypoproteic formula | An enteral formula supplying less than 10% of TCC in the form of proteins. | 9 | 0.25 | 9 | 0 | 0.03 | Very consistenta | Yes |
| Normocaloric or isocaloric formula | An enteral formula supplying between 0.9–1.2kcal/ml. | 9 | 1.18 | 9 | 0 | 0.14 | Very consistent | Yes |
| Hypocaloric or diluted formula | An enteral formula supplying less than 0.9kcal/ml. | 9 | 0.21 | 9 | 0 | 0.02 | Very consistenta | Yes |
| Hypercaloric, concentrated or energetic formula | An enteral formula supplying a caloric density of 1.2kcal/ml or more. | 9 | 0.31 | 9 | 0 | 0.04 | Very consistenta | Yes |
| Fat-rich formula | An enteral formula supplying over 40% of TCC in the form of lipids. | 9 | 0.48 | 9 | 0 | 0.05 | Very consistenta | Yes |
| Nutritional formula rich in monounsaturated fatty acids (MUFAs) | An enteral formula supplying 20% or more of TCC in the form of MUFAs. | 9 | 0.40 | 9 | 0 | 0.04 | Very consistenta | Yes |
| Formula enriched with omega-3 polyunsaturated fatty acids | A nutritional preparation including polyunsaturated fatty acids of the omega 3 series (ω-3) in amounts of over 3g/day. | 9 | 0.51 | 9 | 0 | 0.06 | Very consistenta | Yes |
| Isotonic enteral formula | A nutritional preparation with an osmolality of about 200–350mOsm/kg. | 9 | 0.41 | 9 | 0 | 0.05 | Very consistenta | Yes |
| Moderately hypertonic enteral formula | A nutritional preparation with an osmolality of between 350–550mOsm/kg. | 9 | 0.35 | 9 | 0 | 0.04 | Very consistenta | Yes |
| Hypertonic enteral formula | A nutritional preparation with an osmolality of over 550mOsm/kg. | 9 | 0.37 | 9 | 0 | 0.04 | Very consistenta | Yes |
| Standard enteral formula | A formula containing the macro- and micronutrients capable of covering the requirements of most of the population. It may or may not contain fiber. The term is usually considered equivalent to an isocaloric normoproteic polymeric formula. | 9 | 0.74 | 9 | 0 | 0.09 | Very consistenta | Yes |
| Special or specific enteral formula | An enteral formula specifically designed for a concrete disease and which aims to serve not only as a food source but also to modify the evolutive course and/or the prognosis of the disease for which it has been designed. | 9 | 0.76 | 9 | 0 | 0.09 | Very consistenta | Yes |
| Immunonutrients | These are nutrients which when administered on a sustained basis in larger than usual amounts exert certain pharmacological effects upon immunological and/or inflammatory parameters. Immunonutrients include arginine, glutamine, nucleotides and omega-3 MUFAs, among others. | 9 | 0.37 | 9 | 0 | 0.04 | Very consistenta | Yes |
| Immune modulating enteral formula | A nutritional product supplying immunonutrients, which are nutritional substrates affording immune modulating effects. | 9 | 0.37 | 9 | 0 | 0.04 | Very consistenta | Yes |
| Home enteral nutrition (HEN) | Home enteral nutrition involves the administration of enteral formulas via the digestive route in order to avoid or correct patient denutrition in the home. | 9 | 0.51 | 9 | 0 | 0.06 | Very consistenta | Yes |
| Nutrilinea | This is a universal EN system adaptable at its proximal extremity to nasoenteral tubes or ostomies, and at the distal extremity to the different containers. | 9 | 0.35 | 9 | 0 | 0.04 | Very consistenta | Yes |
| Formula with fiber | A nutritional formulation with fermentable and/or non-fermentable fiber in generally recommended amounts of less than 35g/day. | 8 | 1.07 | 8 | 1 | 0.13 | Very consistent | No |
CV: coefficient of variation; SD: standard deviation; m: mean; M: median; MUFAs: monounsaturated fatty acids; EN: enteral nutrition; HEN: home enteral nutrition; IQR: interquartile range; ONS: oral nutritional supplement; TCC: total caloric content.
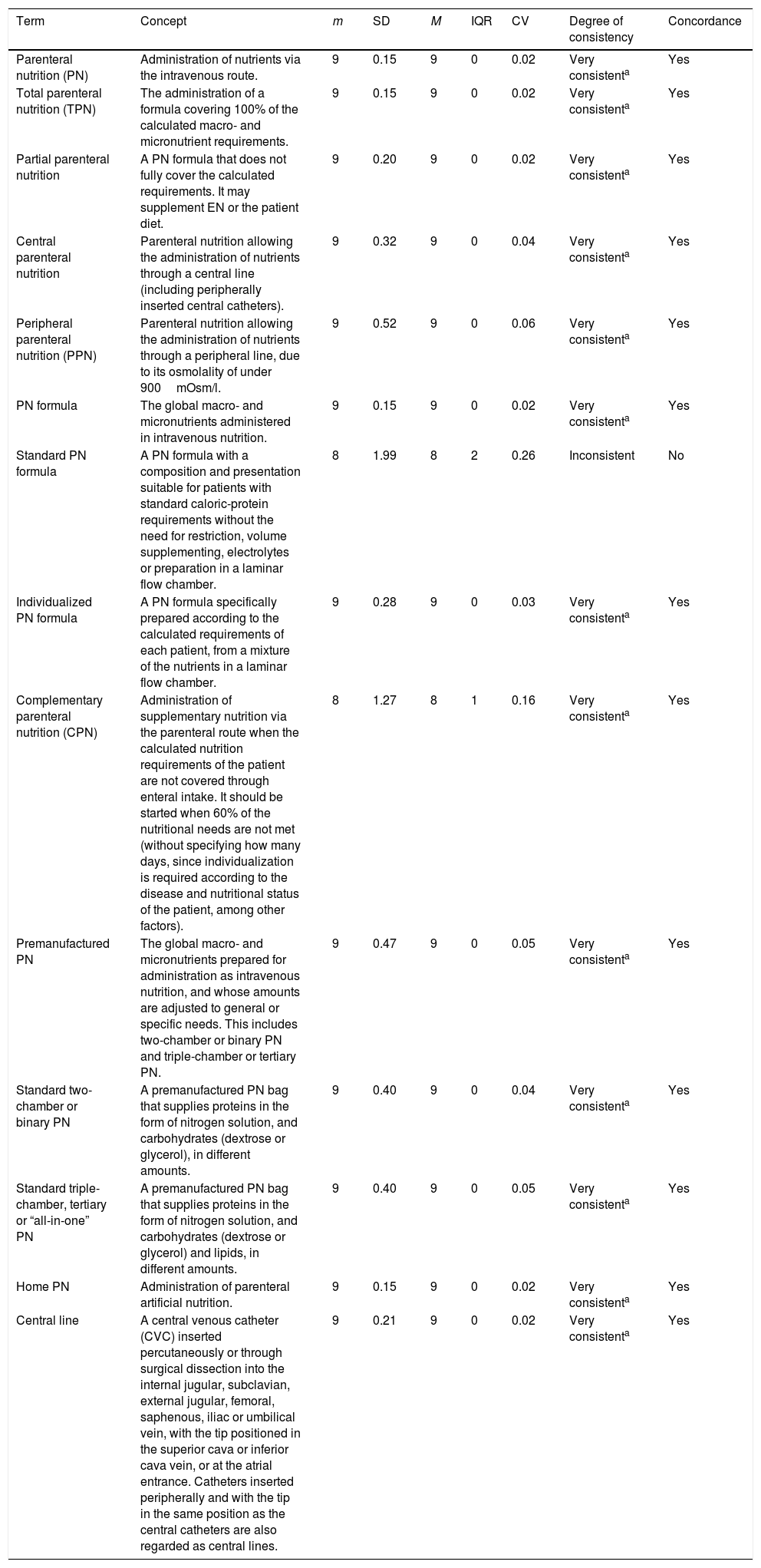
Degree of agreement, consistency and concordance of the selected parenteral nutrition concepts.
| Term | Concept | m | SD | M | IQR | CV | Degree of consistency | Concordance |
|---|---|---|---|---|---|---|---|---|
| Parenteral nutrition (PN) | Administration of nutrients via the intravenous route. | 9 | 0.15 | 9 | 0 | 0.02 | Very consistenta | Yes |
| Total parenteral nutrition (TPN) | The administration of a formula covering 100% of the calculated macro- and micronutrient requirements. | 9 | 0.15 | 9 | 0 | 0.02 | Very consistenta | Yes |
| Partial parenteral nutrition | A PN formula that does not fully cover the calculated requirements. It may supplement EN or the patient diet. | 9 | 0.20 | 9 | 0 | 0.02 | Very consistenta | Yes |
| Central parenteral nutrition | Parenteral nutrition allowing the administration of nutrients through a central line (including peripherally inserted central catheters). | 9 | 0.32 | 9 | 0 | 0.04 | Very consistenta | Yes |
| Peripheral parenteral nutrition (PPN) | Parenteral nutrition allowing the administration of nutrients through a peripheral line, due to its osmolality of under 900mOsm/l. | 9 | 0.52 | 9 | 0 | 0.06 | Very consistenta | Yes |
| PN formula | The global macro- and micronutrients administered in intravenous nutrition. | 9 | 0.15 | 9 | 0 | 0.02 | Very consistenta | Yes |
| Standard PN formula | A PN formula with a composition and presentation suitable for patients with standard caloric-protein requirements without the need for restriction, volume supplementing, electrolytes or preparation in a laminar flow chamber. | 8 | 1.99 | 8 | 2 | 0.26 | Inconsistent | No |
| Individualized PN formula | A PN formula specifically prepared according to the calculated requirements of each patient, from a mixture of the nutrients in a laminar flow chamber. | 9 | 0.28 | 9 | 0 | 0.03 | Very consistenta | Yes |
| Complementary parenteral nutrition (CPN) | Administration of supplementary nutrition via the parenteral route when the calculated nutrition requirements of the patient are not covered through enteral intake. It should be started when 60% of the nutritional needs are not met (without specifying how many days, since individualization is required according to the disease and nutritional status of the patient, among other factors). | 8 | 1.27 | 8 | 1 | 0.16 | Very consistenta | Yes |
| Premanufactured PN | The global macro- and micronutrients prepared for administration as intravenous nutrition, and whose amounts are adjusted to general or specific needs. This includes two-chamber or binary PN and triple-chamber or tertiary PN. | 9 | 0.47 | 9 | 0 | 0.05 | Very consistenta | Yes |
| Standard two-chamber or binary PN | A premanufactured PN bag that supplies proteins in the form of nitrogen solution, and carbohydrates (dextrose or glycerol), in different amounts. | 9 | 0.40 | 9 | 0 | 0.04 | Very consistenta | Yes |
| Standard triple-chamber, tertiary or “all-in-one” PN | A premanufactured PN bag that supplies proteins in the form of nitrogen solution, and carbohydrates (dextrose or glycerol) and lipids, in different amounts. | 9 | 0.40 | 9 | 0 | 0.05 | Very consistenta | Yes |
| Home PN | Administration of parenteral artificial nutrition. | 9 | 0.15 | 9 | 0 | 0.02 | Very consistenta | Yes |
| Central line | A central venous catheter (CVC) inserted percutaneously or through surgical dissection into the internal jugular, subclavian, external jugular, femoral, saphenous, iliac or umbilical vein, with the tip positioned in the superior cava or inferior cava vein, or at the atrial entrance. Catheters inserted peripherally and with the tip in the same position as the central catheters are also regarded as central lines. | 9 | 0.21 | 9 | 0 | 0.02 | Very consistenta | Yes |
CV: coefficient of variation; CVC: central venous catheter; SD: standard deviation; m: mean; M: median; EN: enteral nutrition; PN: parenteral nutrition; CPN: complementary parenteral nutrition; PPN: peripheral parenteral nutrition; TPN: total parenteral nutrition; IQR: interquartile range.
The third phase of the study involved a two-round Delphi process to determine the degree of concordance with the proposed definitions. For this purpose a specific e-mail was generated, with the questionnaire being submitted via personal mail to the 48 inscribed members. In this first round the members were required to score their degree of agreement by means of a Likert scale from 1 to 9, where 1 represents minimum concordance with the term definition and 9 represents maximum concordance.
Those who answered the first questionnaire received the second round, including the median and interquartile range as an orientation to pre-agreement.
Data analysis was performed using the statistical tools of Microsoft Excel 2012, with calculation of the following values for the 57 terms: mean (m) and standard deviation (SD); median (M) and interquartile range (IQR), as well as the coefficient of variation (CV).
Concordance consistency was determined based on two criteria:
- 1.
Criterion according to group median if IQR≤1.00:
- a)
1–2 and 8–9: disagreement and agreement, respectively, “very consistent”.
- b)
3 and 7: disagreement and agreement, respectively, “consistent”.
- c)
4–6: “inconsistent”.
- 2.
Criterion according to simultaneous compliance: mean and median ≤3 or ≥7, in addition to SD and IQR ≤1 and CV ≤0.25, defining “very consistent”.
In the event of IQR>1, dispersion was considered excessive and therefore proved “inconsistent”.
Concordance was assumed when at least 95% of the responses were concentrated in the same sector: 1–3: disagreement; 4–6 undefined; 7–9: agreement.
In parallel to the process, we determined the global Spearman correlation level and its p-value (cut-off point p=0.05) to check whether the two rounds were congruent, and the Cronbach alpha (cut-off point 0.7) to establish the internal reliability of the questionnaire.
ResultsOf the 48 initially inscribed specialists in Endocrinology and Nutrition, 47 completed both Delphi rounds (Annex). Their ages ranged between 30 and 60 years, with a mean of 42.7 years (SD: 8.67), and a professional experience of between 7 and 37 years. The specialists came from 38 hospital centers in all the Spanish Autonomous Communities, in both the public (89.5%) and private sectors.
The degree of concordance and consistency are reported in Tables 1–3. The 13 nutrition terms of a general character (Table 1) showed a consistent or very consistent level of agreement, though in one case concordance was lacking.
Of the 30 terms related to enteral nutrition (Table 2), only one showed a lack of concordance. Agreement was observed in the other cases.
Of the 14 terms related to parenteral nutrition (Table 3), we identified an inconsistent level of agreement that likewise was not concordant.
At the global level, the Spearman correlation coefficient was 0.3627, with p=0.0055, and a Cronbach alpha of 0.9026.
DiscussionOver the last few years, as a result of the efforts of European and North American societies for nutrition, a number of introductions to clinical practice guides have been published, documenting the definitions of the terms used. To the best of our knowledge, this is the first publication in Spain seeking to establish a consensus regarding the definitions in Spanish of the most important and common terms in clinical nutrition. As can be seen from the tables, the terms included are in very common use. Their choice depended upon the systematic literature search for definitions and concepts, as well as on the publications and websites of the different societies for nutrition. Although not part of the Delphi method, we considered it very important to have a prior consultation with the experts on the suitability of the selected terms. In this way, and in addition to establishing the definition of 13 terms, we were able to incorporate three new terms which referred to fiber.
The Delphi method is considered the best technique for evaluating agreement and/or evidence of discrepancies among experts. The successive submission of questionnaires reduces dispersion and helps define the general consensus. With regard to the consistency of the agreements, dispersion has been limited with respect to the central value, in order to establish unequivocal support of the affirmations. The first criterion was limited to IQR≤1.00, while the second and more demanding criterion contemplated the mean and median, SD, IQR≤1.00 and CV≤0.25.
Likewise, the concordance criterion, which required a response coincidence of at least 95% among the participants, was very demanding.
We observed no relevant deviations with regard to the characteristics of the participating experts. On the basis of the Spearman correlation and p-value, we consider that there was adequate correlation between the two Delphi rounds. Furthermore, the Cronbach alpha confirmed the internal reliability of the questionnaire.
Of the 57 selected terms and definitions, 54 showed very consistent agreement, and thus could be regarded as defined. Only three terms lacked agreement on their definition. The Delphi method does not allow us to determine the reasons for a lack of consensus, though some of the reasons can be intuited from the comments of the participants. From a strict perspective, in defining the term nutritional supplement, enteral nutrition initially included in its description an incomplete mixture of nutrients destined to “supplement” feeding. However, regulation regarding the financing of enteral nutrition formulas in Spain has probably modified this concept. Many professionals use the term with reference to nutritionally complete formulas that are used as a supplement, always flavored and supplied in bottles, jars or in brik format.
With regard to the definition of enteral formula with fiber, we consider that there was only limited agreement regarding the quantity contemplated in the definition. This is one of the terms that was modified by the contributions of the experts, since no upper or lower limit in quantity was initially defined. The debate regarding the amount of fiber which enteral nutrition should supply has persisted for decades, with no drawing of firm conclusions. Not only the most adequate quantity of fiber but also the necessary type of fiber remains to be defined. In both cases the answer is probably dependent upon the clinical indication. On the other hand, it seems logical to assume that the quantity we should include in the definition must refer to the lower limit, since the presence of any amount of fiber whatever should not suffice to define the enteral nutrition formula as a formula with fiber. The definition of a minimum quantity therefore remains pending.
The reason why consensus was not reached regarding the term standard parenteral nutrition is probably related to the condition that it is not prepared in a laminar flow chamber. Perhaps its meaning should be similar to that of a standard enteral nutrition formula, referring to its composition, not its preparation. We should seek a term for those premanufactured parenteral nutrition formulas that do not require major changes in composition because they can be used in patients without nutritional complications or changing needs.
In conclusion, to the best of our knowledge, the present study is the first document to offer a definition in Spanish of the most commonly used terms in clinical artificial nutrition. We believe that it may become a starting document for the reaching of consensus with other scientific bodies involved in nutrition.
Conflicts of interestThe authors state that they have no conflicts of interest.
Thanks are due to the participating members of the Nutrition Working Group of the SEEN (Annex), the SEEN Foundation for funding of the project, and Scientia Salus for technical secretarial support.
| Abad González, A.L. | H. G. U. de Alicante (Valencia); |
| Alfaro Martínez, J.J. | C. H. U. de Albacete (Castilla-La Mancha); |
| Altemir Trallero, J. | H. G. San Jorge (Aragón); |
| Álvarez Hernández, J. | H. U. Príncipe de Asturias (Madrid); |
| Aragón Valera, C. | H. U. Fundación Jiménez Díaz (Madrid); |
| Argente Pla, M. | H. U. i Politècnic La Fe (Valencia); |
| Arraiza Irigoyen, C. | C. H. de Jaén (Andalusia); |
| Ballesteros-Pomar, M.D. | C. A. U. de León (Castilla y León); |
| Batanero Maguregui, R. | H. U. Marqués de Valdecilla (Cantabria); |
| Botella Romero, F. | G. de Atención I. (C. H. de Albacete) (Castilla-La Mancha); |
| Burgos Peláez, R. | H. U. Vall d’Hebron (Catalonia); |
| Cancer Minchot, E. | H. U. de Fuenlabrada (Madrid); |
| de Luis Román, D. | H. C. U. de Valladolid (Castilla y León); |
| de Luna Boquera, I. | H. U. Quirónsalud (Madrid); |
| del Olmo García, D. | H. U. Severo Ochoa (Madrid); |
| Díaz Guardiola, P. | H. U. Infanta Sofía de Madrid (Madrid); |
| García Luna, P.P. | H. Virgen del Rocío (Andalusia); |
| García Malpartida, K. | H. U. i Politècnic La Fe (Valencia); |
| García Puente, I. | H. Perpetuo Socorro (Canary Islands); |
| García Zafra, MV | H. G. U. Santa Lucia de Cartagena (Murcia); |
| García-Manzanares Vázquez de Agredos, A. | H. G. La Mancha Centro (Castilla-La Mancha); |
| Herrero Ruiz, A. | H. C. U. de Salamanca (Castilla y León); |
| Iglesias Hernández, N.C. | H. U. de Basurto (Basque Country); |
| López Gómez, J.J. | H. C. U. de Valladolid (Castilla y León); |
| Luengo Pérez, L.M. | H. U. Infanta Cristina de Badajoz (Extremadura); |
| Martín Palmero, M.A. | H. San Pedro (La Rioja); |
| Martínez Olmos, M.A. | C. H. U. de Santiago de Compostela (Galicia); |
| Molina Puerta, M.J. | H. U. Reina Sofía de Córdoba (Andalusia); |
| Muñoz Jiménez, C. | H. U. Reina Sofía de Córdoba (Andalusia); |
| Ocón Bretón, J. | H. C. U. Lozano Blesa (Aragón); |
| Olivares Alcolea, J. | H. Son Llàtzer (Balearic Islands); |
| Olveira Fuster, G. | H. R. U. de Málaga (Andalusia); |
| Parreño Caparrós, E. | H. de la Vega Lorenzo Guirao (Murcia); |
| Peiró Martínez, I. | I. Catalán de Oncología (Catalonia); |
| Pereyra-García Castro, F. | H. U. Ntra. Señora de la Candelaria (Canary Islands); |
| Petrina Jáuregui, M.E. | C. H. de Navarra (Navarre); |
| Pita Gutiérrez, F. | C. H. U. de A Coruña (Galicia); |
| Pujante Alarcón, P. | H. C. de Asturias (Asturias); |
| Ramos Carrasco, A. | H. U. de Móstoles (Madrid); |
| Sánchez Juan, C. | H. G. U. de Valencia (Valencia); |
| Suárez Llanos, J.P. | H. U. Ntra. Señora de la Candelaria (Canary Islands); |
| Tapia Guerrero, M.J. | H. R. U. de Málaga (Andalusia); |
| Tejera Pérez, C. | C. H. U. del Ferrol (Galicia); |
| Tenorio Jiménez, C. | C. H. de Jaén (Andalusia); |
| Tomé García, M. | H. Internacional Xanit (Andalusia); |
| Vidal Casariego, A.J. | C. A. U. de León (Castilla y León); |
| Zugasti Murillo, A. | C. H. de Navarra (Navarre). |
Please cite this article as: del Olmo García MD, Ocón Bretón J, Álvarez Hernández J, Ballesteros Pomar MD, Botella Romero F, Bretón Lesmes I, et al. Términos, conceptos y definiciones en nutrición clínica artificial. Proyecto ConT-SEEN. Endocrinol Diabetes Nutr. 2018;65:5–16.