“We tend to think in opposites, to feel that what is not good must be bad and that what is not bad must be good”. Samuel I. Hayakawa
Pituitary neuroendocrine tumors are tumors that have no specific molecular characteristics that may be applied in the context of routine clinical diagnosis.1
In pathology, historically (and to date) we have divided tumors into benign and malignant, and although almost five centuries have gone by since G. Falopio established this division, the main task of the pathologist – and the first thing the clinician wants to know – is to establish which of these two categories the tumor belongs to. However, on the basis of our current understanding of the nature of neoplasms, we see that the above benign-malignant paradigm is not so clear-cut. In effect, it is obvious that, either as a result of the sum of genetic events or of the functional changes derived from them, there is a broad range of possibilities which in certain situations make it impossible to trace a clear line separating benign tumors from malignant lesions.
In 2004, the World Health Organization (WHO) introduced a system for grading primary endocrine tumors of the pituitary gland.2 These tumors were classified as typical adenoma, atypical adenoma, and pituitary carcinoma. However, differences between “typical” and “atypical” adenomas were not clearly established, and there are no morphological criteria for distinguishing locally aggressive “atypical” adenomas from carcinomas when the tumor is limited to the sella turcica.3 Although hypercellularity, cytological atypia, high mitotic activity (particularly if atypical mitotic figures are present), necrosis, the invasion of adjacent structures, and recurrence are not necessarily indicators of malignancy in that they can be seen in lesions exhibiting a favorable clinical course, in most cases they are indeed indicative of aggressive behavior. Pituitary carcinomas are only exceptionally diagnosed, partly because of a highly restrictive definition of the WHO and of previous classifications, since the crucial defining criterion is the confirmation of brain-spinal cord spread and/or systemic metastases.
In the new WHO 2017 classification,4 the histological grading of pituitary neuroendocrine tumors is not contemplated, and it is recommended that reference to the intermediate entity called “atypical” adenoma should be abandoned. This, in effect, means a return to the adenoma-carcinoma (benign-malignant) model. However, reference is made to “high risk” adenomas (tumors exhibiting rapid growth, radiographic invasion, and with a high proliferation index [Ki-67]) and to special subtypes whose clinical behavior has been shown to be more aggressive because of their intrinsic histological characteristics, such as sparsely granulated somatotropic adenoma or silent corticotroph adenoma.
I trust that the reader will agree with us when we affirm that in tumors of this kind the most we can say is that those lesions corresponding to one end of the range are likely to exhibit benign behavior (like a green traffic light: “crossing is safe”), while those at the opposite end are likely to exhibit malignant behavior (red light: “danger”). The approach adopted by the new WHO classification thus ignores all the lesions found in between (yellow light: “caution”), and hence the whole spectrum of derived possibilities. The fact is that not everyone is aware of what the “yellow” traffic light means or of what to do in such situations, and few remember that after this “yellow” light the “red” light appears...
In other tumors of endocrine organs, the situation is not very different. We have struggled for decades with differential diagnoses between adenoma and carcinoma of the parathyroid and adrenal glands, simply because of this insistence on defining the tumor as benign or malignant, when in some cases the differences between the two are so subtle that only the occurrence of metastases during patient follow-up can define the true diagnosis. We must recognize that this simplistic division between benign and malignant tumors is inadequate for expressing the existing range of possibilities.
This situation has sometimes led to inconsistent terminologies and a lack of uniformity in tumor taxonomy. In the case of adenoma versus carcinoma, certain tumors that may cause significant morbidity due to hormone hypo- or hypersecretion, the invasion of brain structures, blindness, and cranial nerve palsies that may require radiotherapy and ultimately prove fatal are classified as adenomas (and thus as benign lesions). By contrast, other epithelial tumors such as basal cell carcinoma of the skin are classified as cancer, when in fact these widely invasive lesions (referred to as ulcus rodens in the past because of their locally aggressive behavior) very rarely (if ever) produce metastases.
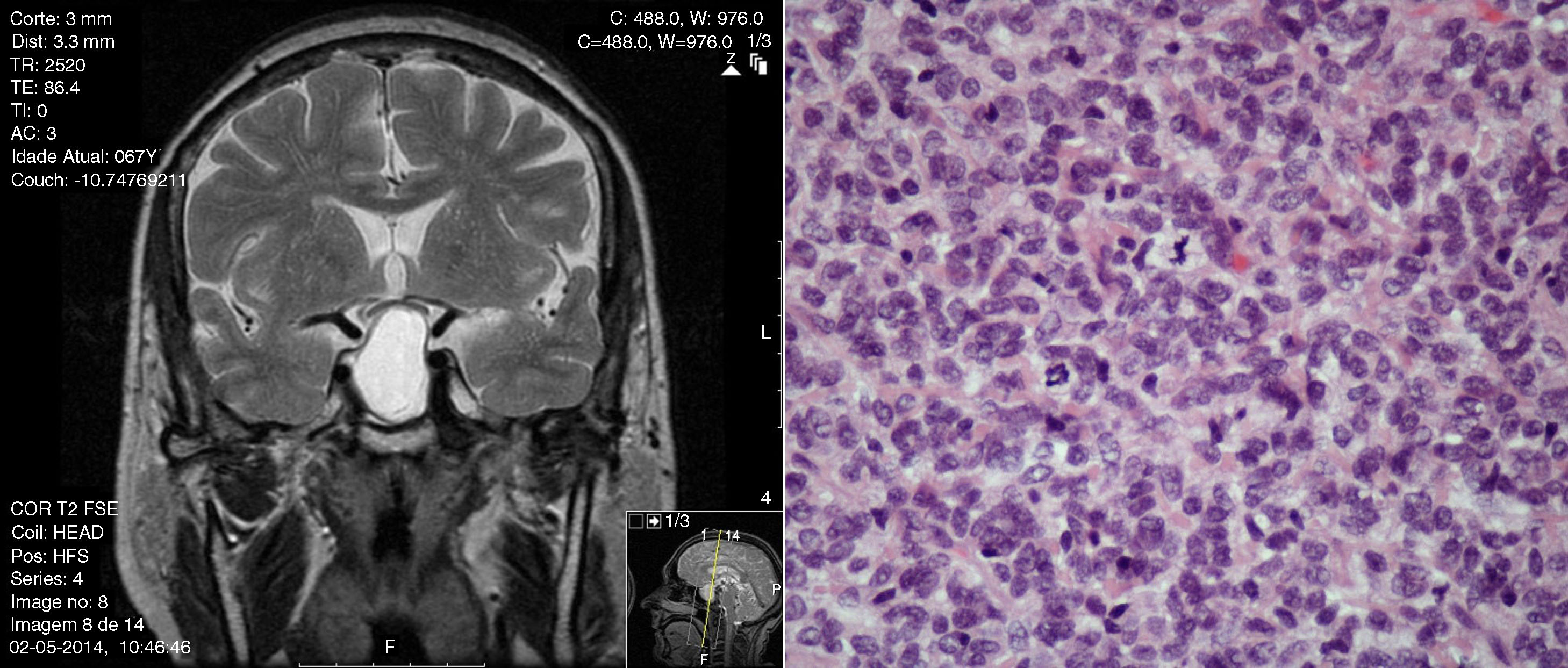
Applying the term adenoma (even if classified as “atypical”) to a pituitary neuroendocrine tumor transmits the idea of an indolent tumor, while using the term carcinoma (even if classified as well differentiated and in situ) transmits the idea of an aggressive and potentially metastatic neoplasm. In the presence of characteristics of aggressiveness with no documented metastases, why not use the term “atypical pituitary neuroendocrine tumor/neoplasm”? (Fig. 1). The 2016 International Pituitary Pathology Club proposed the reclassification of these tumors by applying the terminology that has been widely accepted in other neuroendocrine tumors, thus recommending the use of PitNET (pituitary neuroendocrine tumors),5 a term previously suggested by other authors.6
In conclusion, the dual benign-malignant nomenclature should be discouraged, as has already been suggested by other authorities in this field.7,8 We recommend the adoption of a classification according to the risk-estimating biological behavior of the tumor, instead of stubbornly insisting on dividing all neoplastic proliferations into just these two categories. In fact, in pathology in recent years a number of terms have come into general use which support a belief in the coexistence of intermediate tumor categories (semi-malignant, pseudo-malignant, borderline, intermediate, atypical, of uncertain malignant potential, etc.). Re-evaluation of the definition, classification and criteria of malignancy applicable to neuroendocrine tumors appears necessary, specifically as regards pituitary neoplasms, so we can leave behind the famous phrase “there are no borderline tumors, only borderline pathologists” and adopt a new phrase “there are no borderline pathologists, only borderline classifications”.
Please cite this article as: Tortosa F. El paradigma benigno-maligno en tumores neuroendocrinos hipofisarios y la metáfora del semáforo: reflexiones de un patólogo. Endocrinol Diabetes Nutr. 2019;66:134–135.