Metastases in the thyroid gland are very rare despite its high blood flow.1,2 According to the literature, thyroid metastases account for around 1.4–3% of all patients undergoing surgery for suspected thyroid malignancy.1–3 The cancers that most frequently metastasise to the thyroid are: renal cell carcinoma (48.1%), colorectal cancer (10.4%), lung cancer (8.3%), breast cancer (7.8%), and sarcoma (4%).2,4,5 In autopsy series, the proportion of thyroid micrometastases reported is between 4.4% and 24%,5,6 which shows that they are significantly underdiagnosed.
Furthermore, large series of patients have revealed that syndrome of inappropriate antidiuretic hormone secretion (SIADH) occurs in 3% of patients with head and neck cancer, in 0.7% of those with non-small cell lung cancer and in 15% of those with small cell lung carcinoma.7
This was the case of a 70-year-old woman who visited accident and emergency due to recent onset of a lump on her neck and dysphonia. After an incidental finding of hyponatraemia in the laboratory tests, she was admitted to endocrinology. She did not report any relevant history and was not on any medication. In the directed anamnesis, she also reported a two-week history of dysphagia to solids. Her blood pressure was 164/90mmHg and her heart rate was 72 bpm. Her hydration was normal and she did not exhibit signs of fluid overload. Cardiopulmonary auscultation did not reveal significant findings. A predominantly left goitre with a hard consistency and which was not painful on palpation was found.
Initial blood tests revealed hypoosmolar hyponatraemia with plasma sodium concentration (Na+) 127mmol/l, potassium (K+) 4.9mmol/l, osmotic concentration (Osm) 255mOsm/kg, creatinine 0.63mg/dl, urea 20mg/dl and CKD-EPI 82ml/min. In urine, the concentration of Na+ was 62mmol/l and the osmotic concentration 579 mOsm/kg, findings which are consistent with the diagnosis of SIADH. There was no evidence of hypothalamic-pituitary-adrenal axis dysfunction (serum cortisol 17.8μg/dl).
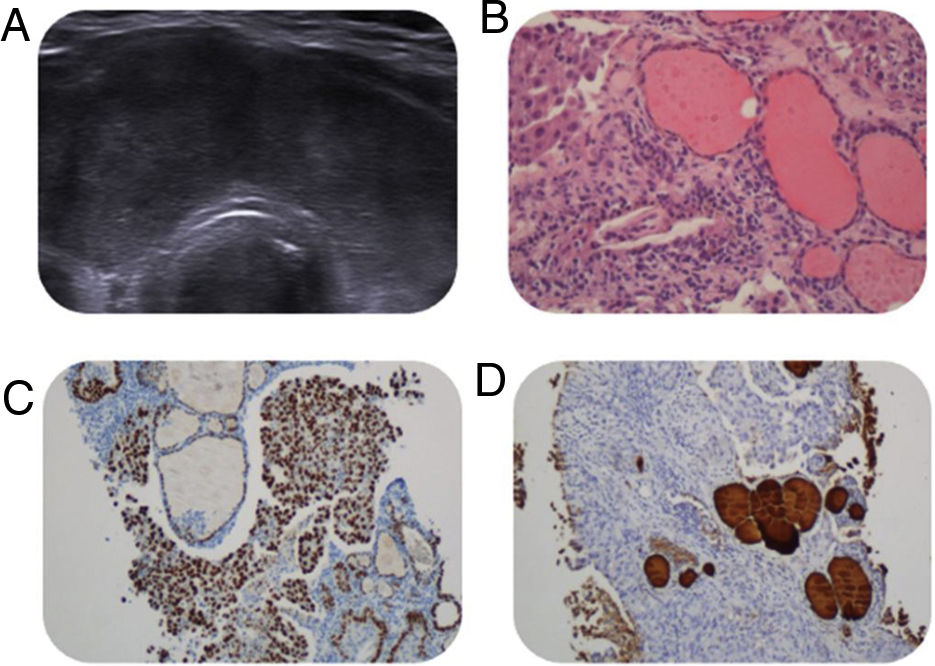
No relevant findings were found on the chest X-ray. The serum concentration of thyroid-stimulating hormone (TSH) and the thyroid autoimmunity study were within normal limits. Neck ultrasound revealed an enlarged thyroid gland with globally altered echostructure, a pseudonodular appearance, significant hypoechogenicity with isoechoic areas and hypervascularisation, as well as some reactive cervical lymph nodes in compartments II–IV (Fig. 1A).
Despite the fact that no thyroid nodule was singled out on the ultrasound, it was decided to perform fine-needle aspiration (FNA) of the thyroid in light of the clinical suspicion of malignancy based on the recent appearance of goitre, hardness on palpation and associated local symptoms, revealing a poorly differentiated carcinoma (Fig. 1B).
The diagnosis of SIADH with no apparent related cause led to requesting a full-body CT scan, performed following the FNA, which revealed an enlarged thyroid gland measuring 3.6×2cm in the RTL and 2.5×2.4cm in the LTL, predominantly hypodense and with decreased uptake, and a pulmonary nodule measuring 2cm in diameter located in segment 6 of the RLL, with a spiculated morphology suggestive of neoplasia, and multiple hilar-mediastinal adenopathies, segmental pulmonary thrombosis and 2.5-cm-thick pericardial effusion.
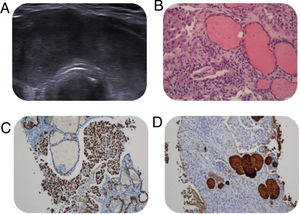
A core needle biopsy (CNB) of the thyroid and a cervical adenopathy were performed, which confirmed that both tissues were infiltrated by a high-grade carcinoma. Immunohistochemistry (IHC) revealed positive tumour cells with cytokeratin (CK) 7, (CK) 20, AE1/AE3 and TTF1 (Fig. 1C), negative for calcitonin, thyroglobulin and p40 (Fig. 1D). PD-L1 was positive for tumour cells in 65%.
The results of the tests described enabled us to reach a diagnosis of stage IV high-grade lung adenocarcinoma (thyroid, pericardium), and treatment with atezolizumab (anti-PD-L1) and tiragolumab (anti-TIGIT) was started.
This was a female patient presenting with thyroid metastasis and paraneoplastic SIADH as the first manifestations of lung adenocarcinoma, both entities being extremely rare in the literature. The remarkable aspect of the case is the atypical clinical presentation, in which the diagnosis was reached due to a thyroid FNA, requested as a result of the high clinical suspicion of thyroid malignancy even following a thyroid ultrasound without the presence of a nodule.
According to a multicentre study conducted in the USA and Europe in which FNA was performed in patients with a malignant condition, the prevalence of thyroid metastases was 1.9%.8 For this reason, it is advisable to consider the potential for thyroid metastasis in patients presenting with a known primary carcinoma that most frequently metastasises to the thyroid. For its diagnosis, it is useful to perform an ultrasound-guided FNA as it is a fast, minimally invasive and inexpensive technique with a high negative predictive value.5,8
Thyroid metastasis usually manifests as thyroid nodules, but also as a diffuse infiltration of the gland in complementary studies conducted in patients with a malignant tumour.9 The sudden appearance of a fast-growing goitre that is hard on palpation and associated with dysphonia makes it necessary to rule out this possibility.
There are no specific clinical or radiological characteristics that enable us to distinguish whether a thyroid nodule is part of primary or metastatic thyroid disease. However, because FNA is increasingly being performed to assess thyroid disease, diagnosis of a non-thyroid primary tumour will increasingly be observed as the first clinical manifestation. One of the areas of confusion lies in the difficulty in interpreting cytology to differentiate between a primary anaplastic thyroid carcinoma and a metastasis of a high-grade carcinoma, for which immunohistochemistry is very useful.
In the case of an isolated metastasis, most authors recommend total thyroidectomy, depending on the type of primary tumour and the extent of the metastasis.5,10 Confirmation of thyroid metastasis yields a worse prognosis.5,9,10
Due to the complexity of clinical suspicion and the therapeutic decision to follow, and given the scarcity of literature, a multidisciplinary approach involving endocrinologists, oncologists, pathologists and radiologists is important.