Diabetic ketoacidosis (DKA) is a potentially life-threatening complication of diabetes mellitus characterized by hyperglycemia, high-anion anion gap metabolic acidosis, and the presence of ketone bodies. The most common causes are non-adherence to treatment and infections.1 Hospital admissions have increased over the last decades with a mortality of 1% in developed countries2 to 30% in low-income countries.3,4 Complications include hypoglycemia and serum electrolyte disturbances, with potassium being the most commonly affected.5We report our ten-year experience of patients with DKA at an academic center in northeast Mexico.
This retrospective study includes 329 subjects diagnosed with DKA from January 2009 to March 2019 at the “Dr. José E. González” University Hospital of the School of Medicine of the Universidad Autónoma de Nuevo León in Monterrey, México. All subjects who presented to the emergency room and fulfilled the diagnostic criteria of DKA6 were included. Treatment strategies and resolution criteria were selected by each treating physician according to The American Diabetes Association guidelines.6 Mild DKA was categorized by a ph level of 7.25–7.30 and serum bicarbonate between 15 and 18mEq/l, moderate DKA was categorized by a pH level between 7.0 and 7.24 and serum bicarbonate between 10 and 14mEq/l; and severe DKA as patients with pH lower than 7.0 and a serum bicarbonate lower than 10mEq/l. For this analysis, the resolution criteria were guided by current recommendations.6 Hyperkalemia was defined as a potassium level>5mmol/L and clinically relevant hyperkalemia as>6mmol/L. Hypokalemia was defined as a potassium level<3.5mmol/L and relevant hypokalemia as <3.3mEq/L.
The protocol was reviewed and approved by our local IRB, and the need for informed consent was waived. All relevant information was obtained from clinical records. Descriptive analyses were done using frequencies (%) and medians (q25–q75) or means±SD, accordingly. Comparisons of quantitative variables were done using ANOVA. All statistical analysis was done using SPSS version 22.0 (IBM SPSS Statistics for Windows, IBM Corp., Armonk, NY), considering a p-value<0.05 significant.
A total of 329 subjects with DKA were included in our analysis. Subjects had a median age of 32 years (range: 18–90) and 169 (51.4%) were women. Regarding initial biochemical characteristics, blood glucose was 475.6±202.4mg/dL, pH was 7.08±0.15, serum bicarbonate was 7.7±4.4mmol/L and the anion gap was 23.8±6.7mmol/L. No significant difference was found between genders in clinical or biochemical features.
Regarding DKA severity, 236 (71.7%) cases were classified as severe, 73 (22.2%), as moderate and 20 (6.1%) as mild. Of the entire group, 10 (3%) subjects presented hypokalemia, 36 (10.9%) significant hypokalemia, and 6 (1.9%) severe hypokalemia. Hyperkalemia was found in 67 (20.40%) patients, severe hyperkalemia in 28 (8.51%), and the rest had normal potassium levels. Mean serum glucose was 550.5±224.2mg/dL in subjects with hyperkalemia, 454.5±177.9mg/dL in those with normal potassium, and 410.2±205.3mg/dL in subjects with hypokalemia (p<0.001).
Hypoglycemia occurred in 27 (8.2%) patients during treatment. There were no cases of brain edema in our group. Of the whole cohort, time to resolution of DKA was 26h and 22min with a standard deviation of ±18h and 10min. A total of 8 (2.4%) deaths were documented; all of these associated with septic shock.
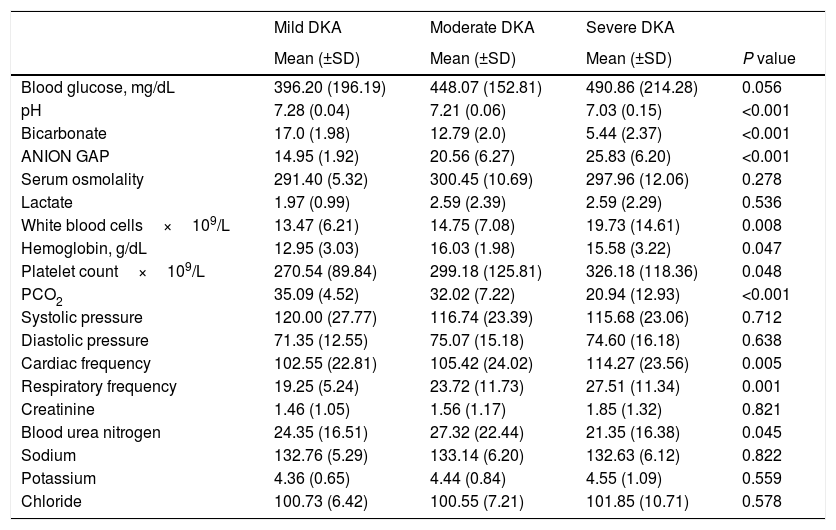
Clinical and laboratory features between mild, moderate and severe DKA were compared. As expected, statistically significant differences were found in pH, serum bicarbonate, and anion gap (p<0.05). Significant differences were also found in hemoglobin, white blood cells, platelets, PCO2, heart rate, respiratory rate, and blood urea nitrogen. Complete data are shown in Table 1.
Comparison of mean values of clinical and laboratory in mild, moderate and severe diabetic ketoacidosis (DKA) at diagnosis. ANOVA test.
| Mild DKA | Moderate DKA | Severe DKA | ||
|---|---|---|---|---|
| Mean (±SD) | Mean (±SD) | Mean (±SD) | P value | |
| Blood glucose, mg/dL | 396.20 (196.19) | 448.07 (152.81) | 490.86 (214.28) | 0.056 |
| pH | 7.28 (0.04) | 7.21 (0.06) | 7.03 (0.15) | <0.001 |
| Bicarbonate | 17.0 (1.98) | 12.79 (2.0) | 5.44 (2.37) | <0.001 |
| ANION GAP | 14.95 (1.92) | 20.56 (6.27) | 25.83 (6.20) | <0.001 |
| Serum osmolality | 291.40 (5.32) | 300.45 (10.69) | 297.96 (12.06) | 0.278 |
| Lactate | 1.97 (0.99) | 2.59 (2.39) | 2.59 (2.29) | 0.536 |
| White blood cells×109/L | 13.47 (6.21) | 14.75 (7.08) | 19.73 (14.61) | 0.008 |
| Hemoglobin, g/dL | 12.95 (3.03) | 16.03 (1.98) | 15.58 (3.22) | 0.047 |
| Platelet count×109/L | 270.54 (89.84) | 299.18 (125.81) | 326.18 (118.36) | 0.048 |
| PCO2 | 35.09 (4.52) | 32.02 (7.22) | 20.94 (12.93) | <0.001 |
| Systolic pressure | 120.00 (27.77) | 116.74 (23.39) | 115.68 (23.06) | 0.712 |
| Diastolic pressure | 71.35 (12.55) | 75.07 (15.18) | 74.60 (16.18) | 0.638 |
| Cardiac frequency | 102.55 (22.81) | 105.42 (24.02) | 114.27 (23.56) | 0.005 |
| Respiratory frequency | 19.25 (5.24) | 23.72 (11.73) | 27.51 (11.34) | 0.001 |
| Creatinine | 1.46 (1.05) | 1.56 (1.17) | 1.85 (1.32) | 0.821 |
| Blood urea nitrogen | 24.35 (16.51) | 27.32 (22.44) | 21.35 (16.38) | 0.045 |
| Sodium | 132.76 (5.29) | 133.14 (6.20) | 132.63 (6.12) | 0.822 |
| Potassium | 4.36 (0.65) | 4.44 (0.84) | 4.55 (1.09) | 0.559 |
| Chloride | 100.73 (6.42) | 100.55 (7.21) | 101.85 (10.71) | 0.578 |
A subgroup of 52 patients with significant hypokalemia during treatment was studied; after a median of 6 units per hour of continuous insulin infusion, and a potassium replacement of 10mEq per hour, only 5 (9.6%) did not improve to >3.3mEq/L of potassium in the next measurement of serum electrolytes.
Even though DKA is a well-known complication of diabetes mellitus, data on clinical and biochemical features are scarce. Similar to a previous study from Canadian institutions,7 severe DKA was frequent, but a lower mean pH was found in our group. This could be due to the greater number of uninsured patients in our population, who commonly delay seeking medical attention.
Hypoglycemia during treatment is a known and frequent concern. In a study from the UK more than 25% of patients8,9 had a serum glucose level below 70mg/dL. This event was only present in 8.2% of our patients. The mortality rate in our group was 2.4%, slightly higher than that reported in high-income countries6 but significantly lower than others.3,4
Interestingly, almost half of the patients in our cohort presented at the emergency department with serum potassium abnormalities. In this respect, insulin plays a determinant role for cellular potassium regulation, promoting its influx from the extracellular compartment. Hypokalemia is also worsened by increased diuresis after aggressive IV hydration, vital in the management of DKA. Furthermore, in subjects with DKA, sodium is retained at the expense of augmented potassium excretion, and renal loss of potassium is also magnified by the accompanying acidosis.1 Hypokalemia on admission was traditionally documented as an uncommon event10; however, this affirmation was completely different in our population. Mortality attributable to this electrolyte disturbance is infrequent, and in this respect, none of the deaths in our cohort were associated with this complication. We documented this and other problems in our Mexican cohort where diabetes mellitus is a current health problem. Nevertheless, complications during treatment of DKA need to be further evaluated in a prospective manner. Some limitations in our study are its single center and retrospective design and the absence of follow-up after discharge. Some of the strengths are the considerable number of patients included and strict adherence to the American Diabetes Association guidelines.
In conclusion, DKA is a serious but preventable complication of diabetes mellitus; similarities to other groups regarding mortality, clinical, and biochemical features were found. Nevertheless, a higher than expected prevalence of severe DKA was found. In addition, potassium disturbances tend to be more frequent but none of them were directly associated with mortality.
Conflict of interestThe authors declare no conflict of interest.
We thank Sergio Lozano-Rodriguez, M.D., for his critical reading and collaboration in the edition of this manuscript.