Thyroid nodule (TN) is a common reason for consultation in daily practice. The purpose of this study was to evaluate the diagnosis and treatment of TNs in our environment and to assess the current status regarding the existence and structure of high-resolution TN clinics.
Material and methodsMembers of the Spanish Society of Endocrinology and Nutrition were invited in 2018 to participate in an online survey on the diagnostic and therapeutic processes of TN.
ResultsA total of 211 valid surveys were received. Of all respondents, 30.8% stated that there were high-resolution TN clinics in their environment, with the endocrinologist being the main person responsible for performing ultrasonography (87.7%) and fine needle aspiration (FNA) (69.2%). For ultrasound classification of TNs, 32.7% used the ATA criteria, 32.2% the TI-RADS criteria, and 22.7% no classification. In situ verification of sample suitability was performed in 35.5% of the cases, and molecular analysis in 8.1%. With regard to clinical discharge, 65.4% would consider it after 5 years of follow-up and with a benign FNA. In the event of a Bethesda III result, 50.2% of respondents would repeat FNA and 35.5% would opt for surgery; if a Bethesda IV result was found, 95.8% would opt for surgery.
ConclusionsHigh-resolution TN clinics are structures increasingly implemented in our environment where the endocrinologist is the main person responsible for performing ultrasonography and FNA. The standard clinical practice in our specialty is consistent with most recommendations concerning clinical practice guidelines for TNs.
El nódulo tiroideo (NT) es un motivo de consulta frecuente en la práctica diaria. El objetivo de este estudio es conocer el proceso diagnóstico y terapéutico del NT en nuestro medio y evaluar el estado actual sobre la existencia y estructura de las consultas de alta resolución de NT.
Material y métodosLos miembros de la Sociedad Española de Endocrinología y Nutrición fueron invitados en el año 2018 a participar en una encuesta online sobre los procesos diagnósticos y terapéuticos del NT.
ResultadosSe recibieron 211 encuestas válidas. El 30,8% de los encuestados indicaron que existía consulta de alta resolución de NT en su medio, siendo el endocrinólogo el responsable mayoritario de realizar la ecografía (87,7%) y la punción-aspiración con aguja fina (PAAF) (69,2%). Respecto a la clasificación ecográfica, el 32,7% utilizaban criterios ATA y el 32,2% criterios TI-RADS (el 22,7% no utilizaba ninguna clasificación). El 35,5% comprobaban in situ la idoneidad de la muestra y el análisis molecular en el 8,1%. El 65,4% plantearían alta del NT tras 5 años de seguimiento y PAAF benigna. Ante un Bethesda III, el 50,2% de los encuestados repetirían la PAAF y un 35,5% optarían por cirugía; ante un Bethesda IV, el 95,8% optarían por cirugía.
ConclusionesLa consulta de alta resolución de NT es una estructura con una creciente introducción en nuestro medio, siendo el endocrinólogo el responsable fundamental de realizar la ecografía y la PAAF. La práctica clínica habitual en nuestro medio es concordante con la mayoría de las recomendaciones de las guías de práctica clínica de NT.
A thyroid nodule (TN), defined as a well-differentiated lesion within the thyroid gland radiologically distinct from the surrounding gland parenchyma, is a very common reason for consultation in daily clinical practice, and the detection of such nodules is also increasing as a result of the widespread use of imaging techniques and a growing awareness on the part of healthcare professionals.1,2
The prevalence of thyroid nodules increases linearly with age, radiation exposure, and iodine deficiency. The prevalence of such nodules is 10 times higher in females. Although 4–8% of all adults present thyroid nodules on palpation, the prevalence increases to 20–67% in ultrasound explorations, and to 50% in necropsy studies.2,3
The importance of thyroid nodules is not due to their high prevalence, however, but to the fact that, while most of them are benign, 5–15% correspond to thyroid cancer. The evaluation of a thyroid nodule therefore should essentially focus on ruling out possible malignancy.4
Standard thyroid nodule assessment involves clinical evaluation of the patient (including laboratory tests with thyroid function) and the performance of thyroid ultrasound (determining the ultrasound characteristics of the nodule) and fine needle aspiration biopsy (FNAB), if considered necessary.5 All these tests can be performed at high-resolution thyroid nodule clinics (HRTNCs) or in conventional clinical centers, though the former are possibly a more ideal and efficient option for evaluating thyroid nodules.6
In recent years we have witnessed a very dynamic period characterized by great changes in the evaluation of thyroid nodules, with the publication of several international guides on nodule management, the introduction of new ultrasound risk classifications, and a recent update on the Bethesda cytological classification.7–11
Given these important changes, the Area of Thyroid Knowledge of the Spanish Society of Endocrinology and Nutrition (Sociedad Española de Endocrinología y Nutrición [SEEN]) considered it to be of interest to determine the routine diagnostic and therapeutic process followed in Spain in relation to thyroid nodules, and to examine the current status of the HRTNCs (existence, structure). To this end, a survey was designed, addressing these issues, and was distributed among the members of the SEEN. The present study describes the results of that survey.
Material and methodsDevelopment of the surveyThe thyroid nodule survey started in October 2016, with the identification of a number of issues and situations referring to thyroid nodule management and considered to be relevant. Based on the above, a first version of the survey was drafted and distributed to all the members of the Area of Thyroid Knowledge of the SEEN, with a two-month period for comments and suggestions. After this review and improvement period, a second version of the survey was forwarded to the Steering Committee of the SEEN, which evaluated and approved the final version in April 2017. This final version contained 26 questions (3 on the existence and organization of HRTNCs, 11 on the clinical management of thyroid nodules, and 12 on specific clinical situations). The survey also collected sociodemographic data (age, gender, years of experience, etc.). The survey is available as supplemental material in the online version of the article (Appendix B Annex).
This anonymous survey was distributed in June 2017 to all SEEN members (n = 1694) by means of an e-mail explaining the purpose of the survey and providing instructions for accessing and completing it. In addition, a specific link to the survey was habilitated in the members’ private area of the SEEN website. An e-mail reminder was sent in March 2018 to increase the survey response rate.
Statistical analysisThe deadline for receiving the responses to the survey was 30 June 2018, and the data were then exported to the SPSS version 15.0 statistical package for analysis. Qualitative variables were expressed as absolute numbers and percentages, and associations between them were analyzed using the chi-square test. Statistical significance was considered for p < 0.05.
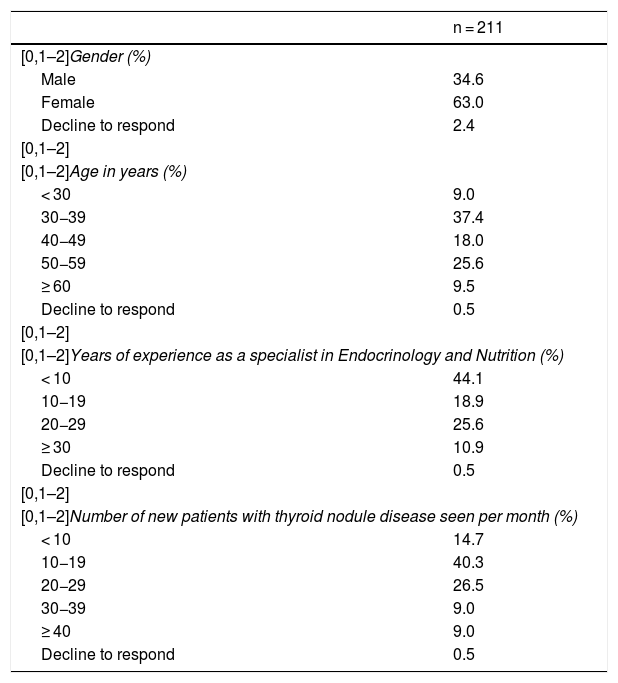
ResultsA total of 211 valid surveys were received. Table 1 shows the sociodemographic characteristics of the people who responded to the survey. Briefly, most of the respondents were women, with a majority of individuals between 30−39 years of age, and with a mean experience as specialists in Endocrinology and Nutrition of less than 10 years. Most of the respondents saw 10−19 new patients with thyroid nodular disease each month.
Sociodemographic characteristics of the respondents of the survey.
| n = 211 | |
|---|---|
| [0,1–2]Gender (%) | |
| Male | 34.6 |
| Female | 63.0 |
| Decline to respond | 2.4 |
| [0,1–2] | |
| [0,1–2]Age in years (%) | |
| < 30 | 9.0 |
| 30−39 | 37.4 |
| 40−49 | 18.0 |
| 50−59 | 25.6 |
| ≥ 60 | 9.5 |
| Decline to respond | 0.5 |
| [0,1–2] | |
| [0,1–2]Years of experience as a specialist in Endocrinology and Nutrition (%) | |
| < 10 | 44.1 |
| 10−19 | 18.9 |
| 20−29 | 25.6 |
| ≥ 30 | 10.9 |
| Decline to respond | 0.5 |
| [0,1–2] | |
| [0,1–2]Number of new patients with thyroid nodule disease seen per month (%) | |
| < 10 | 14.7 |
| 10−19 | 40.3 |
| 20−29 | 26.5 |
| 30−39 | 9.0 |
| ≥ 40 | 9.0 |
| Decline to respond | 0.5 |
In turn, 69.2% of the respondents reported having no HRTNC in their setting, while 30.8% of did have such a center. Among those who reported having HRTNC in their setting, 66.2% claimed to perform ultrasound and FNAB in the same medical procedure, while 33.8% performed FNAB on a delayed basis. Thyroid ultrasound was performed by endocrinologists in most HRTNCs (87.7%), while radiologists performed the technique in only 12.3% of the cases. Likewise, 69.2% of those surveyed answered that the endocrinologist performed FNAB, while 21.5% and 9.2% reported that the technique was performed by radiologists and pathologists, respectively.
As regards the laboratory tests requested as initial assessment of a thyroid nodule, 35.5% of the respondents would choose to request only thyroid-stimulating hormone (TSH) levels, 15.2% would add thyroid peroxidase antibodies (anti-TPO), 16.9% would request TSH and free thyroxine (FT4), and 19.4% would request TSH, FT4 and anti-TPO antibodies. Most of those surveyed (65.9%) would not routinely request calcitonin, but would do so in cases with a family history of medullary carcinoma or a prior or current history of pheochromocytoma or hyperparathyroidism.
In addition, 22.7% of the respondents indicated that they did not use any ultrasound classification system for thyroid nodule malignancy risk, while 32.7% used the criteria of the American Thyroid Association (ATA), 32.2% used the Thyroid Imaging Reporting and Data System (TI-RADS), and only 1.4% used the classification of the British Thyroid Association. The remainder used more than one ultrasound classification.
Regardless of the presence or absence of HRTNC, the FNAB technique was performed by the radiologist in most institutions (69.2%), by the endocrinologist in 24.2%, and by the pathologist in only 5.7% of the cases. Likewise, FNAB was performed under ultrasound guidance in most cases (91.5%). With regard to cytological interpretation, 52.1% of those surveyed replied that it was performed by an expert cytologist, while 47.9% reported that it was performed by a general pathologist. In only 35.5% of the cases was in situ confirmation made of the suitability of the sample for diagnostic purposes.
As regards the mean time to availability of the cytological result, most answered that it was obtained in less than one week (39.3%) or in between 1−2 weeks (37%), while 23.7% reported that the cytological result took over two weeks to become available. Lastly, 93.4% of those surveyed reported using the Bethesda system for cytological classification, while only 8.1% reported using molecular analysis on a routine basis.
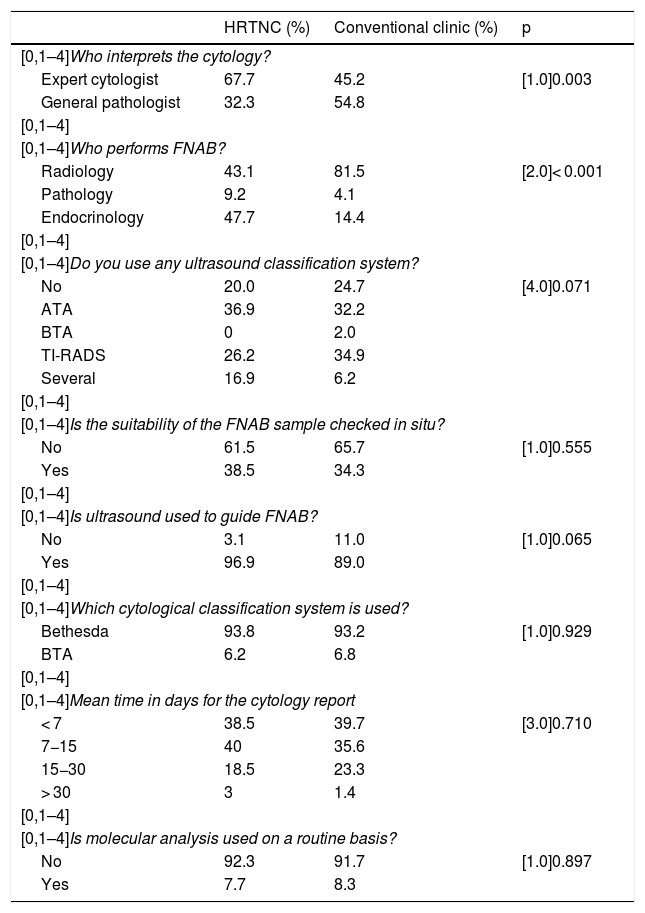
The existence of HRTNC was associated with some clinical differences with respect to centers lacking HRTNC. In effect, FNAB was preferably performed by radiologists in centers without HRTNC (80.8%), while in centers with HRTNC the technique was performed by both radiologists (43.1%) and endocrinologists (47.7%) (p < 0.001 for the comparison between HRTNC and conventional clinics without HRTNC). As regards the interpretation of thyroid cytology, an expert cytologist was more commonly present in centers with HRTNC than in those without (67.7% versus 45.2%; p = 0.002). However, no differences were found between centers with or without HRTNC in the use of ultrasound risk classification systems, cytological classification systems, the use of ultrasound to guide puncture, in situ verification of FNAB sample adequacy, the mean time to availability of the cytological result, or the possibility of performing molecular analyses on a routine basis (Table 2).
Comparative evaluation of centers with and without a high-resolution thyroid nodule clinic (HRTNC).
| HRTNC (%) | Conventional clinic (%) | p | |
|---|---|---|---|
| [0,1–4]Who interprets the cytology? | |||
| Expert cytologist | 67.7 | 45.2 | [1.0]0.003 |
| General pathologist | 32.3 | 54.8 | |
| [0,1–4] | |||
| [0,1–4]Who performs FNAB? | |||
| Radiology | 43.1 | 81.5 | [2.0]< 0.001 |
| Pathology | 9.2 | 4.1 | |
| Endocrinology | 47.7 | 14.4 | |
| [0,1–4] | |||
| [0,1–4]Do you use any ultrasound classification system? | |||
| No | 20.0 | 24.7 | [4.0]0.071 |
| ATA | 36.9 | 32.2 | |
| BTA | 0 | 2.0 | |
| TI-RADS | 26.2 | 34.9 | |
| Several | 16.9 | 6.2 | |
| [0,1–4] | |||
| [0,1–4]Is the suitability of the FNAB sample checked in situ? | |||
| No | 61.5 | 65.7 | [1.0]0.555 |
| Yes | 38.5 | 34.3 | |
| [0,1–4] | |||
| [0,1–4]Is ultrasound used to guide FNAB? | |||
| No | 3.1 | 11.0 | [1.0]0.065 |
| Yes | 96.9 | 89.0 | |
| [0,1–4] | |||
| [0,1–4]Which cytological classification system is used? | |||
| Bethesda | 93.8 | 93.2 | [1.0]0.929 |
| BTA | 6.2 | 6.8 | |
| [0,1–4] | |||
| [0,1–4]Mean time in days for the cytology report | |||
| < 7 | 38.5 | 39.7 | [3.0]0.710 |
| 7−15 | 40 | 35.6 | |
| 15−30 | 18.5 | 23.3 | |
| > 30 | 3 | 1.4 | |
| [0,1–4] | |||
| [0,1–4]Is molecular analysis used on a routine basis? | |||
| No | 92.3 | 91.7 | [1.0]0.897 |
| Yes | 7.7 | 8.3 | |
ATA: American Thyroid Association; BTA: British Thyroid Association; HRTNC: high-resolution thyroid nodule clinic; FNAB: fine needle aspiration biopsy; TI-RADS: Thyroid Imaging Reporting and Data System.
The results referring to the clinical scenarios contemplated in the survey are described below:
1. A 48-year-old woman with no disease history of relevance presented with a thyroid nodule measuring 1.3 cm in size detected by ultrasound. The nodule was hypoechoic, solid, with no other findings, and thyroid function was normal. What would you do? A total of 70.6% of the respondents would request FNAB while 28.4% would re-evaluate the nodule by ultrasound. Likewise, in response to the question of when a new ultrasound exploration would be made if ultrasound re-evaluation was decided upon, 52.6% reported that they would do so within 3–6 months, and 95.7% would do so 12 months after the diagnosis. In this same scenario, the respondents were asked whether their clinical approach would change if the patient were 85 years old and had good quality of life. Sixty-three percent reported that they would be less inclined to request FNAB in such a case, while 37% claimed that their clinical approach would not change.
2. In the case of a 55-year-old male with a hypoechoic solid nodule measuring 2 cm in diameter, with microcalcifications and greater height than width, in which FNAB revealed benign features, what would be your usual approach to follow-up? A total of 60.2% of the respondents would repeat FNAB at the next visit, while the remaining 39.8% would only request repeat FNAB in the event of changes over follow-up.
3. In the case of a patient with a thyroid nodule, which factors would cause you to consider definitive discharge? A total of 8.5% of those surveyed would not discharge a patient with a thyroid nodule, 65.4% would consider definitive discharge after 5 years of follow-up and benign FNAB findings, and 19.4% would consider discharge after at least 10 years of follow-up or two benign FNAB reports.
4. A 42-year-old woman presented with a solitary, solid, hypoechoic thyroid nodule measuring 2.3 cm in size, without calcifications or risk factors. Fine needle aspiration biopsy of the nodule was performed. If the FNAB result corresponded to Bethesda I (non-diagnostic), what would you do? Most of the respondents (89.1%) would repeat FNAB, while 9% would conduct ultrasound follow-up and 1.9% would perform a core needle biopsy or hemithyroidectomy. In the case of repeating FNAB, 68.2% would do so in the first three months, while 28.9% would do so after 6–12 months.
5. If the FNAB result corresponded to Bethesda III (atypia / follicular lesion of undetermined significance), what would you do? In this case, 50.2% would repeat FNAB, while 35.5% would choose the surgical option (preferably hemithyroidectomy). Other possibilities, such as clinical follow-up (5.7%), molecular analysis (3.8%) or core needle biopsy (4.7%), would be minority options.
6. If the FNAB result corresponded to Bethesda IV (follicular neoplasm or suspicious for follicular neoplasm), what would you do? Hemithyroidectomy would be decided upon by 65.9% of the respondents, while 29.9% would indicate total thyroidectomy. Here again, molecular analysis (2.8%) and core needle biopsy (1.4%) were minority options.
7. What clinical factors would influence your decision regarding total thyroidectomy instead of hemithyroidectomy in the case of indeterminate cytological findings (Bethesda III/IV)? In response to this question, most of those surveyed cited the combination of the presence of adenopathies and bilateral nodules as relevant factors (45%), as well as the combination of size, the presence of adenopathies and bilateral nodules (19%).
8. In the case of a 64-year-old woman with no high risk history, diagnosed with multinodular goiter, with ultrasound evidencing at least 6 nodules ranging from 1−2 cm in diameter (distributed in both thyroid lobes) of a solid, hypoechoic nature, no adenopathies and TSH 1.8 μU/mL (normal range 0.5–4), what would you normally do? In this case, 15.2% of those surveyed would choose ultrasound follow-up, 53.6% would request FNAB of the largest nodule, and 16.6% would request FNAB of the dominant nodule in each thyroid lobe.
Lastly, we examined whether there were differences in thyroid nodule management according to the number of new patients seen with nodular disease or to clinical experience. Although no significant differences were observed regarding the number of patients, the respondents with greater clinical experience (> 20 years) would request fewer laboratory tests at the initial evaluation of a nodule (p = 0.013); would more often delay evolutive ultrasound monitoring of a nodule for at least 12 months (p < 0.001); would be less inclined to repeat FNAB in the event of non-diagnostic cytological findings (p = 0.039) (and if they were to do so, would more often wait 6 months; p = 0.002); and would be more conservative (ultrasound control or FNAB only of the dominant nodule) in the study of a multinodulat goiter (p = 0.030).
DiscussionThe present study describes the results of a national survey on thyroid nodule diagnosis and treatment in Spain, promoted by the Area of Thyroid Knowledge of the SEEN. The study evaluated standard diagnostic and therapeutic clinical practice in reference to thyroid nodules, and also compiled information regarding the existence of HRTNCs and their specific organization.
The main aim of the diagnostic evaluation of a thyroid nodule is to rule out malignancy. To this end, it is essential to adopt a cost-effective and systematic approach allowing us to distinguish between benign and malignant nodules.1 After taking the clinical history and conducting the physical examination, we need to decide which supplementary tests should be performed. Although most thyroid nodules are associated with normal thyroid function, at least one TSH measurement should be made. If the result is normal, no additional measurements are required; however, if TSH is found to be elevated, it is advisable to also request FT4 and anti-TPO antibodies. If TSH is seen to be suppressed, in addition to requesting anti-TSH receptor antibodies or Thyroid Stimulating Immunoglobulins (TSI) and free triiodothyronine, we should perform scintigraphy in view of the low risk of malignancy of nodules with enhanced uptake.5,7,12 In this regard, the present survey found that most endocrinologists would determine TSH levels, as indicated by the guidelines, and a considerable number of them would also request some other measurement, preferably anti-TPO antibodies or FT4.
Separate mention should be made of calcitonin, an excellent marker of C-cell hyperplasia, and therefore a parameter of potential clinical value in medullary thyroid carcinoma. However, most clinical guides do not recommend the routine use of calcitonin in the study of thyroid nodules, and its value as a tool for optimizing the diagnosis of medullary carcinoma remains subject to controversy. Measurement of this marker is only recommended if there is evidence of a family history of medullary carcinoma or multiple endocrine neoplasia type 2, or if FNAB suggests possible medullary carcinoma.5,7,13 Similarly, most of the respondents would choose to determine calcitonin mainly in cases of suspected multiple endocrine neoplasia type 2 or a history of medullary carcinoma.
Among the imaging techniques, thyroid ultrasound is the procedure of choice for the study of thyroid nodules, because evaluation of the ultrasound characteristics of the nodule allows us to establish a malignancy risk level, and thus helps to guide our management approach. Since the unification of criteria is essential for interpreting ultrasound images, the different guides7,8 propose ultrasound risk stratification systems, all based on the original TI-RADS of Horvath et al.,9 which has subsequently been modified and optimized by other professional bodies.10 Each system emphasizes certain characteristics and establishes different risk levels that allow definition of the need for FNAB or regular monitoring. The data from the respondents indicate that the use of these classification systems is quite widespread in Spain, with the American Thyroid Association (ATA) classification being the most widely used instrument. This preference might be related to the fact that the ATA classification adopts a more clinical approach and reports on the degree of suspicion more directly (benign, very low suspicion, low suspicion, intermediate suspicion or high suspicion). However, a considerable percentage of centers use no ultrasound classification system (about 23%).
Similarly, in order to unify diagnostic criteria, the guides also recommend the use of a cytological classification for application to thyroid nodules. Although there are classifications other than the Bethesda system,11 the latter is currently the most widely used option, and is recommended by the ATA.7 In this regard, the results of the survey show that the Bethesda classification is the predominantly used system in our setting, regardless of who performs the cytological analysis or whether there is an HRTNC or not.
When assessing a thyroid nodule, it is essential to follow a cost-effective and systematic strategy. Multidisciplinary teams working together in high-resolution units or in coordination with conventional clinics are recommended in this respect.14,15 Accordingly, HRTNCs have been adopted in our setting for a number years, and have been shown to be an efficient and useful option for the evaluation of thyroid nodules.6,16 Likewise, endocrinologists are increasingly being incorporated into thyroid ultrasound as a strategy to optimize the care of patients with thyroid nodule disease.15–17 In our survey, approximately 30% of the respondents worked in the setting of an HRTNC, and the endocrinologist was mostly in charge of performing ultrasound and FNAB. These data should be interpreted with caution, however, because the respondents could be particularly interested in thyroid nodule disease. Furthermore, many of them may even be dedicated to thyroid nodules in HRTNCs, and if so, the real implementation of HRTNCs in our setting is less than that reported in the survey. In any case, as seen from our results, it does seem to be more common for endocrinologists to be involved in performing ultrasound and FNAB in the presence of an HRTNC, and the presence of an expert cytologist in these monographic clinics is also more frequent.
Lastly, through a series of clinical scenarios, we explored whether the daily clinical practice of the respondents complied with the recommendations of the most commonly used guides on the management of thyroid nodules. In the first of these scenarios, involving a nodule of intermediate suspicion due to its hypoechogenicity in a 48-year-old woman, we found most of the respondents to abide with the recommendations of the ATA7 or the Korean TI-RADS10 - though almost 30% of them would opt for ultrasound reassessment of the nodule. On the other hand, the guides recommend ultrasound follow-up of all intermediate suspicion nodules, regardless of whether FNAB is performed or not. In this respect, most of the respondents agreed in doing so within the first year after diagnosis. Although there is no consensus among the different guides on the frequency of follow-up, most of the respondents preferred to conduct follow-up over the short-middle term. On changing the above scenario to a patient with an age of 85 years, more than half of the respondents would adopt a more conservative approach, probably considering an eventual diagnosis of malignancy in an elderly patient to be of lesser clinical relevance.
The second clinical scenario corresponded to a 55-year-old patient with a highly suspicious nodule measuring 2 cm in size, with benign FNAB findings. In this situation, the guides recommend puncture in nodules over 1 cm in size and, in the case of benign cytological findings, advise the repetition of FNAB within 6–12 months.7 It should be noted, however, that almost 40% of the respondents would not repeat FNAB unless the nodule shows changes over ultrasound follow-up.
In another clinical scenario we explored respondent attitudes toward certain cytological findings in a nodule of intermediate suspicion in a 42-year-old woman. It is interesting to note that most of the respondents would repeat FNAB if the cytological findings were non-diagnostic (Bethesda I), and moreover would do so early (in the first 3–6 months), as recommended by the ATA guide.7 However, a small proportion of respondents would not repeat FNAB, and would conduct ultrasound follow-up instead. This could also be a valid option considering that the nodule was not of high suspicion and that there were no associated risk factors in this scenario. If this same nodule were to exhibit cytological features consistent with atypia of undetermined significance (Bethesda III), the respondents mostly agreed with the ATA guide, which recommends monitoring with ultrasound and/or FNAB.7 However, approximately 35% would opt for diagnostic surgery. Lastly, with regard to the above, if cytology is indicative of follicular neoplasm/suspected follicular neoplasm (Bethesda IV), the standard recommendation of the clinical guides is to perform surgery, the extent of which may vary depending on the characteristics and preferences of each patient.7 Over 60% of the respondents described hemithyroidectomy as their preferred option. It also should be noted that a considerable proportion of those surveyed considered the presence of adenopathies or lesion size to be important elements in deciding on total thyroidectomy, these being clearly established risk factors according to the different clinical guides.7,8,10 The presence of bilateral nodules was also considered important by many respondents in deciding on total thyroidectomy. Although it is true that the risk of malignancy in multinodular goiter is similar to that in single nodules, this preference for total thyroidectomy in the presence of indeterminate cytology findings may be explained by the intention to avoid two-step surgeries, which can be associated with greater postoperative complications.
Likewise in relation to multinodular presentations, we considered a case of multinodular goiter. In this scenario, the guides usually recommend an analysis of the larger nodules or of nodules with features of malignancy in each gland lobe, except in the case of very low suspicion nodules of a coalescent nature and with very little healthy parenchyma between them, where ultrasound monitoring is the preferred option.7,8,10 However, only 16% of the respondents in our study would perform FNAB in both lobes, most choosing only to analyze the largest nodule.
Finally, a comparison of the results according to clinical experience or to the number of new patients yielded interesting data. In effect, it was seen that the most experienced respondents would request fewer laboratory tests, would delay ultrasound monitoring longer, would be less inclined to repeat a non-diagnostic FNAB, and would be more conservative in their study of multinodular goiter. We consider these results to be logical, since clinical experience possibly influences clinical practice and diagnostic-therapeutic decisions. Thus, it is plausible to think that the clinical practice of physicians with greater experience is not so closely tied to the recommendations of the clinical guides/consensuses but is more conditioned by personal experience and good clinical judgment developed over the years of practice.
Our study has some limitations that should be mentioned. The main limitation is the relatively low response rate obtained (211 valid surveys received out of a total of approximately 1700 SEEN members; a 12.4% response rate). In this regard, it should be noted that the SEEN is not only made up of clinical endocrinologists; other professionals such as family physicians, pediatricians, biologists, etc. also participate. Furthermore, a significant proportion of endocrinologists might not have considered answering the survey because their routine clinical practice has little to do with thyroid disease (preferential dedication to nutrition, diabetes, obesity, teaching, or no clinical activity). Moreover, the relatively low response rate we obtained in this survey is a common situation that may be attributable to a lack of time/interest among the potential participants. In this respect, in a 2015 survey of more than 19,000 members of the ATA, the Endocrine Society and the American Association of Clinical Endocrinologists, a total of 821 valid responses were obtained, corresponding to a response rate of 4.12% (i.e., clearly lower than our own).18 Another possible limitation of our study refers to potential bias derived from the fact that the survey respondents may have been professionals who are personally more interested in thyroid nodule disease or who even work in an HRTNC. The strengths of the survey include its nationwide nature, which affords an overall picture of the management of thyroid nodules in our setting, and also evaluates the current status of HRTNCs.
In conclusion, the present survey on the management of thyroid nodules in Spain has found standard clinical practice in our setting to be consistent with most of the recommendations of the clinical practice guides on thyroid nodules, though there are some areas amenable to improvement. The HRTNC is an entity with a growing presence in our setting, and endocrinologists are the professionals mainly responsible for performing ultrasound and FNAB.
Financial supportAna María Gómez-Pérez is the holder of a contract for the reinforcement of research activity of the Andalusian Health Service (Servicio Andaluz de Salud [SAS]) (B-0033-2014); José Carlos Fernández-García has a contract as clinical investigator of the SAS (B-0003-2017).
Conflicts of interestThe authors declare that they have no conflicts of interest in relation to this article.
Thanks are due to all the people who spent their valuable time answering the survey.
Please cite this article as: Gómez-Pérez AM, Fernández-García JC, Iglesias P, Díez JJ, Álvarez-Escolá C, Lecumberri B, et al. Diagnóstico y tratamiento del nódulo tiroideo en España. Resultados de una encuesta nacional. Endocrinol Diabetes Nutr. 2019. https://doi.org/10.1016/j.endinu.2019.10.003