The expanding use of 18F-fluorodeoxyglucose (FDG) positron emission tomography-computed tomography (PET-CT) has resulted in an increased frequency of incidentally discovered areas of FDG uptake within the thyroid gland. In these incidentalomas, high malignancy rates are reported. The study aimed, on the one hand, to determine the prevalence in our setting of thyroid incidentalomas in patients with no previous history of thyroid cancer undergoing an FDG PET-CT as well as the risk of malignancy and, on the other hand, to evaluate the usefulness of the maximum standard uptake value (SUVmax) for detecting thyroid cancer.
Material and methodsThe FDG PET-CT scans performed at our hospital between June 2013 and December 2020 were retrospectively reviewed. In those incidentalomas with sufficient additional investigation, a diagnosis of benign or malignant was established based on the complementary tests.
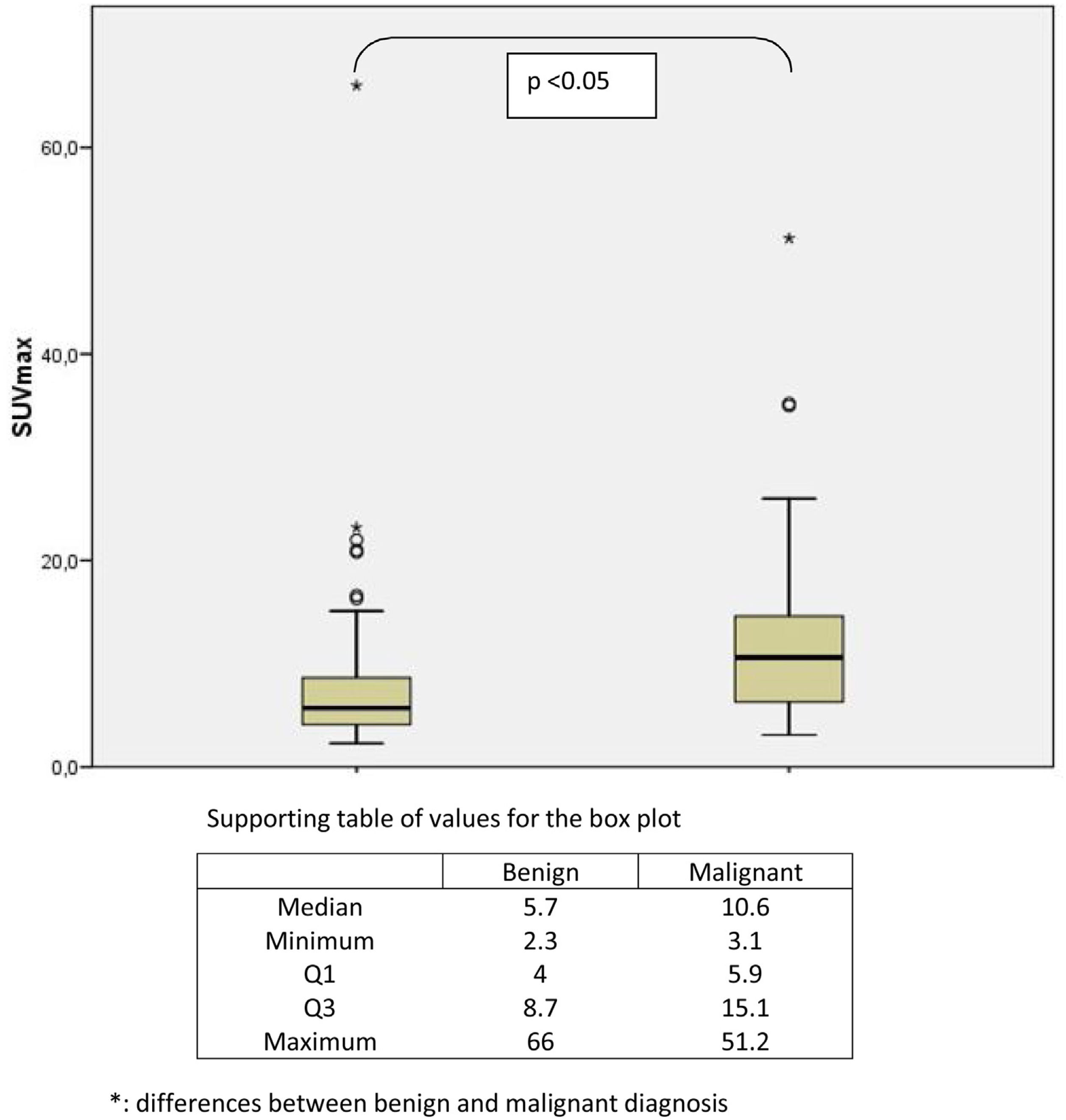
ResultsFrom the 21,594 PET-CT scans performed, 398 (1.8%) patients had an incidental FDG uptake, either focal (n=324) or diffuse (n=74). Among incidentalomas with further investigation, the rate of malignancy was higher in patients with focal FDG uptake than in those with diffuse uptake (26.5% versus 4%, respectively, p<0.05). The SUVmax value was significantly lower in benign focal lesions (5.7 [range: 2.3–66] than in malignant ones 10.6 [range: 3.1–51.2]; p<0.05). Nearly a quarter of malignant diagnoses (23.3%) were related to potentially aggressive tumours.
ConclusionThe high rate of malignant tumours found among PET-CT incidentalomas and the high proportion of aggressive tumours demonstrate the need for a standardised approach in the investigation of incidental focal FDG uptake in the thyroid gland.
El empleo creciente de la tomografía por emisión de positrones con tomografía computarizada (PET/TC) con 18F-fluorodesoxiglucosa (FDG) ha llevado al descubrimiento incidental de áreas de captación de FDG dentro de la glándula tiroidea, cada vez más frecuente. En estos incidentalomas, las tasas de malignidad descritas son elevadas. Los objetivos del estudio incluyeron, por un lado, conocer la prevalencia en nuestro medio de los incidentalomas tiroideos en pacientes sin antecedentes de cáncer de tiroides sometidos a una prueba de PET-TC con FDG, así como el riesgo de malignidad, y por otro lado, evaluar la utilidad del máximo valor normalizado de captación (SUVmáx) en la detección de malignidad.
Material y métodosSe revisaron de manera retrospectiva los PET-TC con FDG llevados a cabo en nuestro centro entre junio de 2013 y diciembre de 2020. En aquellos incidentalomas con investigación adicional suficiente se estableció un diagnóstico de benignidad o de malignidad de acuerdo con las pruebas complementarias.
ResultadosEn los 21.594 pacientes con PET-TC realizados, 398 (1,8%) presentaban una captación incidental de FDG, ya sea focal (n=324) o difusa (n=74). Entre los incidentalomas con investigación adicional, la tasa de malignidad resultó mayor en aquellos con captación focal de FDG que aquellos con captación difusa (26,5 vs. 4%, respectivamente, p<0.05). El valor de SUVmáx resultó significativamente menor en las lesiones focales benignas (5,7 [rango: 2,3-66] que en las malignas (10,6 [rango: 3,1-51,2]; p<0,05). Casi una cuarta parte de los diagnósticos de malignidad (23,3%) se relacionaron con tumores potencialmente agresivos.
ConclusiónLa elevada tasa de tumores malignos hallados entre los incidentalomas del PET-TC y la alta proporción de tumores agresivos hacen precisa una aproximación estandarizada en la investigación de las captaciones incidentales focales de FDG en la glándula tiroidea.
The indications for 18F-fluorodeoxyglucose (FDG) positron emission tomography-computed tomography (PET-CT) in the investigation of oncological1 and inflammatory2 diseases are increasing. As the number of FDG-PET scans performed rises, more unexpected FDG uptakes are reported, including those within the thyroid gland.3 In subjects without known thyroid pathologies, the prevalence of focal uptake varies from 0.1% to 4.8% among studies.4 Diffuse uptake, in 0.1–4.5% of PET-CT, has been related to benign processes such as chronic thyroiditis, Graves’ disease, and multinodular goitre.5 These thyroid incidentalomas are added to those already described in other imaging modalities, such as cervical CT, magnetic resonance imaging, and ultrasonography (US), in which they are reported in 16%6 and 19–46%7 of cases, respectively. In two reviews, the average malignancy rates of focal incidentalomas revealed with PET or PET-CT were similar (34.8% and 34.6%).4,8 but with a broad range of prevalence among different publications. This risk of malignancy is higher than in incidental thyroid nodules identified on other imaging modalities, such as US (from 4.4% to 12%).9,10 Even so, almost two-thirds of PET focal uptakes within the thyroid gland are related to benign diseases. Consequently, to differentiate between malignant and benign thyroid lesions, many researchers have evaluated the usefulness of semi-quantitative parameters used in PET, such as the maximum standard unit value (SUVmax), with highly discrepant conclusions.8 The wide disparity in this outcome and the heterogeneity reported on the prevalence of incidental thyroid uptakes led to a study in our environment. The study aimed to evaluate the prevalence of incidental thyroid uptakes (focal and diffuse) observed in PET-CT performed on patients without previously detected thyroid carcinoma and to analyse the risk of malignancy of incidentalomas and the usefulness of SUVmax for differentiating between benign and malignant lesions.
Material and methodsSubjectsThis retrospective study was conducted on all patients older than 18 years who underwent an FDG PET-CT from June 2013 to December 2020 at the Nuclear Medicine Division of Clínico San Carlos Hospital (Madrid, Spain) to identify subjects with thyroid incidentalomas. The study was approved by the institutional ethical committee (Comité Etico de Investigación Clínica GAE HCSC Area 7). Thyroid incidentaloma was defined as either focal (in less than one lobe) or diffuse (uptake in the whole gland) FDG uptake within the thyroid gland in subjects without a previous diagnosis of thyroid cancer. Patients with more than one examination during the study period were counted only once. Results were initially extracted from all PET-CT reports containing the word ‘thyroid’ in the radiology information system database using a keyword search. Those reports that mentioned thyroid but no underlying thyroid FDG uptake and those scans performed to investigate a known primary thyroid malignancy were excluded. Patients’ electronic records were reviewed to collect demographic and clinical data. Two possible indications for PET-CT were established (staging or restaging of a previously known malignancy, or other indication) and the pattern of FDG uptake was classified into focal or diffuse. Thyroid function, when available, was divided into normal function or thyroid dysfunction, including hypothyroidism and hyperthyroidism, according to thyroid-stimulating hormone (TSH) and free thyroxin (FT4) values close to the time when the PET-CT procedure was performed. Four US pattern categories were considered, based on the recommended American Thyroid Association (ATA) nodule sonographic patterns, in cases when US examination was performed close to the PET-CT11: very low risk US category (normal and ATA benign or very low suspicion pattern), US low risk category (ATA low suspicion pattern), US intermediate category (ATA intermediate suspicion pattern) and US high risk category (ATA high risk suspicion pattern). FNAC (fine-needle aspiration cytology), when performed, was classified as conclusive or inconclusive FNAC when it fell in the Bethesda Categories II or VI12 or in Bethesda Categories I, III, IV or V, respectively. In cases with more than one FNAC, only one result was collected: the conclusive result when available or the first FNAC result when repeated FNACs were inconclusive. The final benign or malignant histopathological diagnosis at the time of thyroid surgery was registered.
PET-CT procedure and interpretationImaging was performed on PET-CT equipment (Biograph 6 True Point, Siemens). Patients fasted 4–6h before PET imaging and had a blood glucose level of less than 200mg/dl before the examination. Image acquisition, from the top of the skull to the mid-thigh, started 60min after the injection of 5Mbq/kg of 18F-FDG. The CT scan was acquired using iodine intravenous contrast, provided there was no contraindication. Abnormal FDG uptake was examined both qualitatively (higher accumulation compared to the contralateral lobe or surrounding soft tissue) and quantitatively (SUVmax determination). The SUVmax values were calculated by drawing regions of interest around the hypermetabolic lesions after adjustment for administered activity per unit of body weight. Two trained physicians evaluated each study with a consensus interpretation when needed.
US evaluation and US-guided FNACNeck US studies were generally performed in the Department of Radiology with a 7.5-MHz linear transducer (Toshiba, Aplio 300). All studies were retrospectively reviewed by a radiologist specialised in thyroid imaging. After the evaluation of distinct features, a radiologic pattern was assigned according to the ATA nodule sonographic patterns11 as described before. FNACs were performed for suspected nodules when requested and were interpreted and classified as category I to VI following the Bethesda System by experienced pathologists.12
Benign or malignant incidentaloma diagnosisSubjects with adequate further investigations were assigned to benign or malignant diagnosis. Benign diagnosis (BD) was established in patients in whom histopathology was reported as benign after lobectomy or thyroidectomy, and in patients who did not undergo surgery with nodule FNAC that fell into Bethesda Category II or with US imaging classified in the US very low risk category and consequently not submitted to FNAC. Malignant diagnosis (MD) was defined when histopathology was reported as malignant after thyroid surgery or FNAC was classified as Bethesda Category VI despite no thyroid surgery.
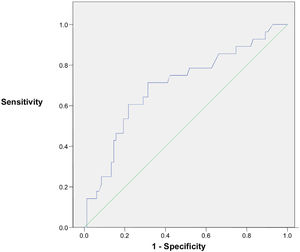
Statistical analysisAll statistical analyses were carried out using SPSS software (version 15.0). Quantitative variables were expressed as mean±standard deviation or median and range (minimum–maximum) as appropriate. Categorical variables were expressed as percentages or frequencies. The Mann–Whitney test was used to compare the values of SUVmax and nodule size between thyroid incidentalomas with BD and MD. A Spearman r test was performed for the correlation between SUVmax and nodule size. Receiver operating characteristic (ROC) analysis was used to identify the best SUVmax cut-off point for discriminating between BD and MD. Tests were considered significant given overall p<0.05.
ResultsPatientsFrom June 2013 to December 2020, a total of 21,696 patients underwent a PET-CT study in the Department of Nuclear Medicine of our institution. Of these, 172 subjects with a history of thyroid cancer were excluded. From the remaining 21,524, a total of 398 (1.8%) had an incidental thyroid uptake that was either focal (n=324) or diffuse (n=74). The baseline characteristics of patients are described in Table 1 for the whole group, and the focal and diffuse subgroups. The mean age of the patients was 67±13 years at the time of the examination with 66.8% being women. The percentage of women with diffuse incidentalomas was higher than those with focal incidentalomas (78.4% and 64.2%, respectively, p<0.05). The prevalence of incidentalomas was similar, independently of the PET indication. Staging or restaging of a previously known malignancy represented the principal PET-CT indication (79.6%), with breast and lung carcinomas being the most prevalent primary tumours (in 96 and 60 cases, respectively), followed by colorectal carcinomas (38), lymphoproliferative disorders (33), melanomas (17), gynaecologic cancer (15), head and neck carcinomas (14), other gastrointestinal tumours (13), urologic cancer (7) and other miscellaneous tumours (23). Most patients had normal thyroid function (76.1%). Thyroid dysfunction was more common in the diffuse incidentaloma subgroup (33.8%) than in the focal subgroup (21.6%, p<0.05). SUVmax and nodule size values were similar between subgroups with a median of 5.7 (range: 1.7–67) for SUVmax and 12mm (range: 0–55) for US size. Among patients with available US imaging (n=204), 16 had no US-proven nodule in the corresponding FDG uptake.
Baseline characteristics of patients with thyroid incidentalomas.
| Whole group(n=398) | Focal uptake group(n=324) | Diffuse uptake group(n=74) | p# | |
|---|---|---|---|---|
| Sex | ||||
| Female/male(%) | 266/132(66.8%/33.2%) | 208/116(64.2%/35.8%) | 58/16(78.4%/21.6%) | <0.05 |
| Years | ||||
| Mean±SD | 67±13 | 68±13 | 66±12 | NS |
| PET indication | ||||
| Staging/restaging* | 79.6% | 79.6% | 79.7% | NS |
| Other indications | 20.4% | 20.4% | 20.3% | |
| Nodule size (mm) | ||||
| Median (min–max) | 12 (0–55) | 12 (0–55) | 10 (0–42) | NS |
| SUVmax | ||||
| Median (min–max) | 5.7 (1.7–67) | 5.7 (1–67) | 5.1 (2.1–32.9) | NS |
| Thyroid functional status | ||||
| Available in (n) | 352 | 287 | 65 | |
| Normal (%) | 76.1% | 78.4% | 66.2% | |
| Dysfunction (%) | 23.9% | 21.6% | 33.8% | <0.05 |
NS: not significant.
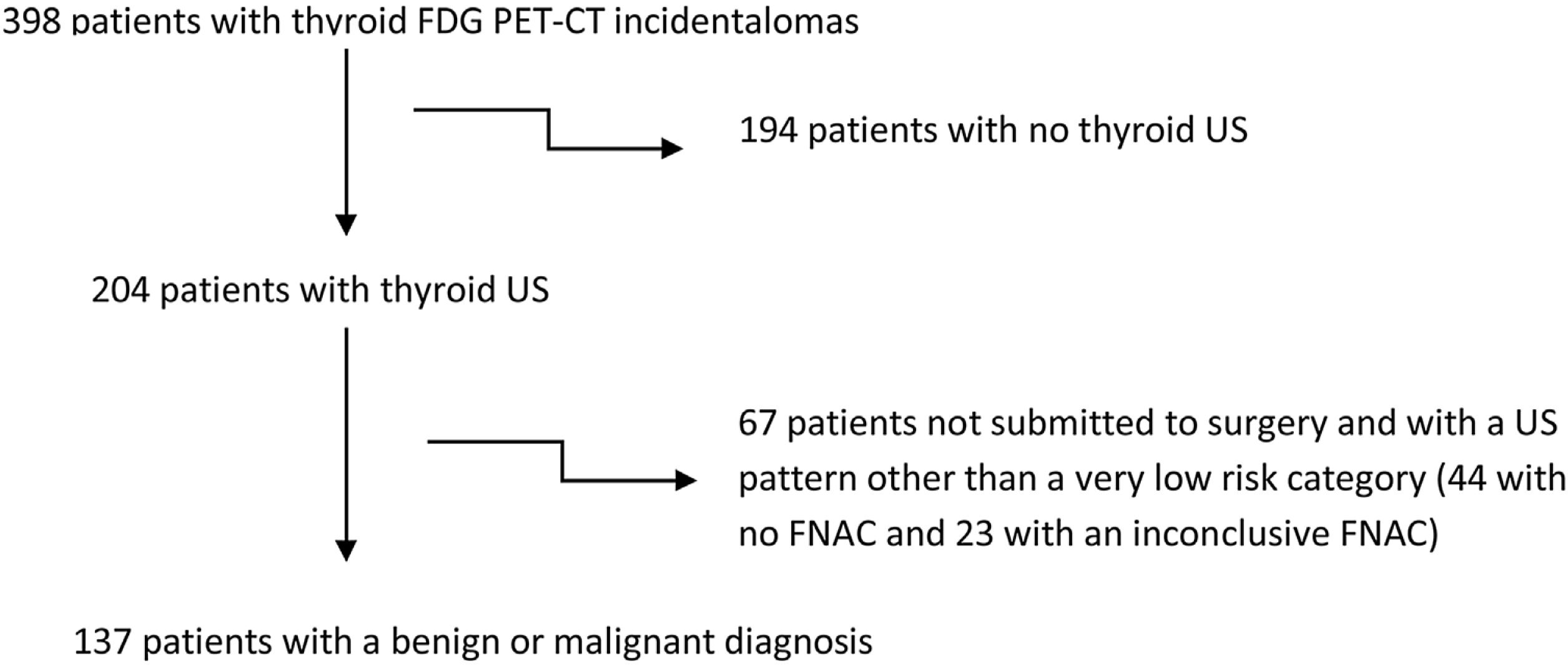
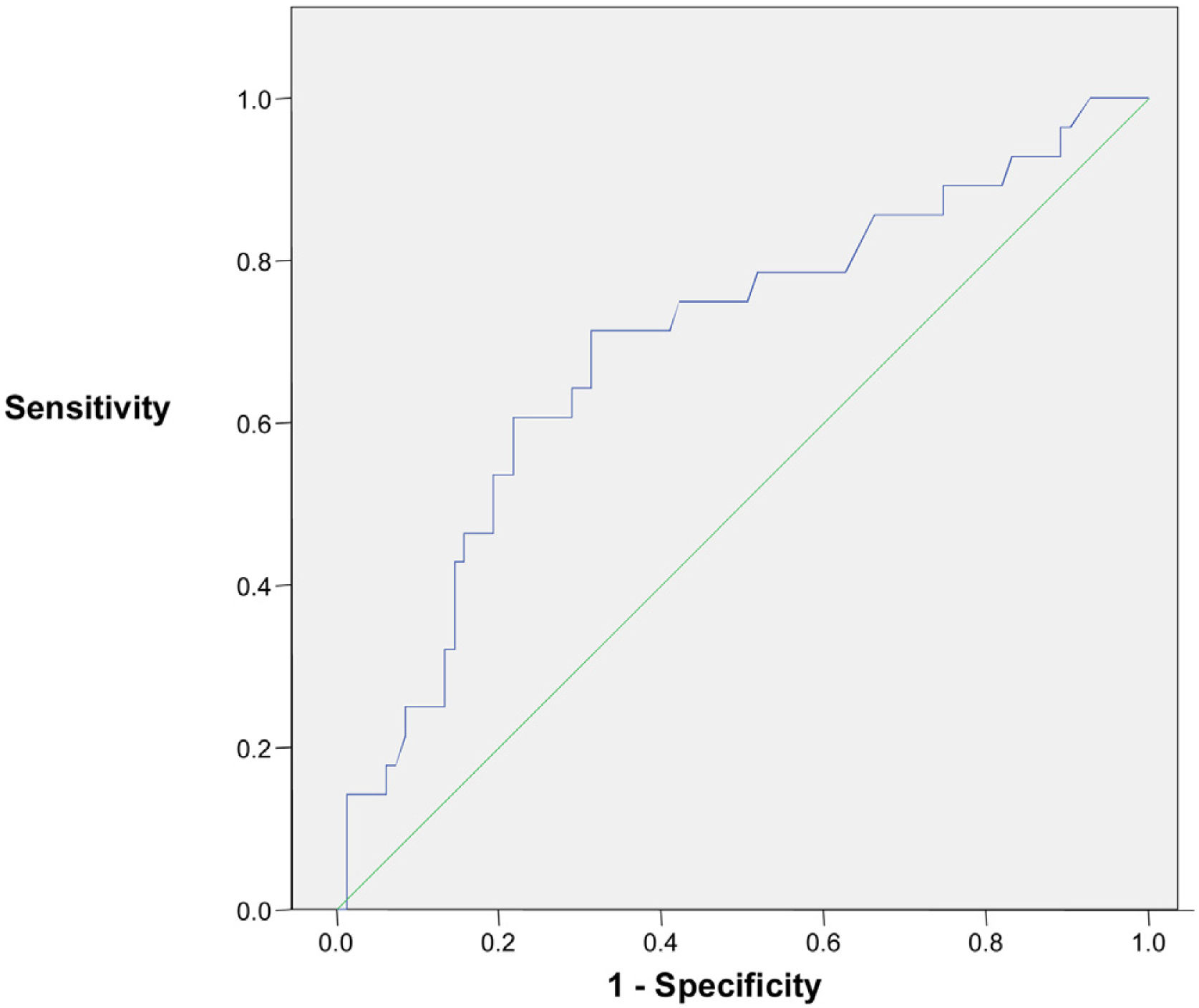
Only subjects with adequate further evaluation were included for a BD or MD as shown in the flow chart of Fig. 1. A total of 194 subjects were excluded for the analysis because they had no available thyroid US data. A further 67 patients with US examination were excluded because FNAC was inconclusive or was not performed despite the US pattern being different from the very low risk category. Therefore, patients with BD or MD consisted of 137 subjects, where 113 and 24 participants had focal and diffuse uptake on FDG PET-CT, respectively. The median values of SUVmax (6.77 [range: 2.1–66]) and nodule size (11 [range: 0–55]mm) were similar between focal and diffuse uptake lesions. The results from complementary studies carried out to assign a benign or malignant diagnosis in these patients are described in Table 2. A definitive benign or malignant diagnosis in these 137 patients was established according to histopathology in 40 cases who underwent thyroid surgery, after a conclusive FNAC in 61 cases who did not undergo surgery, and was based on a very low risk US category (as defined previously) in the remainder (36 cases) without any cytological or histopathological results (16 with no nodules found on US, 1 with an ATA benign US pattern and 19 with an ATA very low suspicion pattern). The prevalence of malignancy was significantly higher in the focal uptake subgroup (26.5%, 30 cases) than in the diffuse uptake subgroup (4%) where it was found in only one case of a 19mm classic papillary carcinoma with an intense lymphocytic infiltrate of the thyroid gland. Considering patients who underwent thyroid surgery or had a conclusive cytological result with FNAC, the malignancy rate rose to 33.3% among focal incidentalomas. The final diagnoses in 31 malignant diseases were the following: 21 papillary thyroid carcinomas (all but one with FDG focal uptake), three follicular thyroid carcinomas, one Hurthle cell carcinoma, two poorly differentiated thyroid carcinomas, two lymphomas and two metastases to the thyroid gland from tongue epidermoid carcinoma and colonic carcinoma. Comparisons between BD and MD in thyroid incidentally detected focal uptake are shown in Table 3. No differences were observed regarding age, nodule size and gender distribution. The median SUVmax was higher in the MD group (10.6 [3.1–51.2]) than in the BD group (5.7 [2.3–66], p<0.05), although there was a substantial overlap as shown in Fig. 2. When the ROC curve and SUVmax value for differentiating between MD and BD were used, the cut-off value for the SUVmax of 7.75 exhibited the largest area under the curve (0.698) with a sensitivity and specificity for malignancy of 71.4% and 68.7%, respectively. The ROC curve is depicted in Fig. 3. A Spearman r test revealed no correlation between the SUVmax and nodule diameter.
Complementary tests used to assign a benign or malignant diagnosis in 137 subjects.
| n | All (137) | Focal uptake (FU)113 | Diffuse uptake (DU)24 | p | |
|---|---|---|---|---|---|
| Histopathology | 40 | 40 (29.2%) | 37 (32.7%) | 3 (12.5%) | <0.05 |
| Conclusive FNAC* | 61 | 61 (44.5%) | 53 (46.9%) | 8 (33.3%) | <0.05 |
| Very low risk US** category | 36 | 17 normal US or ATA benign US pattern (12.4%) | 9 (8%) | 8 (33.3%) | <0.05 |
| 19 ATA very low suspicion US pattern (13.9%) | 14 (12.4%) | 5 (20.8%) | |||
| Malignant diagnosis | 137 | 31 (22.6%) | 30 (26.5%) | 1 (4%) | <0.05 |
In patients who did not undergo thyroid surgery, conclusive FNAC results fell into Bethesda Category II except in three cases belonging to Bethesda Category VI12 (one case of lymphoma, one case of poorly differentiated thyroid carcinoma and one case of papillary carcinoma).
In patients who did not undergo thyroid surgery and whose nodule was not submitted to FNAC, the very low risk US category included a normal US and ATA US benign and very low suspicion patterns.11
Comparisons between benign and malignant diagnosis in focal incidentalomas.
| Diagnosis | Benign | Malignant | p* |
|---|---|---|---|
| Female % | 69.8% | 53.3% | NS |
| Age: mean±SD | 65±11 | 63±13 | NS |
| Nodule size: median (range) | 11 (0–50) | 10 (6–55) | NS |
| SUVmax: median (range) | 5.7 (2.3–66) | 10.6 (3.1–51.2) | <0.05 |
NS: not significant.
We found a 1.8% prevalence of incidental thyroid uptakes in FDG PET-CT. Our rates were similar to those published in other studies.13 A few authors recommend using the term incidentaloma only when the FDG uptake is focal, but not when it is diffuse due to its association with benign processes.5 In our report, only one papillary thyroid carcinoma was described in 24 patients with a diffuse uptake who could be assigned a benign or malignant diagnosis. FDG diffuse uptake has been related to autoimmune lymphocytic infiltration as seen in chronic thyroiditis and Graves’ disease5 and to TSH receptor activation either by genetic mutations in autonomous nodules or antibodies in Graves’ disease.14 Although the lack of available data prevented us from analysing the proportion of patients with thyroid antibodies, thyroid dysfunction (mostly hypothyroidism) was found more frequently in the group with diffuse uptake (33.8%) than with focal uptake (21.6%), suggesting a greater number of autoimmune diseases among the former. Supporting this assumption, women comprised a higher percentage among FDG diffuse incidentalomas. The definition adopted for thyroid dysfunction in our study could have underestimated the differences because it did not include cases of pharmacologically normalised hormone levels.
In patients with further evaluation, establishing benign and malignant diagnosis, the malignancy rate of 26.5% in focal incidentalomas was comparable to that described in other studies15 but lower than that reported in two reviews (in about one-third of cases).4,8 Although the lower percentage found could partly be explained by the differences in subjects’ genetic background and the population submitted to PET-CT, the way we assigned the benign diagnosis could represent the main reason. Indeed, in most studies included in the above-mentioned reviews, the diagnosis was established with a conclusive cytological or histopathological result. When US patterns associated with a very low risk of malignancy11 are also considered for the benign diagnosis, the risk of malignancy can be similar to ours.16 Including, for a benign diagnosis, only cases with conclusive cytological or histopathological data, the rate of malignancy rose to 33.3%, resembling that reported by the meta-analysis. As FNAC indication usually depends on clinical suspicion and US, the pre-test probability of malignancy could be higher when a pathology report is required for benign diagnosis.4 In any case, such a high rate of malignancy suggests there is a need to develop specific PET-FDG thyroid incidentaloma management protocols.
Several hypotheses try to explain the high rates of malignancy in FDG-PET thyroid lesions. Firstly, most subjects submitted to FDG-PET studies are neoplastic patients in whom the probability of a second tumour may be higher and related to the abnormal genetic structure or previous treatment with radiotherapy.17 However, a similar prevalence of thyroid incidentalomas described in oncologic patients and in healthy subjects in PET scans limits the validity of this hypothesis.18 We did not observe differences in prevalence depending on the purpose of the PET-CT (patients with or without known malignancies). Secondly, the high rate of thyroid malignancy could be attributable to the PET-FDG principle itself as FDG uptake often reveals malignant cells with accelerated glucose consumption.19 Overexpression of the high-affinity glucose transporter GLUT-1 has been demonstrated in thyroid malignant neoplasms,20 mainly in aggressive differentiated carcinomas and anaplastic carcinomas.21 Although most malignant tumours in our study comprised papillary thyroid carcinomas (70%), histological distribution differed from those of palpable or US-identified carcinomas.22 Nearly a quarter corresponded to potentially aggressive tumours, including uncommon histological subtypes such as metastases from non-thyroid carcinomas already described among PET-CT incidentalomas.23 According to several authors,2,17 FDG thyroid focal uptake could be associated with potential aggressive malignant neoplasm as evidenced in one series,24 in which half of the thyroid carcinomas detected were aggressive malignancies (tall cell, insular or Hurtle cell tumours). Inversely and based on this assumption, most well-differentiated thyroid carcinomas that are usually considered with low aggressive potential and low glycolytic activity could be unidentified with a PET scan. Indeed, the absence of perithyroidal or lymphovascular invasion has been related to a negative uptake.25 Furthermore, well-differentiated papillary thyroid micro-carcinomas not evidenced by a preoperative PET are often reported on histological specimens after surgeries performed for unrelated indication.26 Also, several authors argue that the false-negative of PET-CT for microcarcinomas could be explained by the lower spatial resolution when tumour size is below 0.5 to 1cm due to the partial volume effect rather than its good cellular differentiation.27 In our study, as reported by other authors,28 there was no correlation between nodule size and glucose avidity evaluated with the SUVmax value.
Although focal thyroid uptakes on PET scans should contemplate the possibility of an aggressive tumour, most are not associated with malignant processes4 as observed in our study. Therefore, semi-quantitative parameters, such as SUVmax, have been considered to improve discrimination between malignant and benign lesions. In published studies, results on the prediction of malignancy by SUVmax are controversial. As in our study, about half of the studies observed significant differences in SUVmax values between malignant and benign lesions whereas half reported no differences.4,8 Comparing the studies is difficult because of the large heterogeneity regarding important factors, such as inclusion and exclusion criteria, selection bias, study size, healthy status (previously known malignancy or healthy volunteers) and diverse genetic or environmental backgrounds. Moreover, although SUVmax values are valid for each institution, no reliable comparison should be done from one institution to another. Actually, there are great variations regarding the method for calculation of the SUVmax concerning the level of fasting serum glucose, length of fasting period before the examination, volume and activity of injected FDG, time from the radiotracer examination and PET technology.
Despite higher SUVmax levels in malignant nodules, there was a pronounced overlap and ROC analysis did not allow identification of a safe threshold to distinguish benign from malignant lesions, as already reported.29 Using a high SUVmax value as the sole indicator of malignancy may be misleading because Hurthle and follicular adenomas have higher SUVmax compared with other benign conditions,5,27 overlapping with malignant neoplasms. Nowadays, the presence of any FDG uptake seems to be more important in terms of clinical decisions than the actual SUVmax level. Since SUVmax only represents a single pixel value within a tumour with potential heterogeneous features, other semi-quantitative parameters have been recently proposed to improve differentiation of benign from malignant lesions (as rates of SUVmax thyroid lesion to background reference tissues and volume-based functional parameters) with controversial preliminary results.30
Our study has several limitations. First, it is a retrospective study limiting the translation of results into clinical routine. Second, the majority of incidentalomas were not further evaluated with a possible incorrect estimation of malignancy rates as manifested in several reports with comparable retrospective designs.19 There are two possible reasons for the apparent low investigation rate in our study. Firstly, our study included patients from other institutions whose PET-CT was performed in our tertiary centre with no available information about further management. On the other hand, the patients’ clinical status related to the primary cancer extent could have prevented or postponed the thyroid evaluation. Anyway, the low percentage of patients with further evaluation might not be representative of the whole group.
ConclusionIn our series, 1.8% of thyroid incidentalomas were found in FDG PET-CT scans and 26.5% of focal uptakes on PET-CT were related to thyroid malignancy. Despite a higher SUVmax value among malignant incidentalomas, no reliable cut-off value was found that allowed discrimination between malignant and benign lesions. High malignancy rates of thyroid and the potential aggressiveness of revealed thyroid tumours by FDG PET-CT should lead to the implementation of specific practice protocols.
FundingThe present investigation has not received any financial support from public sector agencies, the commercial sector or non-profit entities.
Conflicts of interestThe authors declare that they have no conflicts of interest.