To provide recommendations based on evidence on the management of vitamin D deficiency in the general population.
ParticipantsMembers of the Bone Metabolism Working Group of the Spanish Society of Endocrinology.
MethodsRecommendations were formulated using the GRADE system (Grading of Recommendations, Assessment, Development, and Evaluation) to describe both the strength of recommendations and the quality of evidence. A systematic search was made in MEDLINE (Pubmed) using the term Vitamin D and the name of each issue. Papers in English and Spanish with publication date before 17 March 2016 were included. Recommendations were jointly discussed by the Working Group.
ConclusionsThis document summarizes the data about vitamin D deficiency in terms of prevalence, etiology, screening indications, adequate levels and effects of supplementation on bone and non-skeletal health outcomes.
Proporcionar recomendaciones basadas en la evidencia sobre el manejo del déficit de vitamina D en población general.
ParticipantesMiembros del Grupo de Trabajo de Osteoporosis y Metabolismo Mineral de la SEEN.
MétodosSe empleó el sistema Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) para establecer tanto la fuerza de las recomendaciones como el grado de evidencia. Se realizo¿ una bu¿squeda sistemática en Medline de la evidencia disponible para vitaminaD y el título de cada capítulo. Se revisaron arti¿culos escritos en inglés con fecha de inclusio¿n hasta 17 de marzo del 2016. Tras la formulacio¿n de las recomendaciones, estas se discutieron de manera conjunta en el grupo de trabajo.
ConclusionesEste documento resume los datos acerca del déficit de vitamina D en lo que respecta a su prevalencia, etiología, indicaciones de cribado, niveles adecuados y efectos de la suplementación a nivel óseo y extraóseo.
In recent years there has been a growing interest in vitamin D, not only because of its role in mineral and bone metabolism, but also because of its extraskeletal effects and the high prevalence of hypovitaminosis D. The main biochemical forms are vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol). The main source of the vitamin in humans is synthesis in the skin, followed by food1. Vitamin D3 or D2 is first hydroxylated at position 25 of the molecule by hepatic 25-hydroxylase to hydroxycholecalciferol (25OHD), also called calcifediol or calcidiol. Additional hydroxylation by 1α-hydroxylase at renal tubular cells leads to 1,25 dihydroxyvitamin D (1,25OH2D), the most hormonally active metabolite of this endocrine system.1 Its main role is maintenance of phosphorus and calcium metabolism through its actions at renal and intestinal level1. It also has other autocrine and paracrine functions throughout the body.2
Development of evidence-based recommendationsRecommendations were made based on the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system to establish the strength of recommendations and the level of evidence.3 A distinction is made between strong recommendations, expressed as “We recommend” and number 1, and weak recommendations, expressed as “We suggest” and number 2. The quality of evidence is expressed using symbols as follows: ⊕, very low evidence; ⊕⊕, low evidence; ⊕⊕⊕, moderate evidence; and ⊕⊕⊕, high evidence.3
Prevalence of vitamin D insufficiency/deficiency in SpainVitamin D insufficiency/deficiency represents an apparent worldwide epidemic. Thus, it has been reported that 88% of the population has plasma levels of 25OHD less than 30ng/mL, 37% levels less than 20ng/mL, and up to 7% mean levels under 10ng/mL.4
The situation in Spain is very similar. In subjects over 65 years of age, 25OHD levels less than 20ng/mL have been reported in 80%–100% of cases, and 40% of those under 65 years have deficient values.5–10 This apparent paradox of low vitamin D levels in Spain has been explained by low dietary provision, protection from sun exposure in the summer months, and by the fact that the greatest part of Spain is above the 35°N parallel, where the possibility of synthesizing vitamin D is low in winter and spring.
Definition of optimum vitamin D levelsRecommendation- -
We suggest that serum 25OHD levels ranging from 30 and 50ng/mL (75–125nmol/L) are maintained to achieve the health benefits provided by vitamin D (2⊕○○).
The definition of adequate 25OHD levels continues to be controversial. Thus, the values proposed by the Institute of Medicine (IOM) of the United States11 for the healthy general population are over 20ng/mL, while the International Osteoporosis Federation (IOF) suggests levels higher than 30ng/mL for patients.12 This recommendation is supported by the US Endocrine Society13 and by other scientific associations from many countries, including Spain.14 Serum 25OHD levels higher than 30ng/mL will ensure adequate bone health, but higher levels may possibly be required to achieve favorable outcomes in other health objectives.15–17 On the other hand, the maximum recommended serum 25OHD value is also controversial. There are data suggesting that levels less than 100ng/mL are not associated to toxic effects,18 and some authors have therefore proposed levels of 60–70ng/mL as recommended cut-off point.13 However, there is a current debate as to whether high 25OHD levels (>50–60ng/mL) could be associated to risk of death from cardiovascular or any other causes.19
In our view, until more solid evidence is available of the extraosseous benefits of higher vitamin D levels, serum 25OHD levels ranging from 30 and 50ng/mL (75–125nmol/L) ensure benefits for bone while maintaining an adequate safety profile and minimizing the inaccuracy seen with the different commercial tests.
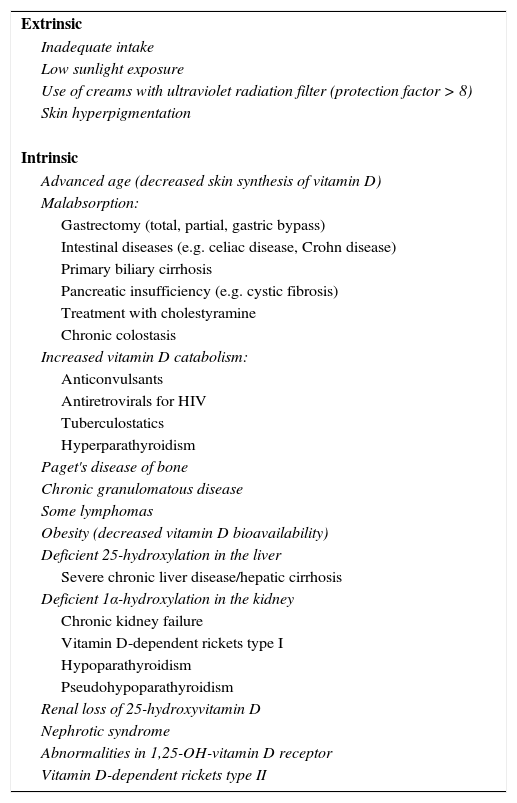
Causes of vitamin D deficiency/insufficiencyVitamin D deficiency may be of an extrinsic or intrinsic origin.13,20 Its main causes are described in Table 1.
Pathogenic mechanism and causes of vitamin D deficiency.
| Extrinsic |
| Inadequate intake |
| Low sunlight exposure |
| Use of creams with ultraviolet radiation filter (protection factor > 8) |
| Skin hyperpigmentation |
| Intrinsic |
| Advanced age (decreased skin synthesis of vitamin D) |
| Malabsorption: |
| Gastrectomy (total, partial, gastric bypass) |
| Intestinal diseases (e.g. celiac disease, Crohn disease) |
| Primary biliary cirrhosis |
| Pancreatic insufficiency (e.g. cystic fibrosis) |
| Treatment with cholestyramine |
| Chronic colostasis |
| Increased vitamin D catabolism: |
| Anticonvulsants |
| Antiretrovirals for HIV |
| Tuberculostatics |
| Hyperparathyroidism |
| Paget's disease of bone |
| Chronic granulomatous disease |
| Some lymphomas |
| Obesity (decreased vitamin D bioavailability) |
| Deficient 25-hydroxylation in the liver |
| Severe chronic liver disease/hepatic cirrhosis |
| Deficient 1α-hydroxylation in the kidney |
| Chronic kidney failure |
| Vitamin D-dependent rickets type I |
| Hypoparathyroidism |
| Pseudohypoparathyroidism |
| Renal loss of 25-hydroxyvitamin D |
| Nephrotic syndrome |
| Abnormalities in 1,25-OH-vitamin D receptor |
| Vitamin D-dependent rickets type II |
Adapted from Varsavsky et al.20.
- -
Screening for vitamin D deficiency is recommended in subjects with risk factors (1⊕⊕○○).
- -
Screening is not recommended in people with no risk factors (1⊕⊕○○).
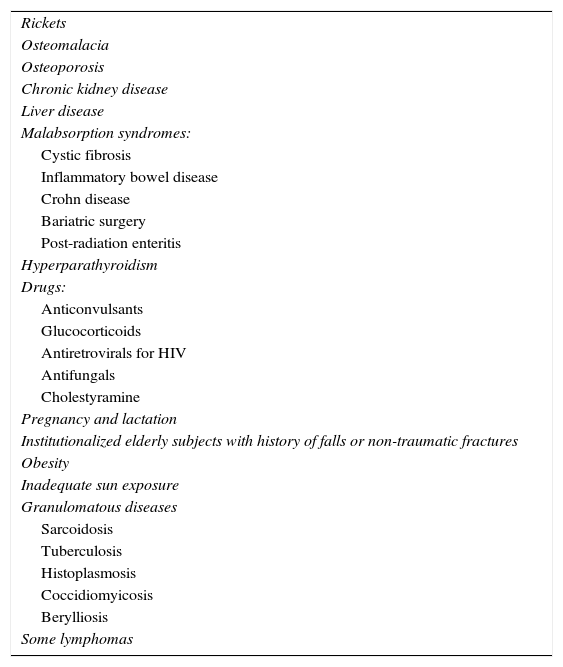
Universal screening for vitamin D deficiency is not recommended13 and should only be done in risk subjects or groups (Table 2).
Indications of screening for vitamin D deficiency.
| Rickets |
| Osteomalacia |
| Osteoporosis |
| Chronic kidney disease |
| Liver disease |
| Malabsorption syndromes: |
| Cystic fibrosis |
| Inflammatory bowel disease |
| Crohn disease |
| Bariatric surgery |
| Post-radiation enteritis |
| Hyperparathyroidism |
| Drugs: |
| Anticonvulsants |
| Glucocorticoids |
| Antiretrovirals for HIV |
| Antifungals |
| Cholestyramine |
| Pregnancy and lactation |
| Institutionalized elderly subjects with history of falls or non-traumatic fractures |
| Obesity |
| Inadequate sun exposure |
| Granulomatous diseases |
| Sarcoidosis |
| Tuberculosis |
| Histoplasmosis |
| Coccidiomyicosis |
| Berylliosis |
| Some lymphomas |
HIV: human immunodeficiency virus.
Adapted from Holick et al.13.
- -
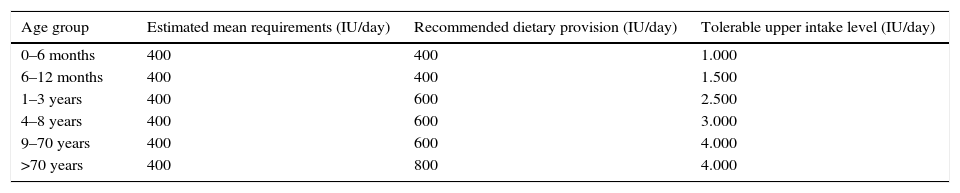
We suggest a daily intake of 600 international units (IU) of vitamin D in people aged less than 70 years old, and 800IU in those over 70 years of age (2⊕⊕○○).
Daily provision of vitamin D is currently controversial. The IOM, endocrinological societies, and the US Task Force do not agree on the daily amount required.11,13 The reason for this is that the recommendations of the IOM and US Task Force would be for the general healthy population, and those of medical societies for patients.11,13,21 The IOM committee recommends a daily amount of 600IU of vitamin D to meet the requirements of almost all the general population in the United States and Canada. The amount for people older than 70 years would be 800IU (Table 3).11
Recommended dietary intake of vitamin D.
| Age group | Estimated mean requirements (IU/day) | Recommended dietary provision (IU/day) | Tolerable upper intake level (IU/day) |
|---|---|---|---|
| 0–6 months | 400 | 400 | 1.000 |
| 6–12 months | 400 | 400 | 1.500 |
| 1–3 years | 400 | 600 | 2.500 |
| 4–8 years | 400 | 600 | 3.000 |
| 9–70 years | 400 | 600 | 4.000 |
| >70 years | 400 | 800 | 4.000 |
Adapted from the US Institute of Medicine.11
- -
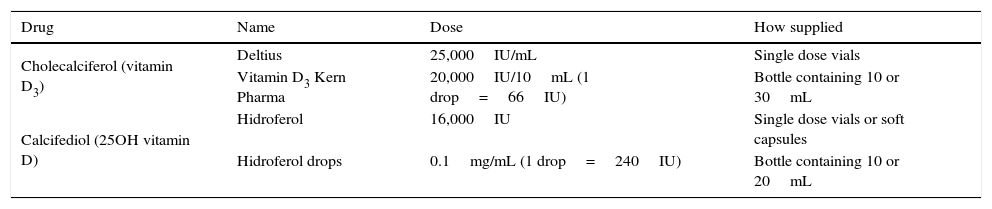
We recommend use of vitamin D3 (cholecalciferol) or 25OHD (calcifediol) to treat vitamin D deficiency (1⊕⊕⊕○).
- -
We suggest that the required dose of vitamin D is calculated depending on etiology and severity of the deficiency, and on the type of vitamin D that will be used for treatment (2⊕⊕○○).
- -
We suggest monitoring of serum 25OHD levels to assess response to treatment at 3–4 month intervals until the adequate 25OHD are reached, and every 6 months thereafter (2⊕⊕○○).
In Spain, vitamin D deficiency may be treated with preparations of vitamin D (cholecalciferol), 25OHD3 (calcifediol), 1,25OH2D3 (calcitriol), and 1αOHD3 (alfacalcidiol) (Table 4). 1,25OH2D3 and 1αOHD3 have a short half-life and greater risk of hypercalcemia, and are therefore not recommended for standard treatment of vitamin D deficiency. It should be reminded that vitamin D and 25OHD are not equipotent. 25OHD is more hydrophilic, has a shorter half-life and a faster start of action, and is 3–6 times more potent to increase serum 25OHD3 levels.22,23 The dose to be used will depend on the cause and severity of deficiency, and also on the vitamin D formulation used.
Commercial vitamin D preparations.
| Drug | Name | Dose | How supplied |
|---|---|---|---|
| Cholecalciferol (vitamin D3) | Deltius | 25,000IU/mL | Single dose vials |
| Vitamin D3 Kern Pharma | 20,000IU/10mL (1 drop=66IU) | Bottle containing 10 or 30mL | |
| Calcifediol (25OH vitamin D) | Hidroferol | 16,000IU | Single dose vials or soft capsules |
| Hidroferol drops | 0.1mg/mL (1 drop=240IU) | Bottle containing 10 or 20mL |
In patients with normal absorption capacity, it has been seen that each 100IU of vitamin D increase serum 25OHD levels by 0.7–1ng/mL. The biological potency of vitamin D is established so that 40IU are equivalent to 1μg of colecalciferol.24 Multiple dosage schemes have been tested, and similar results have been reported with daily, weekly, monthly, bimonthly, and even quarterly schemes.25 However, annual administration of high doses (300,000IU) should be avoided because of the increased risk of fall and fracture reported.26,27
Treatment should be monitored at 3–4 month intervals, and once the desired serum 25OHD levels are reached, maintenance doses should be given to prevent a new decrease in 25OHD levels.13
Bone effects of vitamin D supplementation in the general populationRecommendation- -
We recommend that people over 65 years of age and institutionalized are given 800–1000IU/day of vitamin D to improve bone health and decrease the risk of non-vertebral fracture (1⊕⊕⊕⊕).
- -
We suggest that adults over 50 years of age are given at least 800IU/day of vitamin D in addition to an adequate calcium (1000–1200mg/day) to improve bone health and decrease risk of fracture (2⊕⊕⊕⊕).
- -
There is no evidence to recommend routine supplementation in all adults under 50 years of age to improve bone health (2⊕⊕⊕○).
In adults under 50 years of age, no adequate evidence is available showing the benefit of vitamin D supplementation on risk of fracture.
Studies analyzing the relationship between vitamin D supplementation and bone mineral density (BMD) in people over 50 years of age were relatively small, used doses ≤400IU/day, and did not find a significant effect, but showed a preventive effect on the spine and hip when calcium was coadministered.28 A recent meta-analysis of randomized clinical trials with vitamin D supplementation in non-osteoporotic populations showed no changes of BMD in any tested site, except for a minimum increase in the femoral neck, which was considered by the authors an incidental finding.29
As regards fractures, meta-analyses of controlled trials published in the past 10 years showed that use of vitamin D alone, as compared to placebo, did not decrease the risk of fracture,30–32 except for the Bischoff-Ferrari meta-analysis, where a subgroup analysis showed that high vitamin D doses (>800IU) achieved prevention of non-vertebral fractures irrespective of calcium supplementation especially in elderly subjects, and particularly in those institutionalized.33,34 Variable results have been reported for the combination of calcium and vitamin D, but there was a trend to a significant decrease in hip, non-vertebral, and all fractures with doses higher than 400IU of vitamin D daily and 500–1200mg of calcium.35
Effects of treatment with vitamin D supplements on incidence of fallsRecommendation- -
We recommend measurement of serum 25OHD levels in subjects with muscle weakness and falls (1⊕⊕○○).
- -
We recommend that patients with vitamin D deficiency and high risk of fall are treated with supplements (1⊕⊕○○).
Vitamin D has different effects on muscle. 1,25OH2D, by binding to the vitamin D receptor (VDR), regulates gene transcription and promotes de novo synthesis of proteins involved in calcium and phosphorus transport and in muscle fiber proliferation and differentiation.1,2 In addition, it also appears to have non-genomic effects through a receptor different from vitamin D located at the cell membrane which would promote the active calcium transport into the sarcoplasmic reticulum required for adequate muscle contraction.1,2,36
Vitamin D deficiency is associated to muscle weakness (particularly proximal). In patients with this deficiency, muscle biopsy shows selective loss and atrophy of type II muscle fibers, the main ones involved in fall prevention.36 This observation may explain the increased risk of falls in people with vitamin D deficiency.36 Data from observational studies suggest that 25OHD levels less than 20ng/mL are related to poorer lower limb muscle function in elderly patients.2 Different clinical trials have found that supplementation with vitamin D in elderly patients improves strength, muscle function, and balance.37
As regards the protective effect of vitamin D supplementation on fall rate, results appear to depend on prior serum levels, subject age, and their living environment. In a review of 25 RCTs published in 2011, supplementation with vitamin D with or without calcium decreased 14% the overall risk of fall and up to 47% in patients with prior deficiency.38 In turn, the US Task Force recently concluded that vitamin D supplementation decreased the risk of fall by 11%.39 Serum 25OHD levels higher than 24ng/mL appear to have greater protective effect.40 On the other hand, the last Cochrane review and a sequential meta-analysis of clinical trials showed no benefit of vitamin D supplementation on risk of fall in the general population.41,42 However, there is a benefit in elderly subjects with high risk of falls, such as those who are institutionalized and those living in the community and have lower vitamin D levels before treatment.41–46
Extraosseous benefits of treatment with vitamin D supplementsRecommendation- -
There is no adequate evidence to support use of vitamin D supplements to obtain extraosseous benefits (2⊕⊕○○).
- -
We do not recommend supplementation with vitamin D to decrease the incidence of cancer in the general population (1⊕⊕⊕○).
Vitamin D supplements have not shown benefits on cardiovascular morbidity and mortality.47–51
In pregnant women, supplements non-significantly decrease the risk of preeclampsia (relative risk [RR] 0.52; 95% confidence interval [CI]: 0.25–1.05), with no effect on risk of gestational diabetes. In studies with small patient samples, supplements have been related to a lower risk of preterm delivery (RR 0.36; 95% CI: 0.14–0.93) and low birthweight (RR 0.40; 95% CI: 0.24–0.67).52
A great controversy exists on the effect of vitamin D supplementation and incidence of cancer. In a randomized study, Lappe et al.53 showed a reduced incidence of cancer (RR 0.402; 95% CI: 0.20–0.82; p=0.01) in women over 55 years of age who received daily supplements of calcium and vitamin D3. Treatment with calcitriol or alfacalcidiol for three years after kidney transplant was associated to a lower risk of tumors (HR 0.25; 95% CI: 0.07–0.82).54 In the study Women's Health Initiative, however, daily treatment with 1g of calcium and 400IU of D3 for 7 years had no influence on incidence of colorectal cancer and invasive breast cancer.55 In addition, a systematic review of 18 randomized studies found no association between vitamin D supplementation for up to 7 years and incidence of cancer.56
A meta-analysis of 56 randomized studies showed a slight reduction in total mortality (RR 0.94; 95% CI: 0.91–0.98) and cancer mortality (RR 0.88; 95% CI: 0.78–0.98) in patients treated with vitamin D3 after 4.4 years of follow-up; the effect was only seen when the vitamin was administered daily associated to calcium at doses >800IU/day, and in patients with vitamin D insufficiency.57
Note of authorsThis article is the executive summary of the complete document, which may be consulted at the web site of the Spanish Society of Endocrinology and Nutrition.58
FundingNo funding was received to conduct this study.
Conflicts of interestThe authors state that they have no conflicts of interest in relation to preparation of this article.
Please cite this article as: Varsavsky M, Rozas Moreno P, Becerra Fernández A, Luque Fernández I, Quesada Gómez JM, Ávila Rubio V, et al. Recomendaciones de vitamina D para la población general. Endocrinol Diabetes Nutr. 2017;64:7–14.