The current training program for resident physicians in endocrinology and nutrition (EN) organizes their medical learning. Program evaluation by physicians was assessed using a survey.
Material and methodThe survey asked about demographic variables, EN training methods, working time and center, and opinion on training program contents.
ResultsFifty-one members of Sociedad Castellano-Manchega de Endocrinología, Nutrición y Diabetes, and Sociedad Andaluza de Endocrinología y Nutrición completed the survey. Forty-percent of them disagreed with the compulsory nature of internal medicine, cardiology, nephrology and, especially, neurology rotations (60%); a majority (>50%) were against several recommended rotations included in the program. The fourth year of residence was considered by 37.8% of respondents as the optimum time for outpatient and inpatient control and monitoring without direct supervision. The recommended monthly number of on-call duties was 3.8±1.2. We detected a positive opinion about extension of residence duration to 4.4±0.5 years. Doctoral thesis development during the residence period was not considered convenient by 66.7% of physicians. Finally, 97.8% of resident physicians would recommend residency in EN to other colleagues.
ConclusionsEndocrinologists surveyed disagreed with different training program aspects such as the rotation system, skill acquisition timing, and on-call duties. Therefore, an adaptation of the current training program in EN would be required.
El programa de formación MIR regula el aprendizaje de los médicos residentes en Endocrinología y Nutrición (EYN). Evaluamos la valoración que realizan los facultativos en EYN sobre dicho programa mediante una encuesta.
Material y métodoLa encuesta incluía: variables demográficas, vía y hospital de formación, tiempo trabajado, centro de trabajo actual, y la opinión sobre el contenido del programa de formación: sistema de rotaciones, competencias, guardias, y otras preguntas.
ResultadosSe encuestó a 51 endocrinólogos asistentes a las Jornadas de Casos Clínicos de las Sociedades Castellano-Manchega y Andaluza de EYN (SCAMEND, SAEN). Los entrevistados mostraron su desacuerdo con las rotaciones obligatorias durante el primer año de residencia en Neurología y Protección Radiológica, y con las recomendables por Digestivo, Neumología, Hematología y Unidad de Cuidados Intensivos. Sin embargo, creyeron convenientes las obligatorias a partir del segundo año de residencia dentro del propio Servicio de EYN (Hospital de Día, Consultas Externas y Nutrición). El 37,8% de los encuestados consideraron el cuarto año de residencia como el momento en que el residente puede realizar sin tutorización el control y seguimiento de pacientes ambulatorios y hospitalizados (nivel 1 de responsabilidad). La mayoría de los encuestados consideraron que el residente debe realizar las guardias (3,8±1,2/mes) en el primer año en urgencias, en planta durante el resto de la residencia y no por los servicios de rotación. Detectamos una opinión positiva hacia la prolongación de la duración de la residencia hasta 4,4±0,5 años. El 66,7% no consideró necesario la realización de la tesis doctoral durante la residencia. Finalmente, el 97,8% recomendaría la residencia en EYN a algún médico que haya aprobado el MIR.
ConclusionesLos facultativos en EYN mostraron cierto desacuerdo con el programa de formación MIR en aspectos del sistema de rotaciones, cronología de la adquisición de competencias y módulos de guardias. Por lo tanto, resultaría necesaria una adaptación del actual programa de formación MIR de EYN.
The current training program for resident physicians (RPs) in endocrinology and nutrition (E%N) was prepared by the National E&N Committee, verified by the National Board of Medical Specialties and the Committee of Human Resources of the National Health System, endorsed by the Ministry of Education and Science, and finally approved by the Ministry of Health and Consumer Affairs in 2006.1 This system has been shown to be an excellent way of improving the clinical skills of specialist physicians2 and details the objectives, skills competence, responsibility levels, and clinical rotations of RPs in E&N.
Prior data reported in 2000 and 2006 by our working group showed the positive rating by RPs of their theoretical training and degree of supervision, with a progressive improvement in the level of achievement of the objectives established in the training program.3,4 In an article in this same journal we report the results of the latest survey of E&N residents, showing an improved perception by residents of their training. However, no information was available about the opinion of E&N specialists on the different aspects of the training program in their specialty. This study analyzes the assessment of objectives, skills, responsibilities, clinical rotations, on-call duties, and other aspects of the official training program in E&N made by already trained endocrinologists currently practicing their specialty.
Material and methodThe survey was completed by participants to case report sessions held by Sociedad Castellano-Manchega de Endocrinología, Nutrición y Diabetes (SCAMEND) and Sociedad Andaluza de Endocrinología y Nutrición (SAEN) in 2010 in Alcázar de San Juan and Antequera respectively.
The four-page questionnaire, consisting of 60 questions, collected personal data such as sex, type of E&N training (as RP or other models, specifying if applicable), location and number of beds of hospital of residency (< 500, 500-1,000, > 1,000 beds), time worked since end of residency (in years), and type of hospital where physicians were practicing (general, regional, others, specifying if applicable). 21 questions were about the clinical rotation system (agreement or not with the clinical rotations in the RP training program), and 14 were aimed at determining the year of residency when RPs were able to discharge, with no need for direct tutoring (responsibility level 1), the various roles established in the skills acquisition timing of the training program. Six questions about on-call duties asked physicians whether or not they thought it advisable that first-year residents should perform on-call duties in the emergency room, in the department itself, and in the departments they were in during the different rotation periods. The questionnaire also asked if it would be advisable for residents in their last three years to perform on-call duties in the emergency room and in hospital wards. All of these questions had to be answered ‘yes’ or ‘no’. The last question in this section referred to the number of monthly on-call duties they thought convenient for residents. The final 13 questions of the survey referred to other aspects related to the specialty, such as the journals and books that residents should regularly use and be considered for reference purposes respectively (free choice of answer), attendance of courses and meetings essential for training (free choice of answer), and finally, other subjects of interest such as whether or not they thought an exam at the end of the residency period was convenient or a regular evaluation system of centers accredited for E&N training was necessary, and whether or not they would recommend future RPs to choose E&N as a specialty.
SPSS 11.5 software (in the Spanish version) was used for statistical analysis. Quantitative variables are given as mean ± standard deviation, and qualitative variables as absolute values and percentages.
ResultsThe survey was completed by 51 (63%) endocrinologists attending the case report sessions of SCAMEND (70%) and SAEN (30%).
Survey sample characteristicsOur sample consisted of male (55.5%) and female (44.4%) endocrinologists, most of them trained as RPs (94%), who had worked as associate physicians (90.2%) or heads of department (9.8%) for 12.0 ± 9.8 years at general (82.2%) and regional (17.8%) hospitals of the Castile La Mancha Health Service (SESCAM) and the Andalusia Health Service (SAS). Of the physicians surveyed, 43.3% had completed residency less than 5 years previously. They had mainly been trained at hospitals with more than 500 beds (85%) from the Madrid (52%), Andalusia (40%), Asturias (2%), Castile-Leon (2%), Catalonia (2%), and Navarre (2%) autonomous regions.
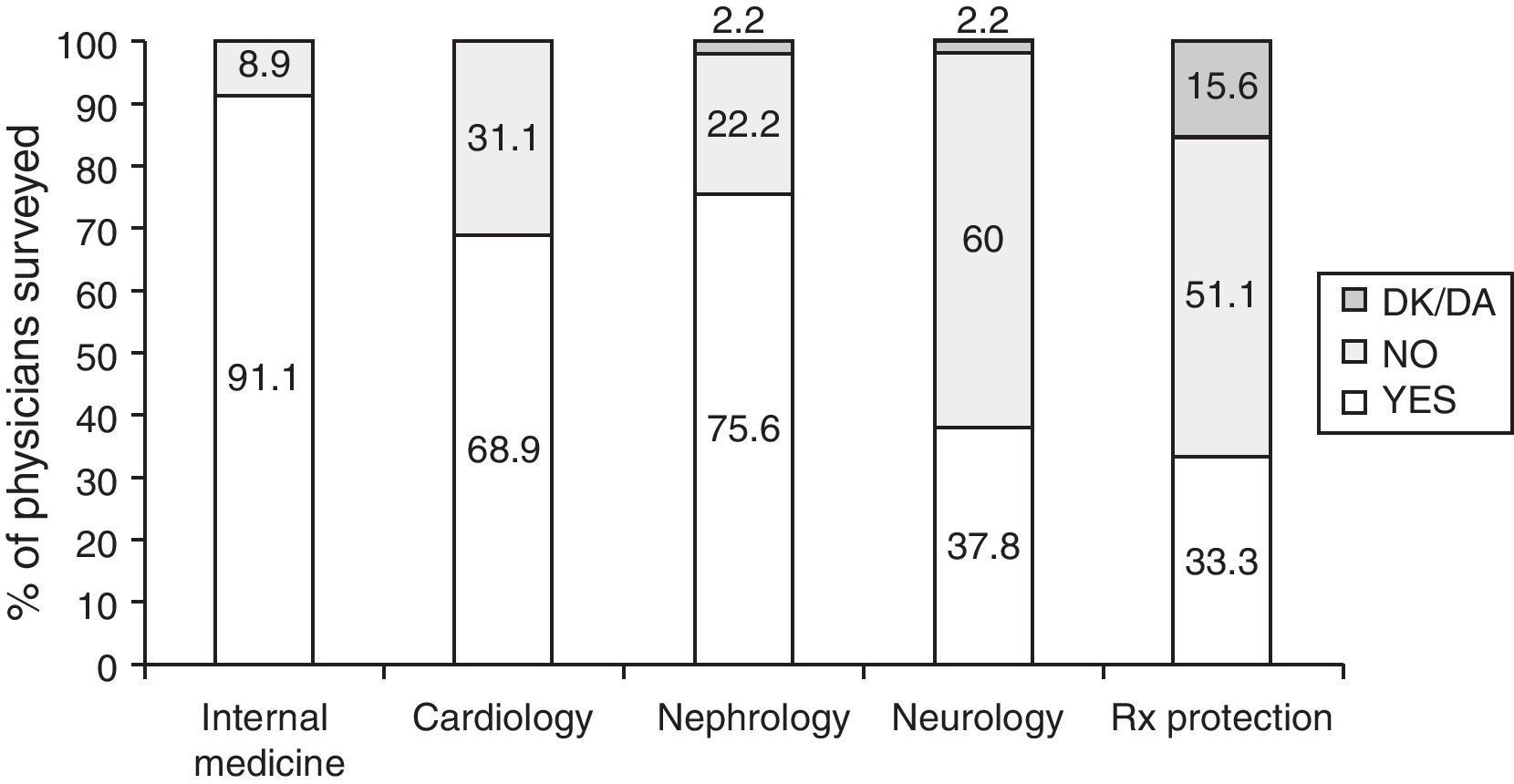
Rotation systemMost physicians surveyed agreed that clinical rotations at the departments of internal medicine (91.1%), cardiology (68.9%), and nephrology (75.6%) should be included in the first year of residency, but 60% were opposed to clinical rotation in the neurology department. Seventy-six percent of endocrinologists considered performance of these clinical training rotations during the first year adequate. However, 40% thought that they should not be mandatory, as recommended in the training program.
With regard to mandatory rotation for training in radiological protection for 7-12h, 51% disagreed with its mandatory nature, but 53% considered their duration adequate. Non-responders to both questions represented 15.6% and 29% of the sample respectively. Fig. 1 details the results found for mandatory training rotations.
The questionnaire included a question about the convenience of a compulsory training rotation in primary care, which was considered inadequate by 60% of the surveyed sample. In any case, 45.5% thought that is should occur during the third year of residency.
As regards compulsory training rotations from the second year of residency within the E&N department itself, there was agreement with the rotations and their duration at the ward and day hospital (91.1%), outpatient clinics (100%), and nutrition (100%). Other training rotations recommended by the RP training program that were considered adequate included those planned in gynecology (57.8%, minimal duration of 2 months) and pediatric endocrinology (75.6%, minimal duration of 3 months).
There was disagreement about the recommended training rotations during the first year of residency, as 66.7%, 91.1%, 91.1%, and 57.8% of physicians did not consider such rotations advisable in the gastroenterology, pneumology, and hemato-oncology departments and the intensive care unit (ICU) respectively. These training rotations are decided at each center by the department heads (there were 5 in the surveyed sample), who did not recommend training rotations at gastroenterology (66.7%), pneumology (100%), and hemato-oncology (66.7%). Clinical training rotation at ICU was, however, recommended by 66.7% of heads of department.
Other optional training rotations from the second year of residency included in the program were recommended by endocrinologists as follows: regional hospital, 13.3%; hormone laboratory, 73.3%; andrology, 31.1%; and others, 26.7%.
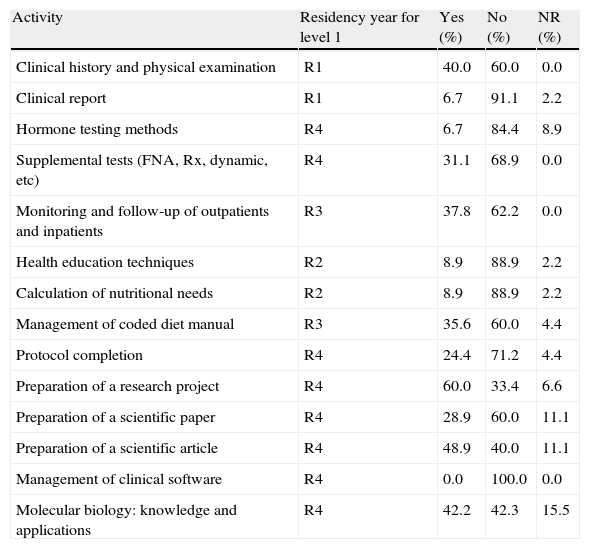
SkillsThe current training program determines the map of skills and skills acquisition responsibility levels by year of residency. Level 1 refers to the performance of certain activities by residents without the need for direct tutoring, and level 3 refers to activities performed by healthcare staff from the center observed or assisted by residents. No agreement was found between the training program and the opinion of most (> 50%) physicians surveyed in 11 of the 14 elements of the skill acquisition timetable considered in our survey (Table 1). In the opinion of 37.8% of the surveyed sample, RPs should not perform monitoring and follow-up of outpatients or inpatients without direct supervision until the fourth year of residency.
Percentage of agreement between skills level 1 (without direct tutoring) and opinion of physicians surveyed.
| Activity | Residency year for level 1 | Yes (%) | No (%) | NR (%) |
| Clinical history and physical examination | R1 | 40.0 | 60.0 | 0.0 |
| Clinical report | R1 | 6.7 | 91.1 | 2.2 |
| Hormone testing methods | R4 | 6.7 | 84.4 | 8.9 |
| Supplemental tests (FNA, Rx, dynamic, etc) | R4 | 31.1 | 68.9 | 0.0 |
| Monitoring and follow-up of outpatients and inpatients | R3 | 37.8 | 62.2 | 0.0 |
| Health education techniques | R2 | 8.9 | 88.9 | 2.2 |
| Calculation of nutritional needs | R2 | 8.9 | 88.9 | 2.2 |
| Management of coded diet manual | R3 | 35.6 | 60.0 | 4.4 |
| Protocol completion | R4 | 24.4 | 71.2 | 4.4 |
| Preparation of a research project | R4 | 60.0 | 33.4 | 6.6 |
| Preparation of a scientific paper | R4 | 28.9 | 60.0 | 11.1 |
| Preparation of a scientific article | R4 | 48.9 | 40.0 | 11.1 |
| Management of clinical software | R4 | 0.0 | 100.0 | 0.0 |
| Molecular biology: knowledge and applications | R4 | 42.2 | 42.3 | 15.5 |
NR, non-responders; FNA, fine needle aspiration; Rx, radiology.
According to the training program, residents should perform 4 to 6 on-call duties per month in the emergency room and ward, depending on the needs of the center. 28.8% of physicians considered it advisable for first year residents to perform on-call duties at E&N, while 93.2% and 33.3% respectively thought that they should do on-call duties in the emergency room and in the departments where they were currently rotating. However, 46.7% and 91.1% thought it advisable for second, third, and fourth year residents to perform on-call duties in the emergency room and ward respectively. On the other hand, physicians tended to think that the number of on-call duties performed by residents should be reduced to 3.8±1.2 per month.
Other questions of interestWith regard to scientific literature, endocrinologists cited the following journals as essential for resident training: Endocrinología y Nutrición (33%), Journal of Clinical Endocrinology and Metabolism (27%), and New England Journal of Medicine (13%). The reference books recommended included Williams Textbook of Endocrinology (61%) and Manual del residente en EYN (13%), among other texts.
Seventy-one percent of the surveyed physicians considered it essential to attend the annual meeting of the Sociedad Española de Endocrinología y Nutrición (SEEN) and 9% the annual meeting of the Sociedad Española de Diabetes (SED) As regards the training courses organized by SEEN and SED, they were recommended by 51% and 16% of physicians respectively.
Studying for a doctorate during residency was considered appropriate by 55.6% of surveyed physicians, but 66.7% thought that RPs did not need to do their doctoral thesis before completing their training period.
Sixty-two percent of the surveyed physicians were opposed to a final residency exam. Thus, 89% thought that residents are adequately trained to work when they have completed their residency. There was also a tendency to think that residency time should be prolonged to 4.4±0.5 years, and 91.1% of the physicians surveyed thought that nutrition should continue to be part of the program and the specialty of E&N. Finally, 97.8% of associate physicians would recommend residency in E&N to a physician who had passed the RP exam this year.
DiscussionThis paper is the first to report the views of specialist physicians in E&N on multiple aspects of the training program for RPs in this specialty, as collected through an anonymous survey.
The questionnaire was completed by 51 (63%) of the physicians attending the case report sessions of SCAMEND and SAEN, and all of them were members of at least one of the two associations. These endocrinologists were members of the endocrinology staffs of the different healthcare centers of SESCAM and SAS, training E&N residents. This, combined with the fact that most of them (94%) had undergone training as RPs, 43.3% within the previous 5 years, suggests that they were aware of the basic essentials of an RP training program. Our data could therefore be extrapolated to all E&N professionals who were informed about the training program. We think that endocrinologists with the best knowledge of the current training program for RPs should be those who are resident tutors themselves. Unfortunately, this information was not collected, and cannot therefore be analyzed. However, as in other studies based on surveys to endocrinologists,5–8 we think that the current survey does not accurately reflect the views of all Spanish endocrinologists, but only those of survey responders. On the other hand, while the vast majority of data collected cannot be compared to prior data or opinions, they may provide an up-to-date overview of the thinking of all E&N specialists.
Analysis of the answers to questions about the training rotation system revealed that a majority did not agree with compulsory clinical rotations at neurology and radiological protection or with a potential compulsory rotation at primary care during the first year of residency. In our view, the objection to clinical rotation at radiological protection may partly be due to a lack of information; in fact, the highest rates of non-responders (15.6% and 29% respectively) of the whole survey were found in the two questions referring to this rotation, which was first included in the 2006 RP training program.1 A similar thing may occur with the primary care rotation proposed by the Ministry of Health and Consumer Affairs but not yet included in the training scheme. Similarly, most physicians surveyed did not consider the recommended clinical rotations at gastroenterology, pneumology, hemato-oncology, ICU, regional hospital, or andrology to be necessary either. The non-compulsory nature of these rotations and the fact that the training program is only used as guidance would explain why, despite these rotations being recommended, they were not supported by most of the physicians surveyed. On the other hand, since categorical answers (‘agree’ or ‘disagree’) were collected to these questions, information was not obtained concerning the degree of acceptance. This could have been avoided by using graded answers (‘mostly agree’, ‘agree’, ‘disagree’, ‘mostly disagree’), but when the survey was prepared, we finally chose a simpler answer system to promote the acceptance and adherence of the survey sample.
Special mention should be made of the majority opinion of the physicians surveyed, previously reported in other countries,9,10 concerning compulsory clinical rotations in the second year of residency in the E&N department itself (day hospital, outpatient clinics, and nutrition), which were considered as essential for the training of future specialists.
As regards skill acquisition timing, disagreement was found between the training program and the views of endocrinologists, with a trend among the latter towards reducing the levels of responsibility in most knowledge areas and skills.
However, 89% of endocrinologists thought that at the end of their residency period, RPs were adequately trained to care for patients, a view which agrees with the positive self-image of residents themselves reported in another article published by us (97.5% felt that they were qualified to work at the end of residency).
As regards on-call duties, disagreement was found between recommendations given in the training program (4 to 6 on-call duties monthly), the view of endocrinologists (3.8 ± 1.2 on-call duties/month), and the actual mean number of more than 5 on-call duties per month currently performed by RPs during the 4 years of residency. It would be convenient if at least part of those on-call duties could be performed at a diabetes day hospital. Specification of all of these conditions in the official training program would help them defend themselves before the teaching committees of each center.4
Emphasis should again be made here on how little research activity is being undertaken by E&N residents, and in another article in this same journal we report on a survey that revealed that 27.5% of residents had not published and not one of them had completed his or her doctoral thesis. The views of endocrinologists, who think that there is no need to follow doctorate courses (44.4%) or do a doctoral thesis (66.7%) during residency, will do nothing to improve this situation.
This survey also reflects, for the first time, the interest of physicians in the training of new physicians in E&N, as virtually all of them (97.8%) recommended our specialty to future residents.
We may conclude by saying that the lack of agreement about various aspects of the current training system makes it necessary to open a debate about the convenience of maintaining some clinical training rotations, incorporating training rotations not currently included, redefining skills timing, establishing new possibilities for on-call duties, and implementing new mechanisms to improve the scientific and research activities of residents.
Training program updates will continue to be required, and resident themselves, endocrinologists, and tutors in charge of training will need to develop mechanisms for information and opinion feedback.
Conflicts of interestThe authors state that they have no conflicts of interest.
We thank all endocrinologists from SCAMEND and SAEN for devoting part of their time to complete the surveys, and the organizing committees of the case report sessions in Alcázar de San Juan and Antequera for their help.
Please, cite this article as: Moreno-Fernández J, et al. Valoración del programa de formación de médicos residentes en Endocrinología y Nutrición por facultativos: resultados de una encuesta. Endocrinol Nutr. 2011;58:510–5.