Oncocytic neoplasms or oncocytomas usually arise in organs such as the kidney, thyroid, parathyroid, salivary, or pituitary glands. Adrenal cortex oncocytomas are extremely rare and are usually discovered as incidental findings. The case of a female patient with Cushing's syndrome caused by a benign adrenal oncocytoma is reported.
The patient was a 61-year-old woman referred to the endocrinology outpatient clinic for obesity in February 2014. When questioned, she reported a tendency to overweight since she was 30 years old, but this had exacerbated in the last year, in which her weight had increased by 10kg for no apparent reason. The patient had also had HBP for the previous 8 years, and was being treated with five antihypertensive drugs (ARB, beta-blocker, alpha-blocker, thiazide, and calcium channel blocker).
Her personal history included menopause at 50 years of age; she had no other remarkable personal or family history.
Physical examination findings included: 96.4kg of weight with BMI of 38.6kg/m2, BP of 130/90mmHg, facial plethora with slight “full moon” appearance, facial hirsutism, atrophic skin, increased posterior cervical and supraclavicular fat, increased abdominal circumference with fat redistribution, and muscle atrophy in her lower limbs.
The results of the laboratory tests initially requested included: hemoglobin 16.7g/dL and hematocrit 51.8% in a complete blood count, which was otherwise normal. The chemistry results were normal except for a glucose level of 107mg/dL. Oral glucose (75g) tolerance test: 106–280mg/dL; plasma cortisol 15.9mcg/dL after 1mg of dexamethasone, and urinary free cortisol 233.9mcg/24h (No.=0–100).
Cushing's syndrome was suspected, and the following measurements were performed, some of them repeated on two consecutive days: plasma cortisol at 8h: 14.1 and 13.9mcg/dL, plasma cortisol at 23h: 12.3 and 10.9mcg/dL, ACTH: <5 and <5pg/mL. Weak suppression with dexamethasone (0.5mg/6h 2 days): plasma cortisol 13.7mcg/dL, urinary free cortisol 160mcg/24h.
Catecholamine and metanephrine levels in 24h urine were normal, as were all other androgen levels measured (testosterone 0.27ng/mL, androstenedione 2.04ng/mL, DHEAS 1.3mcg/mL). Gonadotropin and estradiol levels were FSH 42.80mIU/mL, LH 7.21mIU/mL, and estradiol 13pg/mL.
Abdominal CT with contrast revealed an oval lesion, well defined and homogeneous, dependent on the left adrenal gland, approximately 33mm×30mm in size. Hounsfield units (HU) were 23HU without contrast; after intravenous contrast injection, 102HU at 65s and 40HU at 10min. This showed the lesion to be benign because washout was greater than 50%, despite showing low lipid content behavior and being denser than normal.
The patient underwent a left laparoscopic adrenalectomy. Intravenous hydrocortisone 100mg was administered before surgery, which was uneventful. The postoperative course was favorable, with hospital discharge 6 days after surgery. Three months after surgery. BP values were normal without antihypertensive treatment, the patient had lost 4kg of weight, and her facial plethora had clearly improved. At 11 months, the patient continues on replacement therapy with hydrocortisone 30mg/day, because in the most recent laboratory tests, her cortisol level after ACTH had increased from 3.4 to 7.6mcg/dL.
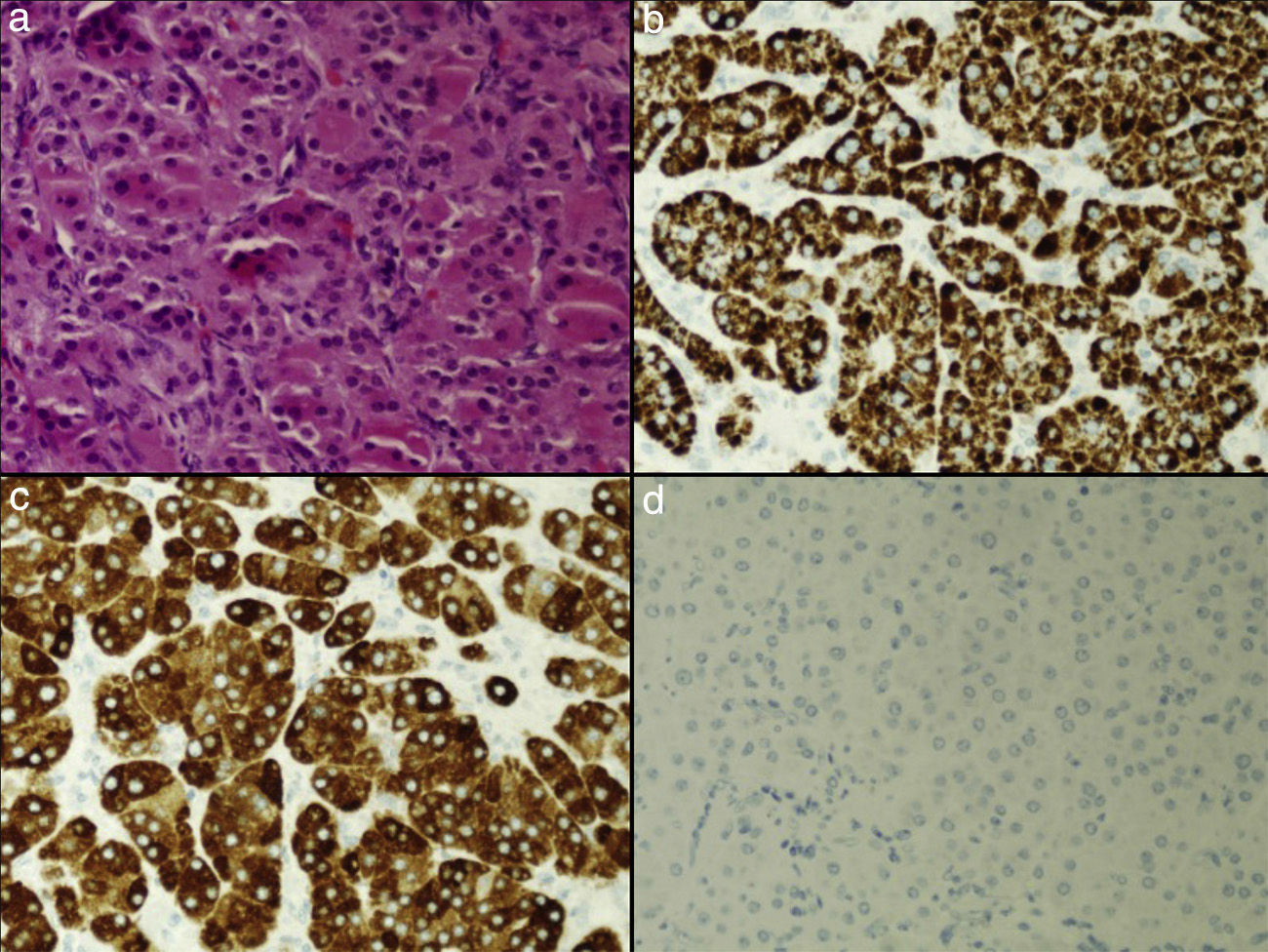
Gross pathological examination of the adrenalectomy specimen showed a round, well-circumscribed, encapsulated tumor that measured 3cm in its longer axis and was mahogany brown in color upon sectioning. Microscopic examination showed a tumor population with a solid growth pattern; more than 50% of tumor cells had eosinophilic and granular cytoplasm. These oncocytic cells had nuclei with mild pleomorphism; no mitotic figures were found. Immunohistochemistry tests were positive for vimentin, alpha-inhibin, and melan-A, weakly positive for calretinin, and focally positive for synaptophysin, with no staining for chromogranin, S-100, EMA, and CD10. The cell proliferation index was less than 1% (Fig. 1).
Oncocytoma is a tumor which is characterized by consisting only or predominantly of oncocytes, large cells with abundant eosinophilic and granular cytoplasm as a consequence of mitochodrial accumulation. Adrenocortical oncocytoma is extremely uncommon; since it was first reported in 1986, approximately 148 cases have been published in the literature,1 and most tumors were benign and non-functioning. Because of these characteristics, oncocytomas are usually diagnosed incidentally.2 These tumors have been reported at all ages, with no clear preference (mean age 47 years, range 3–77 years), and are more common in females (2.5:1) and in the left adrenal gland (3.5:1). However, approximately 20% of adrenal oncocytomas may show some degree of malignancy, and hormone hyperproduction is found in 17% of cases.3,4
Cushing's syndrome associated with adrenal oncocytoma has been reported in very few cases.5–8 The reported patient was diagnosed with Cushing's syndrome of adrenal origin, and therefore underwent surgery, which is the usually recommended therapeutic alternative9 and achieved resolution of her hypercorticism. The surgical specimen was examined based on the description by Bisceglia et al.10 for oncocytc adrenal tumors, according to which, adrenal tumors with more than 90% oncocytic cells are considered pure oncocytic tumors (A), those with 50–90% oncocytic cells are considered as mixed oncocytic tumors (B), and those with less than 50% oncocytic cells are classified as conventional adrenocortical tumors with oncocytic differentiation (C). Our case belonged to category B. The immunohistochemical profile of the tumor reported is superimposable on that of oncocytic adrenocortical tumors. These tumors are typically positive for vimentin, melan-A, alpha-inhibin, synaptophysin, and calretinin, and negative for CK20, chromogranin, S-100, EMA, and CD10.1 There are several classifications for determining the behavior of oncocytic adrenal tumors, of which the most widely accepted is the Lin–Weiss–Bisceglia classification.2 This system proposes major and minor criteria, so that the presence of at least one of the three major criteria (mitotic index greater than 5 per 50 high-power fields, atypical mitoses, and venous invasion) suggests malignancy, at least one of the four minor criteria (size greater than 10cm and/or weight greater than 200g, microscopic necrosis, capsular invasion, and sinusoid invasion) involves an uncertain malignant potential, and the absence of major and minor criteria suggests a benign potential. No major or minor criteria were found in our patient, and a potentially benign tumor was therefore diagnosed.
Adrenal oncocytoma should be considered in differential diagnosis of Cushing's syndrome of adrenal origin, or even adrenal incidentaloma, because most oncocytomas are non-functioning.
Please cite this article as: Calderón Vicente DM, Ronquillo Rubio A, Yunta Abarca P, Quílez Toboso R, Aranda Regules J. Síndrome de Cushing asociado a oncocitoma adrenocortical. Endocrinol Nutr. 2015;62:416–418.