To ascertain the number of diabetic foot units (DFUs) in Spain, the specialists working in them, and the population covered by them.
Material and methodsThe Spanish Group on the Diabetic Foot (SGDF) prepared and agreed a questionnaire based on the recommendations of the 2011 International Consensus on the Diabetic Foot (ICDF). From October to December 2012, the questionnaire was sent to members of three scientific societies formed by professionals involved in the care of patients with diabetes mellitus. Population coverage of the responding centers and DFUs was estimated using the 2012 population census.
ResultsSeventy five questionnaires were received, 64 of them from general hospitals, which accounted for 13% of the general hospitals of the National Health System. It was calculated that they provided coverage to 43% of the population. Thirty four centers answered that they had a DFU. Specialized diabetic foot care was only provided to 25% of the population. The number of different professionals working at diabetic foot units was 6.3±2.7. Classification of DFUs based on their complexity was as follows: 5 basic units (14.7%), 20 intermediate units (58.8%), and 9 excellence units (26.5%).
ConclusionsThe number of DFUs reported in this study in Spain is low, and allow for foot care of only one out of every four patients with diabetes. Spanish health system needs to improve diabetic foot care by creating new DFUs and improving the existing ones.
Conocer el número de unidades de pie diabético (UPD) que existen en España, especialidades que las integran y funcionamiento, así como la cobertura poblacional de las mismas.
Material y métodosEl Grupo Español del Pie Diabético (GEPID) elaboró y consensuó un cuestionario basándose en las recomendaciones organizativas para una clínica del pie diabético propuestas por el Consenso Internacional del Pie Diabético (CIPD) 2011. El cuestionario fue enviado desde octubre a diciembre de 2012, a los miembros de 3 sociedades científicas integradas por profesionales implicados en la atención de personas con diabetes mellitus. Se estimó la cobertura poblacional de los centros respondedores y de las UPD usando el censo poblacional 2012.
ResultadosSe recibieron 75 cuestionarios, 64 de ellos procedentes de hospitales generales, que supusieron el 13% de los hospitales generales del Sistema Nacional de Salud y se estimó que daban cobertura al 43% de la población censada en España. Respondieron que existía UPD 34 centros, estimándose que daban cobertura a un 25% de la población censada. El número de diferentes profesionales que integran las UPD es de 6,3±2,7 miembros. El análisis del tipo de UPD permitió identificar 3 modelos: mínimo 5 (14,7%), intermedio 20 (58,8%) y de excelencia 9 (26,5%).
ConclusionesEl número de UPD comunicadas en este estudio en España es escaso, permitiendo la atención como mucho de uno de cada 4 pacientes con diabetes mellitus. Se precisa mejorar la organización del cuidado del pie diabético en España, mediante la creación de UPD y mejorando las ya existentes.
Diabetic foot and its consequences, such as lower limb amputation (LLA), is a feared and well known complication of diabetes mellitus (DM). Diabetic foot care by multidisciplinary teams, ranging from those working in primary care to the most complex teams integrated in diabetic foot units (DFUs) where different healthcare professionals, including endocrinologists, podiatrists, surgeons (vascular, general and/or orthopedic), and diabetes educators, amongst others, are represented has been shown to decrease the LLA rate by 45–85% in the population with DM.1
Data recently published show that the LLA rate in people with diabetes is almost double the rate in Spain as compared to countries at a similar level of development,2 and that this trend is actually increasing.3 An improvement in the results of diabetic foot management is therefore a priority. On the other hand, there is no registry of Spanish DFUs or of the professionals working in them, and knowledge of these data is a key starting point for laying down the foundations for the improved management of this condition.
The Spanish Group on Diabetic Foot (SGDF) of the Spanish Diabetes Society (SED), consisting of different healthcare professionals, had in performing this study the following objectives: to examine the current situation of DFUs in Spain by ascertaining their number, the different specialists who work in them, and their operation, and in addition to estimate the population covered by these units.
Material and methodsThe study was conducted by means of a questionnaire prepared and agreed by all the founding members of SGDF. The questionnaires consisted of a first part containing center data, and a second part including 12 items. The questionnaire, including open-ended answers, was intended to ascertain whether the surveyed centers had DFUs and to know their members, equipment, and functions. All items were formulated based on the recommendations for the organization of diabetic foot units proposed by the 2011 International Consensus on the Diabetic Foot (ICDF).4
Dissemination of the questionnaireThe final format of the questionnaire was sent by electronic mail in an Excel file to all SED members in October 2012, and two months later, it was sent as an online survey as a reminder. The questionnaire was also available at the SED website (www.sediabetes.org/). The online questionnaire was also sent in December 2012 by electronic mail to the members of the Spanish Society of Endocrinology and Nutrition (SEEN) and the Society of Endocrinology, Nutrition, and Diabetes of Madrid (SENDIMAD). The closing date of the questionnaire was March 31, 2013.
Data analysisThe existence of DFUs at the surveyed centers was ascertained by asking whether they had a specific outpatient clinic to care for most patients with diabetic foot.
To know the overall response rate of the surveyed centers, the number of questionnaires from general hospitals as compared to the total number of hospitals of the National Health System (NHS) was calculated.5 Population coverage of the surveyed centers and those with BFUs was also estimated based on the reference population of their catchment areas in 2012. The percentage contribution of centers answering the questionnaire was calculated by dividing the whole reference population cared for by the centers in each community by the population census in each community and in Spain as a whole.6
The extent of the coverage provided by each DFU and its operational organization were evaluated in terms of the number of patients assessed as new and reviewed in the past year, with the ratios between new and reviewed patients per 100,000 inhabitants, as well as the ratio between reviewed and new patients by DFU being calculated.
DFUs were categorized into three levels based on the recommendations of the ICDF4 regarding the organization and models of diabetic foot clinics: (a) a minimum model (MM)≤3 members (physician, nurse, and podiatrist), the care of patients belonging to the catchment area only, functions being the prevention and treatment of simple lesions, basic equipment; (b) an intermediate model (IM) >3 and <6 members, the care of patients with simple and more complex lesions from the catchment area, intermediate medical equipment, functions of cooperation with hospital departments and with catchment areas; and (c) an excellence model (EM)≥6 members, the care of patients with simple and more complex lesions from inside and outside the catchment area, sophisticated equipment, collaboration with reference centers, the organization of courses and meetings, involvement in training, the presence of a leader, the involvement of professionals, and a decisive role in clinical guideline decisions.
Variable were expressed as absolute values and percentages (%) and mean±standard deviation (SD). Microsoft® Office Excel 2007 and statistical software Analyse-it for Microsoft Excel (version 2.20) were used.
ResultsQuestionnaires answered by and population coverage of diabetic foot unitsSeventy five questionnaires were received from 64 general hospitals, one university, and 10 non-hospital centers (eight healthcare centers and two specialist centers). The 64 general hospitals represented 13% of all the general hospitals in the NHS. Most centers, 64 (85.3%), were publicly funded, while nine (12%) were state-assisted private hospitals, and two (2.7%) were fully private hospitals.
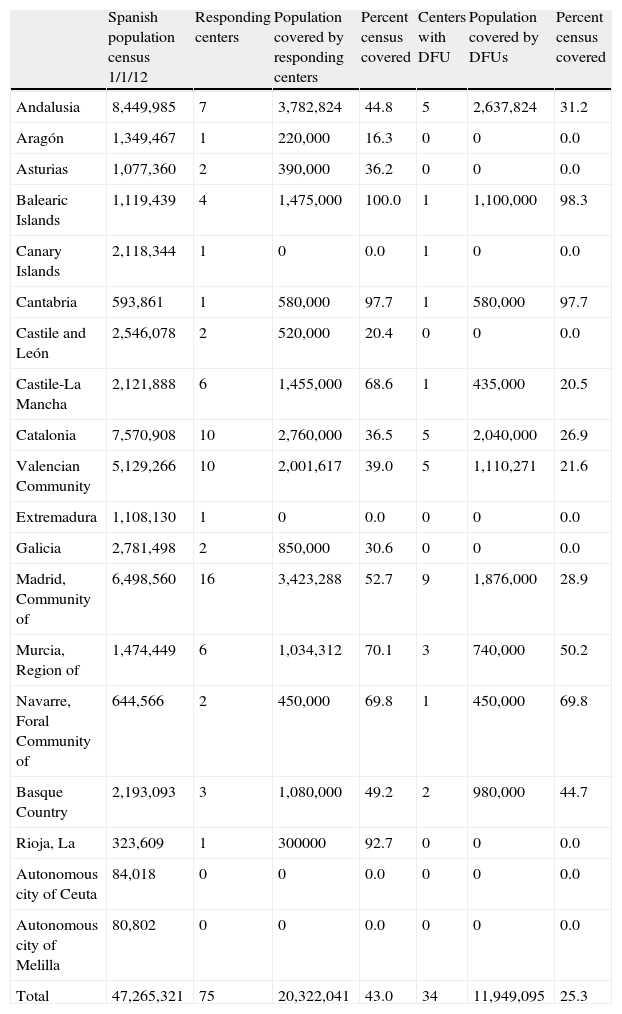
All the autonomous communities except for Ceuta and Meilla completed questionnaires, and the proportion of responding centers was proportional to the extent and number of centers of each community. The percentage of the population covered varied, being greater in communities where most of the population is seen at a few centers, as occurs in the Balearic Islands, Cantabria, and La Rioja.
For centers with an assigned reference population (n=62), the population covered was estimated at 20,323,041 inhabitants, i.e. 43% of the Spanish population census. Table 1 shows the number of centers responding by autonomous community and their population coverage.
Coverage by autonomous community of questionnaires answered and centers with diabetic foot units.
| Spanish population census 1/1/12 | Responding centers | Population covered by responding centers | Percent census covered | Centers with DFU | Population covered by DFUs | Percent census covered | |
| Andalusia | 8,449,985 | 7 | 3,782,824 | 44.8 | 5 | 2,637,824 | 31.2 |
| Aragón | 1,349,467 | 1 | 220,000 | 16.3 | 0 | 0 | 0.0 |
| Asturias | 1,077,360 | 2 | 390,000 | 36.2 | 0 | 0 | 0.0 |
| Balearic Islands | 1,119,439 | 4 | 1,475,000 | 100.0 | 1 | 1,100,000 | 98.3 |
| Canary Islands | 2,118,344 | 1 | 0 | 0.0 | 1 | 0 | 0.0 |
| Cantabria | 593,861 | 1 | 580,000 | 97.7 | 1 | 580,000 | 97.7 |
| Castile and León | 2,546,078 | 2 | 520,000 | 20.4 | 0 | 0 | 0.0 |
| Castile-La Mancha | 2,121,888 | 6 | 1,455,000 | 68.6 | 1 | 435,000 | 20.5 |
| Catalonia | 7,570,908 | 10 | 2,760,000 | 36.5 | 5 | 2,040,000 | 26.9 |
| Valencian Community | 5,129,266 | 10 | 2,001,617 | 39.0 | 5 | 1,110,271 | 21.6 |
| Extremadura | 1,108,130 | 1 | 0 | 0.0 | 0 | 0 | 0.0 |
| Galicia | 2,781,498 | 2 | 850,000 | 30.6 | 0 | 0 | 0.0 |
| Madrid, Community of | 6,498,560 | 16 | 3,423,288 | 52.7 | 9 | 1,876,000 | 28.9 |
| Murcia, Region of | 1,474,449 | 6 | 1,034,312 | 70.1 | 3 | 740,000 | 50.2 |
| Navarre, Foral Community of | 644,566 | 2 | 450,000 | 69.8 | 1 | 450,000 | 69.8 |
| Basque Country | 2,193,093 | 3 | 1,080,000 | 49.2 | 2 | 980,000 | 44.7 |
| Rioja, La | 323,609 | 1 | 300000 | 92.7 | 0 | 0 | 0.0 |
| Autonomous city of Ceuta | 84,018 | 0 | 0 | 0.0 | 0 | 0 | 0.0 |
| Autonomous city of Melilla | 80,802 | 0 | 0 | 0.0 | 0 | 0 | 0.0 |
| Total | 47,265,321 | 75 | 20,322,041 | 43.0 | 34 | 11,949,095 | 25.3 |
Census data by community were obtained from the National Statistics Institute.6
Thirty-four centers answered that they had DFUs. Of these, 31 were located in general hospitals, two in specialist centers, and one in a university. Table 1 shows the distribution of DFUs by autonomous community, as well as the percentage of the population covered. Two centers reported the planned start of operation of a DFU during 2013. Of the 34 centers with DFUs, 30 had an assigned reference population with a total coverage of 25% of the population census during 2012.
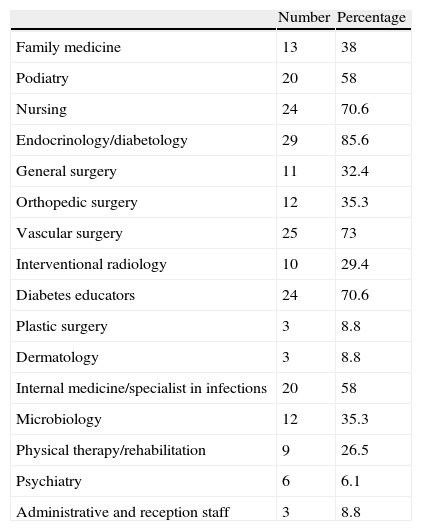
Analysis of members of diabetic foot unitsThe number and mode of different professionals ascribed to DFUs were 6.3±2.7 and six members respectively. The specialties most represented included endocrinology/diabetology (85.6%), vascular surgery (73%), and nursing (70.6%) (Table 2). Three DFUs: 3 (8.8%) had no members from the areas of surgery or podiatry, and only 20 DFUs (58%) had vascular surgeons and podiatrists.
Different specialties incorporated into diabetic foot units.
| Number | Percentage | |
| Family medicine | 13 | 38 |
| Podiatry | 20 | 58 |
| Nursing | 24 | 70.6 |
| Endocrinology/diabetology | 29 | 85.6 |
| General surgery | 11 | 32.4 |
| Orthopedic surgery | 12 | 35.3 |
| Vascular surgery | 25 | 73 |
| Interventional radiology | 10 | 29.4 |
| Diabetes educators | 24 | 70.6 |
| Plastic surgery | 3 | 8.8 |
| Dermatology | 3 | 8.8 |
| Internal medicine/specialist in infections | 20 | 58 |
| Microbiology | 12 | 35.3 |
| Physical therapy/rehabilitation | 9 | 26.5 |
| Psychiatry | 6 | 6.1 |
| Administrative and reception staff | 3 | 8.8 |
Thirty centers (88%) reported that a healthcare professional coordinated or managed the DFU; such professionals were, by decreasing frequency: an endocrinologist/diabetologist (40%), a podiatrist/endocrinologist (20%), a podiatrist (10%), a general surgeon (10%), a vascular surgeon (6.7%), and others (3%).
Analysis of operation and equipment of diabetic foot unitsMost DFUs, 27 (79.4%), used some clinical guideline for the management of patients with diabetic foot and 17 (50%) used more than one guideline, while seven DFUs used no guideline. The ICDF guideline from the International Working Group on the Diabetic Foot (IWGDF) was the one most commonly used (76.5%).4
Most DFUs (22, 64.7%) provided care only to the population from the catchment area, while some (9, 26.5%) also provided care to patients from outside their communities or catchment areas.
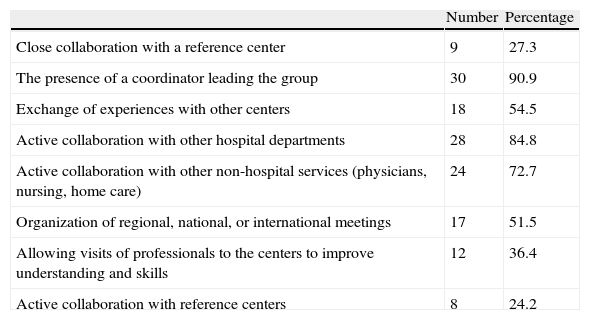
The main roles of DFUs included the prevention and treatment of all patients, including the most complex cases (29 DFUs, 85.3%), or the prevention and treatment of patients with simple lesions only (5 DFUs, 14.7%). Other functions included the education and training of other centers (17 DFUs, 50%) and the development of innovative strategies and treatments, as well as participation in clinical trials (12, 35.3%). Table 3 lists the other activities performed at DFUs.
Actions performed at diabetic foot units (n=33).
| Number | Percentage | |
| Close collaboration with a reference center | 9 | 27.3 |
| The presence of a coordinator leading the group | 30 | 90.9 |
| Exchange of experiences with other centers | 18 | 54.5 |
| Active collaboration with other hospital departments | 28 | 84.8 |
| Active collaboration with other non-hospital services (physicians, nursing, home care) | 24 | 72.7 |
| Organization of regional, national, or international meetings | 17 | 51.5 |
| Allowing visits of professionals to the centers to improve understanding and skills | 12 | 36.4 |
| Active collaboration with reference centers | 8 | 24.2 |
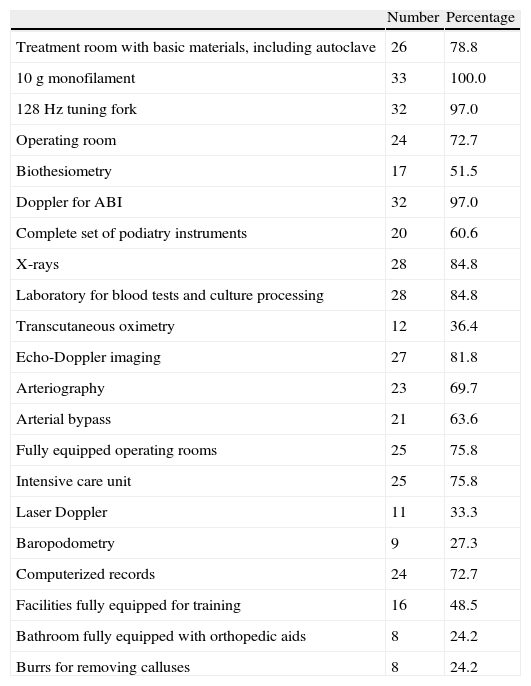
As regards equipment (Table 4), a vast majority of DFUs had basic equipment for the detection of sensory loss (monofilament and tuning fork) and noninvasive arterial examination (ABI and echo-Doppler image). Seventy percent of DFUs had access to imaging procedures for intravascular treatment (arteriography) or to revascularization procedures such as artery bypass.
Equipment/procedures available at the diabetic foot unit (n=33).
| Number | Percentage | |
| Treatment room with basic materials, including autoclave | 26 | 78.8 |
| 10g monofilament | 33 | 100.0 |
| 128Hz tuning fork | 32 | 97.0 |
| Operating room | 24 | 72.7 |
| Biothesiometry | 17 | 51.5 |
| Doppler for ABI | 32 | 97.0 |
| Complete set of podiatry instruments | 20 | 60.6 |
| X-rays | 28 | 84.8 |
| Laboratory for blood tests and culture processing | 28 | 84.8 |
| Transcutaneous oximetry | 12 | 36.4 |
| Echo-Doppler imaging | 27 | 81.8 |
| Arteriography | 23 | 69.7 |
| Arterial bypass | 21 | 63.6 |
| Fully equipped operating rooms | 25 | 75.8 |
| Intensive care unit | 25 | 75.8 |
| Laser Doppler | 11 | 33.3 |
| Baropodometry | 9 | 27.3 |
| Computerized records | 24 | 72.7 |
| Facilities fully equipped for training | 16 | 48.5 |
| Bathroom fully equipped with orthopedic aids | 8 | 24.2 |
| Burrs for removing calluses | 8 | 24.2 |
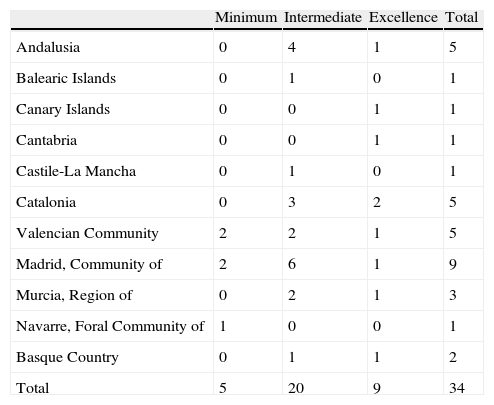
An analysis of the types of DFUs led to our identifying five DFUs (14.7%) as being MMs, 20 (58.8%) as IMs, and 9 (26.5%) as EMs. The distribution of these types of DFUs in the autonomous communities was proportional to the number of units in each community ((Table 5).
Distribution of types of diabetic foot unit (minimum, intermediate, and excellence models) by autonomous communities.
| Minimum | Intermediate | Excellence | Total | |
| Andalusia | 0 | 4 | 1 | 5 |
| Balearic Islands | 0 | 1 | 0 | 1 |
| Canary Islands | 0 | 0 | 1 | 1 |
| Cantabria | 0 | 0 | 1 | 1 |
| Castile-La Mancha | 0 | 1 | 0 | 1 |
| Catalonia | 0 | 3 | 2 | 5 |
| Valencian Community | 2 | 2 | 1 | 5 |
| Madrid, Community of | 2 | 6 | 1 | 9 |
| Murcia, Region of | 0 | 2 | 1 | 3 |
| Navarre, Foral Community of | 1 | 0 | 0 | 1 |
| Basque Country | 0 | 1 | 1 | 2 |
| Total | 5 | 20 | 9 | 34 |
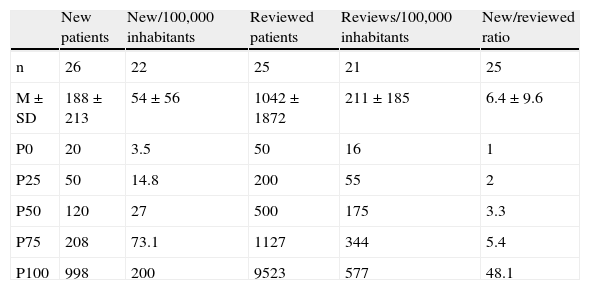
Patients assessed at DFUs could only be analyzed at 25 centers. Table 6 shows patients seen for the first time and subsequently per 100,000 inhabitants.
Analysis of patients (new and reviewed) assessed at diabetic foot units and ratio per 100,000 inhabitants.
| New patients | New/100,000 inhabitants | Reviewed patients | Reviews/100,000 inhabitants | New/reviewed ratio | |
| n | 26 | 22 | 25 | 21 | 25 |
| M±SD | 188±213 | 54±56 | 1042±1872 | 211±185 | 6.4±9.6 |
| P0 | 20 | 3.5 | 50 | 16 | 1 |
| P25 | 50 | 14.8 | 200 | 55 | 2 |
| P50 | 120 | 27 | 500 | 175 | 3.3 |
| P75 | 208 | 73.1 | 1127 | 344 | 5.4 |
| P100 | 998 | 200 | 9523 | 577 | 48.1 |
Mean±SD, P0–P100: percentile distribution.
This study represents the first attempt to ascertain the number of DFUs in Spain, as well as analysing the professionals working in them and some aspects of how these units operate. It suggests that, apparently, no more than one out of every four Spanish patients with diabetic foot is seen by a multidisciplinary team as recommended by the ICDF.
The study design included a questionnaire which was based on the ICDF recommendations and guidelines for the organization of diabetic foot units and accepted by the members of the SGDF with experience in this complication.
The questionnaire was sent to professionals involved in the care of diabetes, some of them in the specific care of patients with diabetic foot. These were mainly specialists in endocrinology, and internal medicine, nurses and diabetes educators, as well as a smaller proportion of primary care physicians and podiatrists. The dissemination of the questionnaire among more than 1800 members of SED, more than 1500 members of SEEN, and more than 170 members of SENDIMAD ensured the coverage of virtually all the professionals concerned working in the NHS hospital system.
The response was poor, as only 75 questionnaires were received, accounting for only 13% of all NHS general hospitals. If the center had no DFU, only two questions had to be answered. Low participation was considered to reflect the little attention usually paid to diabetic foot by Spanish endocrinologists, who were the healthcare professionals surveyed in most cases.
However, the centers were considered to be highly representative, as they covered 43% of the population. The lack of agreement between the low proportion of responding centers (13%) and the wide population represented may be explained by the fact that most of the hospitals which responded were those of a larger size and with more human and material resources. On the other hand, the reference populations of hospitals of different levels in large regions sometimes overlap, and are grouped in hospitals of the highest level.
Six different specialists usually staff the DFUs, of which endocrinologists or diabetologists, as well as vascular surgeons, are the most common. Surprisingly, three so-called DFUs had no member from the surgical field or podiatrist, which does rather question their right to be considered true DFUs.4,7,8 It is perhaps even more striking that only 20 DFUs (58%) had a vascular specialist and a podiatrist on their staff. These professionals are indispensable for the adequate operation of a DFU because they are able to resolve many of the problems occurring in patients with diabetic foot, regardless of their complexity.9
Recently, a study by Jurado-Campos et al.10 analyzed the resources and model of care for diabetic foot in Catalonia in 2008 using a structured survey to a sample of 36 basic healthcare areas and 118 surgical centers. The study found that no more than 10–20% of primary care and surgical centers, respectively, had podiatrists on their staff.
Both this study10 and ours demonstrate the limited access to podiatrists in the NHS. These are not among the healthcare professionals hired by the public health system, and only a few of them are now being hired in some autonomous communities.
It should also be noted that family doctors were only reported in 38% of DFUs, despite the fact that they are essential for the adequate prevention and referral of these patients.4 In Spain, the multidisciplinary unit protocol of Hospital de Cruces could serve as a model document representing what a DFU should be.11 This DFU includes primary care teams, hospital outpatient clinics, acute hospitalization, and home hospitalization. These are grouped in a multidisciplinary team with a common podiatrist–vascular axis.
Thirty of the 34 DFUs reported a leader, most commonly the endocrinologist and/or podiatrist. This agrees with the usual model in Europe, while in the United States the podiatrist is usually the coordinator of large DFUs.9
When DFUs were classified by model, the IM model was most common, followed by the EM, while the MM model was uncommon. This was to be expected: hospitals gave a majority response, and the poor development of clinics and DFUs in Spain explains their low response. The Jurado-Campos et al. study10 found that, among the 85 surgical centers caring for patients with diabetic foot. 11 (13%) were of the EM type and 29 (34%) of the IM type. However, the primary study objective was to ascertain whether the centers surveyed had the resources to care for this condition. It should also be considered that, in standard clinical practice, healthcare for diabetic foot is rarely provided by units consisting of multidisciplinary teams caring for most patients living in the catchment area and following the recommendations of the ICDF.12
Analysis of the number of patients attending DFUs for new and subsequent visits showed a great difference in population coverage between them, reflecting the fact that many of them do not see the majority of patients with diabetic foot in their reference population. If we consider the infrastructure for diabetic foot care in primary care, which does not correspond to what is considered a multidisciplinary team, it is very likely that many patients seen at such DFUs do not benefit from the ICDF recommendations and guidelines.4 However, their role in prevention, the so-called minimum model, is essential. The reviewed/new patient ratio was also highly variable, demonstrating differences in working procedures between the DFUs. It should be borne in mind that many patients with ulcers require multiple visits, and that mean healing time is not less than 15 weeks,13 despite which our study found that new patients were not seen more than twice in one out of every four DFUs.
One of the main study objectives of this questionnaire was to estimate the size of the population benefiting from the existence of a DFU in the NHS. Table 1 shows that only 25% of the population in the 2012 census, and thus of patients with DM, were receiving care at DFUs. However, because of the functional limitations of the various specialist skills represented in DFUs and the number of new patients seen by assigned populations, the actual figures may be lower. The low percentage of response of the professionals surveyed also suggests a low interest on the part of the healthcare professionals involved in the care for patients with DM in this complication. Both results may partly explain the high amputation rate in Spanish patients with DM despite the generally high quality of care for diabetic patients.14
The limitations of this study included:
- –
Its low dissemination among those professionals concerned who are not attached to hospitals, such as family doctors and podiatrists, most of whom are not members of the scientific societies to which the questionnaire was sent. It should be noted, however, that the specialized care for diabetic foot by both these groups of professionals outside multidisciplinary teams is probably exceptional.
- –
The existence of units not dependent on the endocrinology department at some hospitals which had therefore no access to the channels where the survey was disseminated.
- –
The risk of a low response rate and the difficulty of verifying the information collected and, thus, the accuracy of the data received. Because of the characteristics of the method, the actual number of professionals who received the survey could not be determined.
- –
The majority participation of centers better prepared and with more resources probably caused a participation bias, which may have led to our underestimating the number of units with an MM.
The study strengths included:
- –
The wide dissemination of the study questionnaire among the professionals concerned.
- –
The similar accuracy and percentage response of the questionnaire as compared to other methods of collecting information (telephone interview or regular post).15
The conclusion of this study is that the number of DFUs in Spain is low, and that probably as many as one out of every four patients with DM have no access to a DFU. The organization of diabetic foot care in Spain should be increased and improved by creating DFUs following the organizational models of the IWGDF and enhancing and/or improving the available DFUs.
Funding and means for study conductThis study was conducted using the means provided by the SED according to the rules for working groups. Specifically, this allowed for a meeting of the group members for that purpose, and covered the cost of computer support for the questionnaire in its online version.
Conflicts of interestThe authors state that they have no conflicts of interest.
We thank all members of SED, SEEN, and SENDIMAD for their unselfish participation by completing this questionnaire. We also thank the boards of all three societies for permitting the dissemination of the questionnaire on DFU throughout Spain.
Almaraz Almaraz, María Cruz (Hospital Universitario Carlos Haya, Málaga); Antolín Santos, Juan B. (Centro de Salud de Mansilla de las Mulas, León); Aragón Sánchez, F. Javier (Hospital La Paloma, Las Palmas de Gran Canaria); Costa Lima, Elisabet (Hospital Universitario Dr. Josep Trueta, Girona); Díaz Pérez, José Ángel (Hospital Universitario Clínico de San Carlos, Madrid); Doriá Cervós, Monserrat (Hospital Arnau de Vilanova de Lleida, Lleida); Fabbi, Matteo (Hospital General de Catalunya, Sant Cugat del Vallès); García Morales, Esther (Clínica Universitaria de Podología; Universidad Complutense de Madrid, Madrid); Lázaro Martínez, José Luis (Clínica Universitaria de Podología; Universidad Complutense de Madrid, Madrid); Lozano del Hoyo, María Luisa (Centro de Salud Las Fuentes Norte, Zaragoza); Mauricio Puente, Didac (Hospital Germans Trias i Pujol, Badalona); Rubio García, José Antonio (Hospital Universitario Príncipe de Asturias, Alcalá de Henares); Vela Orús, María Pilar (Hospital Universitario de Cruces, Barakaldo); Viadé Julià, Jordi (Hospital Germans Trias i Pujol, Badalona); Yoldi Arrieta, Alfredo (Hospital Donostia; Donostia).
Please cite this article as: Rubio JA, Aragón-Sánchez J, Lázaro-Martínez JL, Almaraz MC, Mauricio D, Antolín Santos JB, et al. Unidades de pie diabético en España: conociendo la realidad mediante el uso de un cuestionario. Endocrinol Nutr. 2014;61:79–86.
The Spanish Group Diabetic Foot (Gepid) is a multidisciplinary group composed of members of the Spanish Society of Diabetes, whose current composition is given in Annex at end of article.