To ascertain whether patients with type 2 diabetes are screened for diabetic foot, and to analyze the factors related to patients and centers associated with performance of such screening.
Materials and methodsA multicenter, epidemiological, cross-sectional study was conducted. The clinical records of 443 patients with type 2 diabetes monitored at Primary Care for at least 12 months were reviewed. Demographic and healthcare variables and characteristics of the Primary Care Center were recorded.
ResultsIn the previous year, 51.2% of the patients had been trained on foot self-care, 56.4% had undergone foot inspection, 39.5% had been examined with a monofilament, and palpation of peripheral pulses and measurement of the ankle-brachial index were performed in 45.8% and 10.1% of the patients, respectively. Diabetic foot screening (inspection, monofilament testing, and palpation of peripheral pulses) was performed in 37% of the study patients. Ulcer risk stratification was done in 12.4% of the patients. A significant association was found between diabetic foot screening and presence of foot deformities (p<0.001), history of neuropathy (p=0.005), and history of peripheral artery disease (p<0.05). Screening was also associated to some characteristics of the center, such as reception of information about goal achievement (p<0.001) and economic incentives for goal attainment (p<0.001).
ConclusionsCompliance with diabetic foot screening and ulcer risk stratification in patients with type 2 diabetes in Primary Care was poor.
Conocer si se realiza el cribado del pie diabético en pacientes con diabetes tipo 2 atendidos en Atención Primaria y analizar qué factores relacionados con el paciente y el centro de salud se asocian a la cumplimentación de dicho cribado.
Material y métodoEstudio epidemiológico, transversal y multicéntrico. Se revisaron las historias clínicas de una muestra representativa (n=443) de pacientes con diabetes tipo 2 que habían sido seguidos en Atención Primaria como mínimo en los 12 meses previos. Se registraron variables demográficas, de proceso asistencial y características del centro.
ResultadosEl 51,2% de los pacientes recibieron educación sanitaria sobre el autocuidado del pie, al 56,4% se le realizó inspección de los pies, el 39,5% fueron explorados con monofilamento, y en el 45,8 y 10,1% se realizó palpación de pulsos periféricos e índice tobillo-brazo, respectivamente. El cribado del pie diabético (inspección, exploración de sensibilidad con monofilamento y palpación de pulsos periféricos) fue efectuado al 37% de los pacientes estudiados, y la estratificación del riesgo de úlceras se determinó en el 12,4% de los casos. Existe asociación entre realización del cribado y presencia de deformidades en el pie (p<0,001), antecedentes de neuropatía (p=0,005) y arteriopatía periférica (p<0,05). También se asocia a algunas características del centro: recibir información sobre consecución de objetivos (p<0,001), y percepción de incentivos económicos por cumplimiento de los mismos (p<0,001).
ConclusionesSe constata una deficiente atención a las personas con diabetes tipo 2 respecto a la prevención del pie diabético, pues no se realiza de forma rutinaria cribado y estratificación de riesgo.
The term diabetic foot encompasses any lesion in the feet: infection, ulcer, and destruction of deep tissues occurring as the result of diabetes and its complications.1 Diabetic foot is the main cause of non-traumatic amputation in Western countries, may cause death or physical and psychical disability, has a great impact on quality of life, and represents a high cost for society.2,3
In Spain, incidence of amputations related to type 2 diabetes mellitus (T2DM) has increased in recent years.4 It is estimated that approximately 15% of the patients with diabetes will develop ulcers in their lower limbs during their lifetime. Of these, 7–20% will require limb amputation.5
In order to decrease ulcer incidence, the American Diabetes Association (ADA) recommends that patients with diabetes receive general diabetes education in foot care and undergo careful examination to identify risk factors for ulcer and amputation.6 Examination should include inspection, measurement of peripheral pulses, and assessment of protective sensation with monofilament, as well as any other test such as examination of vibration sensitivity or achillean reflexes. Moreover, since peripheral artery disease (PAD) is asymptomatic in many patients, consideration of assessment of the ankle-brachial index (ABI) is advised. Clinical practice guidelines also recommend that foot screening is performed at the time T2DM is diagnosed and a risk category that will determine the frequency of subsequent examinations is assigned.7,8
Structured programs for foot screening, management of the foot at risk, and control of risk factors are the most effective measures to prevent foot ulcers9; however, various studies conducted in Spain demonstrate that foot examination is one of the activities least complied with at the monitoring visits.10–13
The primary objective of this study was to ascertain whether screening of the foot at risk is performed in patients with T2DM, and the secondary objective was to assess which factors related to the patient and the primary care team (PCT) are associated to this activity.
Patients and methodsThis was a multicenter, descriptive, cross-sectional study where a review was conducted of a random, representative sample of clinical histories from patients with T2DM who attended 17 health care centers non-randomly distributed in 11 Spanish autonomous communities.
Inclusion criteria were prior diagnosis of T2DM and prior care in PC for this disease for at least the past 12 months. Major amputation of both lower limbs was an exclusion criterion. Patients with minor amputations or major amputations in a single limb were included in the study.
Once the listings of patients with diabetes (n=23,936) ascribed to the participating PCTs were obtained, sample size was calculated with a 95% confidence level and a 5% precision, and giving to the proportion of the tested parameter the value that maximized sample size (p=0.05), which was in turn increased by 15% to anticipate for losses. This resulted in a total sample of 445 patients.
Selection was performed at each health care center by systematic sampling in proportion to the population of patients with diabetes in each center. Two patients were excluded because they did not meet the inclusion criteria, and data from 443 patients were therefore finally analyzed.
Clinical records were reviewed during October and November 2012. Demographic data (age and sex), time since disease onset, and prevalence of risk factors for ulceration or amputation were collected. Variables collected included active smoking if recorded in the clinical history; diabetic retinopathy if diagnosed by retinography or eye fundus examination by an ophthalmologist, or recorded in a hospital report; neuropathy, PAD, and history of amputation if recorded in clinical history or any hospital report; history of foot ulcers if recorded in the medical history or center records included care for this reason; and foot deformities if clinical history included presence of hallux valgus, claw or hammer toes, pes cavus, flat foot, or any other deformity.
It was also recorded if in the past year patients had been instructed on foot care and a clinical history of symptoms related to neuropathy and peripheral artery disease had been taken. The following foot examinations and the degree of compliance with each of them were recorded: inspection, distal pulse examination, ABI, examination of sensitivity with monofilament and/or tuning fork, and achillean reflex.
In compliance with the criteria of the Clinical Practice Guidelines of the Ministry of Health,7 screening was considered to be performed if inspection, peripheral pulse examination, and a monofilament test were recorded.
It was analyzed whether ulcer risk had been stratified, accepting any classification by risk level. To unify criteria, investigators were asked to stratify ulcer risk of each patient, based on data collected from the clinical history, using the classification proposed in the 2007 International Consensus on the Diabetic Foot.14
Information was subsequently requested to the head of research at each center on the following characteristics of the PCT: availability of pregraduate/postgraduate teaching, care pressure, available resources for foot examination, if health care professionals were informed of the results achieved, and if they were rewarded for their achievement.
Data were recorded into electronic questionnaires prepared for such purpose. An overall descriptive statistical analysis was performed. Mean and standard deviation (SD) were calculated for quantitative variables, and percentages with their 95% confidence intervals (95% CI) for qualitative variables. A Chi-square test and a Student's t test were used to compare percentages and means, respectively. A value of p<0.05 was considered statistically significant. The Statistical Package for Social Sciences – SPSS® – for Windows®, version 20.0, was used for statistical analysis.
ResultsData from the clinical histories of 443 patients with T2DM were collected. Mean patient age was 68.9 years (SD 12). Fifty-two percent of the patients were female patients. Mean time since disease onset was 9.2 years (SD 6.4), with a median of 8.4 years, although this data was not recorded in 19.8% of the cases.
The 14.2% (95% CI 11.0–17.5) of the patients were smokers, and 20.5% (95% CI 16.8–24.3) were former smokers, while no smoking status was reported in 16.4% (95% CI 13.0–19.9) of clinical histories.
Table 1 summarizes the prevalence of risk factors for ulcers.
Prevalence of risk factors for ulceration and/or amputation.
| Risk factors | Patients, n (%) | 95% CI |
| Smoking | 63 (14.2) | 11.0–17.5 |
| Retinopathy | 52 (11.7) | 8.7–14.7 |
| Foot deformities | 64 (14.4) | 11.2–17.7 |
| Peripheral neuropathy | 38 (8.6) | 6.0–11.2 |
| Peripheral artery disease | 42 (9.5) | 6.8–12.2 |
| Prio ulcers | 27 (6.1) | 3.9–8.3 |
| Prior amputations | 3 (0.7) | 0.1–1.4 |
CI: confidence interval.
Health education on foot care had been given to 51.2% of the patients; history of symptoms of neuropathy and peripheral artery disease had been taken in 30.7% and 30.0%, respectively; foot inspection had been performed in 56.4%, monofilament examination in 39.5%, distal pulse examination in 45.8%, and ABI in 10.1%. Screening was performed in 37% of the study patients (Table 2).
Proportion of patients given education, taken a clinical history, and performed examination.
| Patients, n (%) | 95% CI | |
| Foot care education | 227 (51.2) | 45.7–55.0 |
| History on peripheral neuropathy | 136 (30.7) | 24.4–35.0 |
| History on peripheral artery disease | 133 (30.0) | 25.8–34.3 |
| Foot inspection | 250 (56.4) | 51.8–61.1 |
| Examination with monofilament | 175 (39.5) | 35.0–44.1 |
| Examination of peripheral pulses | 203 (45.8) | 41.2–50.5 |
| Examination with tuning fork | 78 (17.6) | 14.1–21.2 |
| Examination of achillean reflex | 37 (8.3) | 5.8–10.9 |
| Ankle-brachial index | 45 (10.1) | 7.3–13.0 |
| Screening (inspection. monofilament. peripheral pulses) | 164 (37.0) | 32.5–41.5 |
| Examination of peripheral pulses, monofilament and other examination (tuning fork, tenderness, achillean reflex) | 138 (31.1) | 26.8–35.5 |
CI: confidence interval.
Peripheral pulse palpation was the examination most commonly performed. ABI was only estimated in 9 of the 17 patients with no peripheral pulses in some limb. No foot examination was recorded in 40.6% (95% CI 36.1–45.2) of the reviewed histories, including those of 6 patients with a history of ulcers.
Risk stratification was not recorded in 87.6% (95% CI 84.5–90.7) of the histories. Investigators tried to stratify risk based on information from the clinical records, but this was not possible in 65% (95% CI 60.6–69.5) of the cases due to missing data. Among patients in whom risk could be stratified, 25.8% had a high risk of ulceration (Grade 2 and 3) (Table 3).
Stratification of foot ulcer risk in patients with diabetes according to the criteria of the 2007 International Consensus on the Diabetic Foot.
| Risk | Definition | Patients, n (%) | 95% CI |
| 0 | No DPS, palpable PPs, no deformity or ulcer history | 62 (40.0) | 32.3–47.7 |
| 1 | DPS, palpable PPs | 53 (34.2) | 26.7–41.7 |
| 2 | DPS and absent PPs and/or foot deformity. Also if absent PPs and no DPS | 23 (14.8) | 9.2–20.4 |
| 3 | History of ulcer and/or amputation | 17 (11.0) | 6.1–15.9 |
DPS: decreased protective sensation; CI: confidence interval; PP: peripheral pulses.
Screening was performed in 37% (95% CI 31.1–40.5) of the female and 47.8% (95% CI 33.4–62.3) (p=0.061) of the male patients.
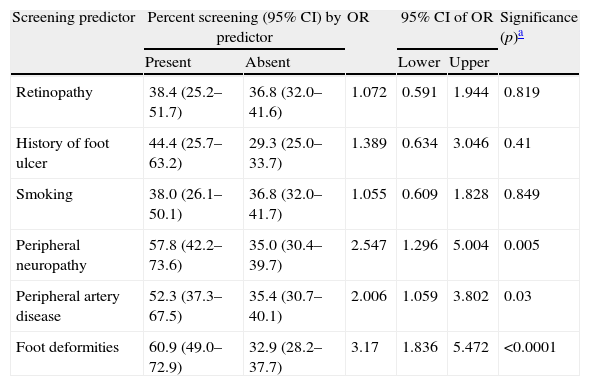
Table 4 shows the proportion of patients with and without risk factors for ulcer who underwent screening. This was performed in a significantly higher proportion of patients with foot deformities, history of peripheral neuropathy, and PAD. No association was seen between performance of screening and smoking, history of ulcer, or retinopathy.
Risk factors for ulcer and performance of screening.
| Screening predictor | Percent screening (95% CI) by predictor | OR | 95% CI of OR | Significance (p)a | ||
| Present | Absent | Lower | Upper | |||
| Retinopathy | 38.4 (25.2–51.7) | 36.8 (32.0–41.6) | 1.072 | 0.591 | 1.944 | 0.819 |
| History of foot ulcer | 44.4 (25.7–63.2) | 29.3 (25.0–33.7) | 1.389 | 0.634 | 3.046 | 0.41 |
| Smoking | 38.0 (26.1–50.1) | 36.8 (32.0–41.7) | 1.055 | 0.609 | 1.828 | 0.849 |
| Peripheral neuropathy | 57.8 (42.2–73.6) | 35.0 (30.4–39.7) | 2.547 | 1.296 | 5.004 | 0.005 |
| Peripheral artery disease | 52.3 (37.3–67.5) | 35.4 (30.7–40.1) | 2.006 | 1.059 | 3.802 | 0.03 |
| Foot deformities | 60.9 (49.0–72.9) | 32.9 (28.2–37.7) | 3.17 | 1.836 | 5.472 | <0.0001 |
CI: confidence interval; OR: odds ratio.
There were marked differences between PCTs with regard to screening completion (Fig. 1); provision of information to professionals about the goals achieved and perception of economic incentives associated to their achievement were associated to performance of screening (Table 5).
Center characteristics and performance of screening.
| Screening predictor | Percent screening (95% CI) by predictor | OR | 95% CI of OR | Significance (p)a | ||
| Present | Absent | Lower | Upper | |||
| Teaching | 37.0 (31.1–40.5) | 47.8 (33.4–62.3) | 0.607 | 0.329 | 1.122 | 0.109 |
| Objectives | 60.9 (54.6–67.2) | 11.3(7.0–15.5) | 12.25 | 7.426 | 20.207 | <0.0001 |
| Incentives | 49.8 (43.7–55.9) | 19.7 (14.0–25.4) | 4.049 | 2.62 | 6.258 | <0.0001 |
CI: confidence interval; OR: odds ratio.
Mean care pressure in the centers ranged from 30 to 55 patients daily. There was virtually no correlation between care pressure at each center and the proportion of patients who underwent screening (Pearson's correlation, r=0.0240).
Portable Doppler devices, reflex hammer, and Semmes–Weinstein monofilament were available at all centers.
DiscussionResults of this study show that diabetic foot screening is not systematically performed in patients with T2DM, although it is true that screening is done in a greater proportion of those with history of neuropathy and PAD, the main diseases underlying ulcers. It appears logical that screening is performed if patients have a history of these conditions, because they have a high risk of ulcers. On the other hand, they may have symptoms of neuropathy or artery disease and require lower limb examination.
Distal pulse inspection and palpation are the most common examinations, possibly because they require no instruments and are done in the shortest time. By contrast, ABI was estimated in only 10% of the patients. However, data from the last year were analyzed, and it is therefore likely that it had been previously determined in some patients, and had not been repeated because the initial result was normal.
Ulcer risk stratification is important because closer monitoring, even at specialized units,1 is required in high-risk patients; ulcer risk stratification was however limited in our study, and when recorded, the classification categories used were heterogeneous because of the variety of computer clinical history models used in the different autonomous communities.
This lack of homogeneity makes it difficult to provide uniform clinical information. Thus, while in some autonomous communities, items in clinical history allowed for classifying risk as mild, moderate, and severe; in other cases it could only be stated if the foot was at risk or not. This variability in records related to diabetes has already been reported by other authors.15
Education in foot self-care has been scarce, that is, structured education is not provided despite the fact that efficacy of education is known to depend on regularity rather than on the intervention itself. It should be a continued activity over time in order to maintain progress.16
Great disparity exists between the teams in performance of screening, which cannot be attributed to differences in care pressure. The results show that centers where professionals receive information about goal achievement perform screening in a significantly greater proportion. Audits and feedback are known to result in improved care quality, and efficacy is greater when, as occurred in this case, initial compliance of the recommended practice is low.17 A systematic review of the effects of feedback to PC physicians on quality of care for patients with T2DM concluded that feedback improved care for diabetics and, more specifically, foot examination.18 In our environment, a study conducted in Catalonia13 demonstrated an improved quality of care for diabetic patients after regular care evaluations and reporting of the results to the centers to promote implementation of corrective actions.
This study also demonstrates that an additional aspect associated to performance of screening is the perception of economic incentives associated to goal achievement in general (not necessarily related to care for diabetic patients). Several authors have shown that pay for performance improves quality of care in chronic diseases,19,20 and specifically in diabetes, but results tend to regress when incentives are removed.21
Foot screening was done in 37% of the patients, a higher proportion than the 22.9% of patients reported in a study conducted in Andalusia using the same criteria as the current study.12 No comparisons could be made with other studies because they did not provide data about screening, only reported that foot examination had been performed, without specifying the tests done. In this regard, the study group of diabetes in PC, redGDPS, reported foot examination rates ranging from 47.3% to 64.2% in studies assessing various quality indicators and their change over time.10,13 Carral San Laureano et al., in a study assessing the quality of care given to a population with diabetes both in PC and endocrinology clinics, found that foot examination had been performed in 44% of the patients.22
As noted above, distal pulse inspection and examination was most commonly performed. This finding agrees with that reported by Arrieta et al.,11 but the latter reached a high degree of compliance with care processes, although they conducted a prospective study where only patients from the catchment population of investigators were enrolled, which may have involved a selection bias as they surely were professionals with a greater motivation for monitoring and follow-up of patients with diabetes. By contrast, ABI was measured in a low number of patients. The ADA provides no guidelines on who should undergo this test and when,6 and advises that its relevance is assessed, because peripheral artery disease is often asymptomatic. However, the ADA consensus panel for peripheral vascular disease recommends that ABI is measured in people with diabetes older than 50 years, and should be considered in younger people who have several cardiovascular risk factors, and repeated every five years if normal.23 In our environment, some authors justify the convenience of estimating ABI in all diabetic patients monitored in PC because of the high prevalence of PAD in this population,24 while other guidelines do not advise routine performance of this examination because it is difficult in PC and falsely elevated results may be found due to the frequency of arterial calcifications in these patients.25
This study has the limitations inherent to an observational study in which information and selection bias cannot be ruled out. Other limitations include lack of center randomization and data sources with deficient records for some variables.
With the above stated limitations, the main study contribution is to confirm deficiencies in diabetic foot screening and risk stratification, which should lead to a reflection on the reasons and prompt the health care administration to take practical measures to promote performance of diabetic foot screening; prevention and foot care programs are highly cost-effective interventions for the care system and for people with diabetes.9 Overall, a wide margin for improvement exists; the number of patients amenable to intensification of educational interventions and examination is very high, and strategies to improve quality of diabetes management increase the chance of detecting high-risk foot.26
Conflicts of interestThe authors state that they have no conflicts of interest in relation to publication of this article.
The other members of the Working Group on Diabetes of SEMERGEN who participated in this study are: Juan Carlos Aguirre Rodríguez (CS Casería de Montijo, Granada), Alfonso Barquilla García (EAP Trujillo, Cáceres), Celia Cols Sagarra (ABS Martorell Rural, Barcelona), José Escribano Serrano (UGC San Roque, Cádiz), Tomás Fuster Bellido (CS Gandía-Beniopa, Valencia), Francisco García Gallego (CS Don Benito Este, Badajoz), Antonio Hormigo Pozo (UGC Puerta Blanca, Málaga), Carmen Huidrobo Dosal (CS Centro, Santander), Jesús Iturralde Iriso (CS Casco Viejo, Vitoria), Luis Mendo Giner (CS Valtierra Cadreita, Navarra), Sonia Miravet Jiménez (ABS Martorell Urbano, Barcelona), Ana Moreno Moreno (CS San Roque, Badajoz), and María Paz Pérez Unanua (CS Dr. Castroviejo, Madrid).
Please cite this article as: Alonso-Fernández M, Mediavilla-Bravo JJ, López-Simarro F, Comas-Samper JM, Carramiñana-Barrera F, Mancera-Romero J, et al. Evaluación de la realización del cribado del pie diabético en Atención Primaria. Endocrinol Nutr. 2014;61:311–317.