In 2009, the Andalusian Society of Endocrinology and Nutrition designed a protocol for subcutaneous insulin treatment in hospitalized non-critically ill patients (HIP).
ObjectiveTo analyze implementation of HIP at tertiary care hospitals from the Andalusian Public Health System.
MethodA descriptive, multicenter study conducted in 8 tertiary care hospitals on a random sample of non-critically ill patients with diabetes/hyperglycemia (n=306) hospitalized for ≥48h in 5 non-surgical (SM) and 2 surgical (SQ) departments. Type 1 and other specific types of diabetes, pregnancy and nutritional support were exclusion criteria.
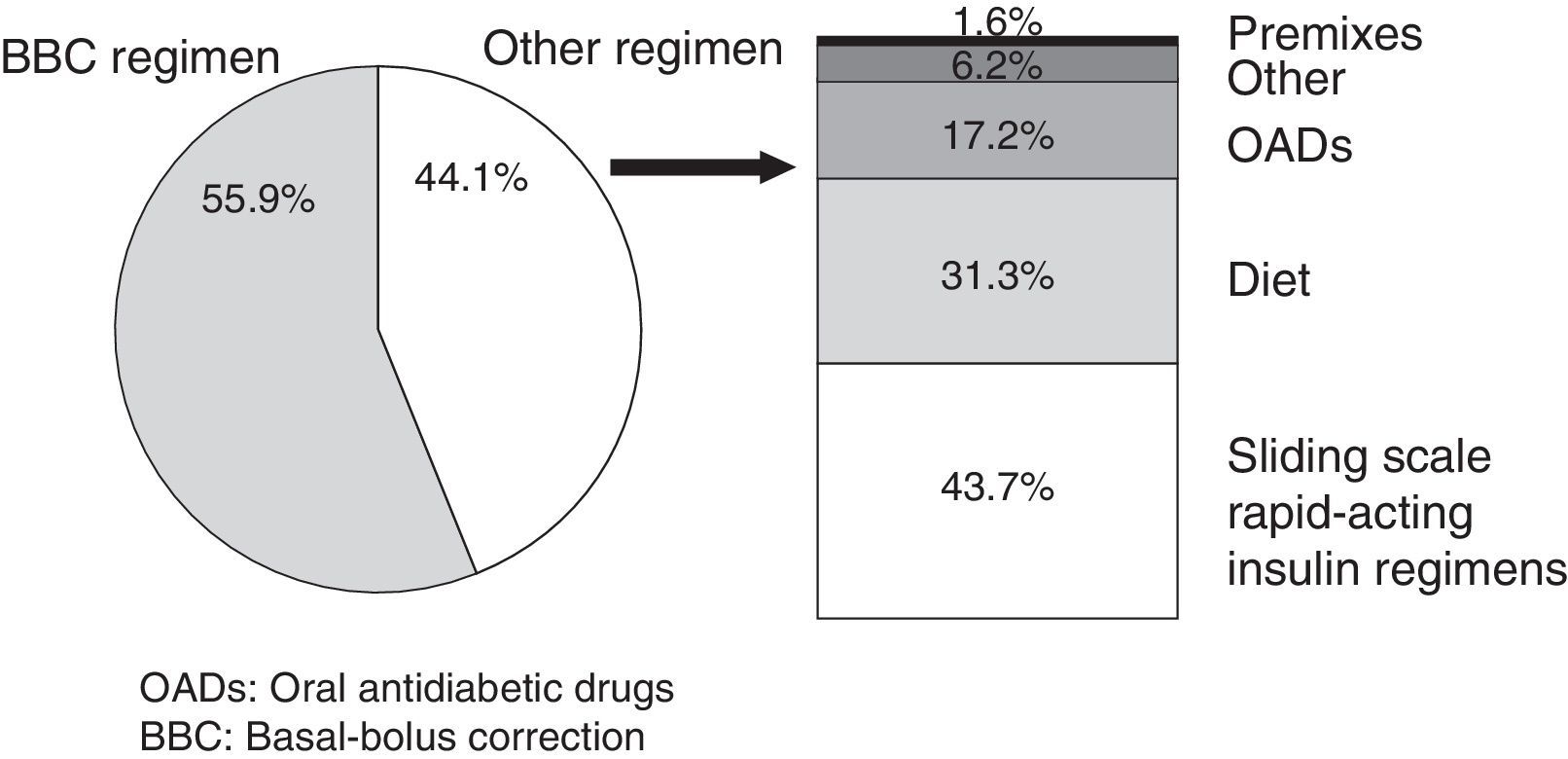
Results288 patients were included for analysis (62.5% males; 70.3±10.3 years; 71.5% SM, 28.5% SQ). A scheduled subcutaneous insulin regimen based on basal-bolus-correction protocol was started in 55.9% (95%CI: 50.5–61.2%) of patients, 63.1% SM vs 37.8% SQ (p<.05). Alternatives to insulin regimen based on basal-bolus-correction included sliding scale insulin (43.7%), diet (31.3%), oral antidiabetic drugs (17.2%), premixed insulin (1.6%), and others (6.2%). For patients previously on oral antidiabetic drugs, in-hospital insulin dose was 0.32±0.1IU/kg/day. In patients previously on insulin, in-hospital insulin dose was increased by 17% [−13–53], and in those on insulin plus oral antidiabetic drugs, in-hospital insulin dose was increased by 26.4% [−6–100]. Supplemental insulin doses used for <40IU/day and 40–80IU/day were 72.2% and 56.7% respectively. HbA1c was measured in 23.6% of patients (95CI%: 18.8–28.8); 27.7% SM vs 13.3% SQ (p<.05).
ConclusionsStrategies are needed to improve implementation of the inpatient subcutaneous insulin protocol, particularly in surgical departments. Sliding scale insulin is still the most common alternative to insulin regimen based on basal-bolus-correction scheduled insulin. Metabolic control assessment during hospitalization should be encouraged.
En 2009, la Sociedad Andaluza de Endocrinología y Nutrición diseñó un protocolo de insulinización subcutánea para pacientes hospitalizados no críticos (“Protocolo de insulinización hospitalaria para el paciente no crítico” [PIH]), adoptado dentro del Sistema Sanitario Público Andaluz.
ObjetivosAnalizar la implementación del PIH en hospitales de tercer nivel del Sistema Sanitario Público Andaluz.
MétodoEstudio multicéntrico descriptivo transversal en 8 hospitales andaluces de tercer nivel, mediante muestreo aleatorizado de pacientes ingresados≥48h, con DM (n=306), en 5 servicios médicos (SM) y 2 quirúrgicos (SQ). La DM tipo 1, DM por trastornos específicos, soporte nutricional artificial, tratamiento esteroideo y gestación fueron criterios de exclusión.
ResultadosSe incluyeron 288 pacientes (varones 62,5%; 70,3±10,3 años; 71,5% SM y 28,5% SQ). El régimen insulínico basal-bolus-corrección se instauró en el 55,9% (IC95%: 50,5–61,2%); 63,1% SM vs. 37,8% SQ (p<0,05). Las alternativas al régimen insulínico basal-bolus-corrección fueron: pautas móviles de insulina rápida (43,7%), dieta (31,3%), antidiabéticos orales (17,2%), premezclas (1,6%) y otras (6,2%). En pacientes tratados previamente con antidiabéticos orales, la dosis de insulina durante el ingreso fue 0,32±0,1UI/kg/día. En pacientes tratados previamente con insulina, la dosis de insulina durante el ingreso se incrementó en un 17% [−13–53] y en pacientes con terapia combinada, en 26,4% [−6–100]. Las pautas correctoras empleadas para<40UI/día y 40–80UI/día fueron las recomendadas en el 72,2% y el 56,7%, respectivamente. Se solicitó HbA1c en el 23,6% (IC95%: 18,8–28,8); 27,7% SM vs. 13,3% SQ (p<0,05).
ConclusionesSon recomendables estrategias para aumentar la implantación del PIH, especialmente en servicios quirúrgicos. Las pautas móviles de insulina rápida son la alternativa más frecuente al régimen insulínico basal-bolus-corrección. Es preciso fomentar la valoración del control metabólico al ingreso.
Diabetes is an increasingly common comorbidity in the hospital setting affecting approximately one fourth of admitted patients.1,2 The association between hyperglycemia and the increased risk of complications, mortality, and hospital costs is well established.3–6 However, despite evidence of the benefits of hyperglycemia control in the hospital, its management can often be improved.7–9 The reasons for deficient control include clinical aspects such as prior poor blood glucose control, the hyperglycemic effect of some drugs, and nutritional support measures, and counterregulatory response to stress. There are also other physician-dependent barriers (tolerance of hypoglycemia due to clinical inertia and fear of hypoglycemia, little familiarity with insulin therapy and the overuse of sliding scale schemes of rapid-acting insulin), which may potentially be changed.2
Aware of this problem, the Diabetes Group of the Andalusian Society of Endocrinology and Nutrition (SAEN) prepared in 2009 a “Hospital insulinization protocol for non-critically ill patients” (HIP) after reviewing the main national2 and international10–12 consensus documents on the management of hyperglycemia in hospitalized patients and intervention studies with subcutaneous insulin regimens.13 Recommendations in the protocol were approved by the consensus of the expert panel of the group. Briefly, the protocol defines its field of application, excluding conditions with specific needs (type 1 DM, secondary DM, artificial nutritional support, steroid treatment, and pregnancy) and recommends a number of actions in the three phases of hospital stay: in the first 24h, during hospitalization, and in planning at discharge. Basic actions recommended during admission include the measurement of HbA1c, the discontinuation of oral antidiabetics (OADs), the start of a scheduled subcutaneous insulinization regimen and the selection of corrective insulin doses adapted to insulin requirements and patient weight. A preparation for discharge, the adaptation of treatment depending on glucose lowering therapy and the degree of control before admission (HbA1c) and on the individual patient profile are recommended. A basal-bolus subcutaneous insulin regimen added to the corrective regimen was defined by the term “basal-bolus regimen-correction” and is at the core of the therapeutic recommendations in the protocol.
The HIP was actively disseminated at the meeting of the Andalusian Society of Endocrinology and Nutrition and through the members of the SAEN Diabetes Group, which took responsibility for its implementation at their reference hospitals. The HIP was also disseminated through triptychs and information posters in paper format and on the website of the SAEN.14 Finally, the HIP was included in the integrated process for the care of diabetes of the Department of Health, which unifies the recommendations for the management of patients with diabetes in the Andalusian public health system (SSPA).15
The purpose of this paper was to assess current compliance in the SSPA with the recommendations of the HIP regarding non-critically ill patients and to identify areas for improvement in its implementation process.
Materials and methodsStudy design and sample size calculationTo address the project objective, a multicenter, descriptive, cross-sectional study was designed and conducted in eight tertiary hospitals from the SSPA. Participating hospitals included five regional hospitals (Hospital Universitario Virgen del Rocío, Hospital Universitario Virgen Macarena, Hospital Universitario Virgen de las Nieves, Hospital Regional Universitario de Málaga, and Hospital Universitario Reina Sofía) and three specialist hospitals (Hospital Universitario Virgen de Valme, Hospital Juan Ramón Jiménez, and Complejo Hospitalario de Jaén). A simple randomized sampling was made of patients admitted with a diagnosis of in-hospital diabetes/hyperglycemia from five medical units (internal medicine, cardiology, gastroenterology, nephrology, and neurology) and two surgical units (general surgery and cardiovascular surgery) from each of the participating hospitals.
For sample size calculation, the expected compliance rate with the HIP was set at 50%. To estimate the HIP compliance rate with 5% precision, an alpha error=0.05, and 5% of non-evaluable patients, 252 patients were needed.
A short description of the “Hospital insulinization protocol for non-critically ill patients”Application scope: The recommendations contained in the HIP apply to the management of hyperglycemia in non-critically ill adult patients (>18 years) admitted to hospital. The HIP identifies clinical conditions where a basal-bolus insulin regimen is warranted, but which may require individualized management in calculation, adjustments and/or administration as prandial and basal insulin. Such clinical conditions include type 1 DM, diabetes due to specific disorders, artificial nutritional support, steroid treatment, and pregnancy, which are therefore excluded from the generic recommendations given in the HIP.
General recommendations: It is recommended that HbA1c be measured at admission, that OADs be discontinued during hospitalization, and that a scheduled insulin regimen with basal and prandial insulin and a supplemental or corrective regimen (basal-bolus-correction or BBC regimen) be started. To calculate the starting insulin dose, three patient groups are distinguished based on hypoglycemic therapy before admission: OADs (started at 0.3–0.5IU/kg/day), treatment with insulin alone (starting with the dose resulting from the total sum of IU/day at home), or combined treatment with insulin and OADs (starting with the total sum of IU/day+20% of the amount calculated). The recommended distribution of the total dose between the basal and prandial components is 50%/50%. Three correction regimens are defined depending on insulin requirements (A: requirements<40IU/day, B: requirements between 40 and 80IU, and C: requirements>80IU). The HIP allows for the possibility of either establishing a complete insulin regimen consisting of the three components (basal insulin, prandial insulin, and correction regimen) in patients being fed, or of maintaining only the basal insulin component and a correction regimen every 4–6h in fasting patients (NPO).
Study inclusion and exclusion criteriaStudy inclusion criteria were: Age18 years, hospital admission time before assessment ≥48h, and diagnosis of in-hospital diabetes/hyperglycemia. A diagnosis of diabetes was made based on the existence of this diagnosis before admission; in patients with no prior diagnosis of diabetes, the current criteria of the American Diabetes Association (ADA) were used.16 Exclusion criteria included the need for intravenous insulinization and those clinical conditions expressly excluded from the application scope of the HIP (type 1 DM, monogenic DM, DM secondary to pancreatic or systemic disease, post-transplant DM, steroid treatment, enteral or parenteral nutrition, and pregnancy).
VariablesThe variables analyzed included the following: the start of the BBC regimen, insulin dose before and during admission (IU/día and UI/g/day), OAD discontinuation, the correction regimen used, and HbA1c request upon admission. To assess the start rate of the BBC regimen, patients receiving all three components and those receiving the components of basal insulin and correction regimen due to the indication of NPO were considered to be in compliance with HIP recommendations.
Statistical analysisQualitative variables are given as percentages. Quantitative variables are given as mean±standard deviation (normal distributions) and as median [interquartile range] (non-normal distributions). The overall compliance rate with the recommendations made in the HIP is given as a percentage (95% confidence interval [95% CI]). A Chi-square test was used for hypothesis testing (a comparison of the degree of compliance of the different recommendations between medical and surgical units).
Ethical issuesThis study was conducted in compliance with ethical standards as set down by the corresponding ethics committees and with the 1975 Declaration of Helsinki. The protocols established by the respective health care centers to access clinical history data have been respected in preparing its publication for research purposes.
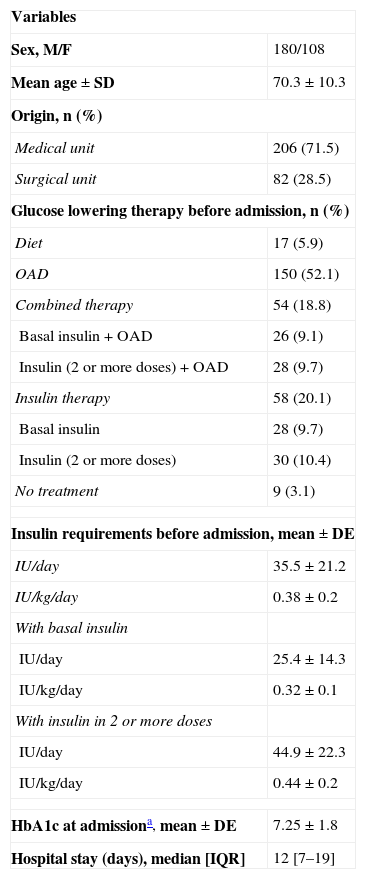
ResultsA total of 306 patients admitted to the above-mentioned medical and surgical units were selected for the study. This represented the recruitment of 25% or more of the patients admitted with a diagnosis of in-hospital diabetes/hyperglycemia. Of these, 288 patients met the inclusion and exclusion criteria and were included in the analysis. Each participating center contributed 12–14% of the total sample. The median hospital stay of the analyzed cohort at the time of assessment was 7 [3–14] days (total hospital stay 12 [7–19] days). Table 1 shows the demographic and clinical characteristics of the sample.
Demographic and clinical characteristics of study patients (n=288).
| Variables | |
| Sex, M/F | 180/108 |
| Mean age±SD | 70.3±10.3 |
| Origin, n (%) | |
| Medical unit | 206 (71.5) |
| Surgical unit | 82 (28.5) |
| Glucose lowering therapy before admission, n (%) | |
| Diet | 17 (5.9) |
| OAD | 150 (52.1) |
| Combined therapy | 54 (18.8) |
| Basal insulin+OAD | 26 (9.1) |
| Insulin (2 or more doses)+OAD | 28 (9.7) |
| Insulin therapy | 58 (20.1) |
| Basal insulin | 28 (9.7) |
| Insulin (2 or more doses) | 30 (10.4) |
| No treatment | 9 (3.1) |
| Insulin requirements before admission, mean±DE | |
| IU/day | 35.5±21.2 |
| IU/kg/day | 0.38±0.2 |
| With basal insulin | |
| IU/day | 25.4±14.3 |
| IU/kg/day | 0.32±0.1 |
| With insulin in 2 or more doses | |
| IU/day | 44.9±22.3 |
| IU/kg/day | 0.44±0.2 |
| HbA1c at admissiona, mean±DE | 7.25±1.8 |
| Hospital stay (days), median [IQR] | 12 [7–19] |
OAD: oral antidiabetic drug; SD: standard deviation; M: male; IQR: interquartile range; F: female; IU: international units.
HbA1c values were available at admission for 68 patients, and HbA1c measurement was therefore required for 23.6% (95% CI: 18.8–28.8%); the proportions of patients with available HbA1c levels were 27.7% (95% CI: 22.4–34.9%) at medical units and 13.4% (95% CI: 6.1–22%) at surgical units (p<0.05 for the comparison of availability of HbA1c between medical and surgical units). OADs were discontinued at admission in 90.3% (95% CI: 84.1–96.3%); no statistically significant differences in the OAD discontinuation rate were found between medical and surgical units.
The scheduled BBC insulin regimen was started in 161 patients, or 55.9% (95% CI: 50.5–61.2%). The BBC regimen was prescribed to 63.1% (95% CI: 57.3–69.9%) of patients admitted to medical units and 37.8% (95% CI: 28–48.7%) of those admitted to surgical units (p<0.05 for the comparison of the application rates of the BBC regimen between medical and surgical units). Alternatives to the BBC regimen are described in Fig. 1.
In patients on the BBC regimen and receiving all three components (basal, prandial, and correction regimen), the proportion of basal compared to total insulin was 50.9±13.8 (%). In patients with OADs before admission, insulin requirements during hospitalization were 0.32±0.1IU/kg/day. In patients on combined therapy before admission, the insulin dose increased by 26.4 [−6–100] (%) during admission as compared to the outpatient insulin dose. In patients on insulin therapy alone before admission, the insulin dose increased by 17 [−13–53] (%) during hospitalization.
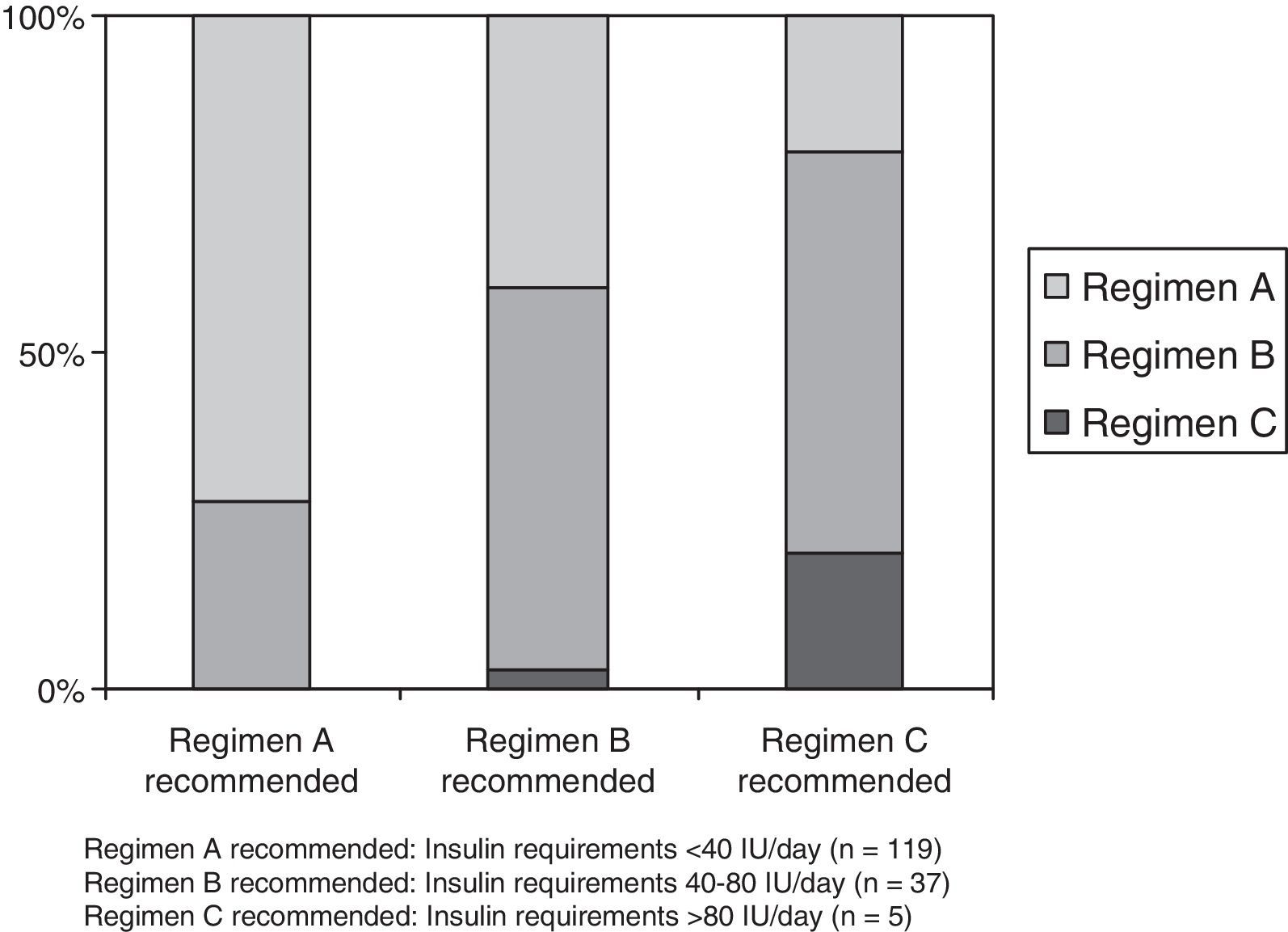
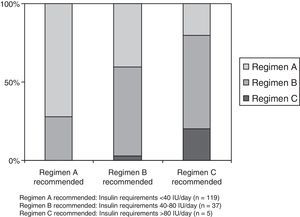
The correction regimen recommended for patients with requirements <40IU/day (regimen A) was prescribed to 86 of 119 patients (72.2%), while the regimen for patients requiring 40–80IU/day (regimen B) was given to 21 of 37 (56.7%), and the regimen for patients with requirements >80IU/day (regimen C) was prescribed to 1 of 5 patients (20%). Fig. 2 illustrates the degree of adaptation of the correction regimen to the recommendations made based on daily insulin requirements.
Percent adaptation of the subcutaneous insulin correction regimen to the recommendations based on daily insulin requirements made in the “Hospital insulinization protocol for non-critically ill patients”. Regimen A recommended: Insulin requirements<40IU/day (n=119). Regimen B recommended: Insulin requirements 40–80IU/day (n=37). Regimen C recommended: Insulin requirements >80IU/day (n=5).
This descriptive study analyzed the degree of compliance with the recommendations made in the HIP prepared by the SAEN in a representative sample of tertiary SSPA hospitals. We discovered that although the use of the BBC regimen was usually adequate in terms of its adaptation to prior treatment, its degree of implementation could be improved, especially in surgical units. Although the HIP expressly recommends the ascertaining of metabolic control before admission through HbA1c values, to our surprise such knowledge was often unavailable.
The association of hyperglycemia and increased morbidity and mortality in hospitalized patients is well established. Although most clinical trials analyze the impact of treatment for hyperglycemia on critically ill patients,17,18 there are sufficient data from observational studies to suggest that glycemic control in non-critical patients in medical and surgical units is also important.1,10,19,20 Deficient control of diabetic patients and lack of action protocols are however often found in the hospital setting and have led to wake-up calls by national and international scientific societies.21,22 The recommendations of the HIP are intended to correct the main potentially modifiable causes that promote inadequate glycemic control during admission, such as clinical inertia, ignorance of prior patient treatment, and the overuse of rapid-acting insulin sliding scales.2,21
The degree of implementation of this protocol was simultaneously analyzed in a sample of SSPA hospitals, including 100% of its regional hospitals, using homogeneous methods. In our study, 55.9% of patients were prescribed a basal-bolus insulin regimen, a proportion higher than that reported in recent studies conducted at national and international university hospitals.9,23,24 Thus, in the survey conducted in 2007 in 44 US hospitals, the proportion of patients receiving some type of basal insulin was only 32%.9 Botella et al. reported, in a cohort of 185 non-critically ill patients in a Spanish hospital, a 34.5% prevalence rate of the use of a scheduled regimen with basal and regular insulin.23 It should also be noted that, unlike in the reported studies, type 1 DM, diabetes caused by specific disorders, artificial nutritional support, and steroid treatment were not considered in this analysis because they are excluded from the HIP. As these are clinical conditions where a basal-bolus regimen is usually indicated and evaluation by endocrinology and nutrition is recommended by the SSPA, we think that the proportion of non-critically ill patients who receive scheduled insulin therapy with basal and prandial components at SSPA hospitals could be higher. No studies prior to the design, dissemination, and implementation of the HIP are available, and quantitative assessment of its impact is therefore not possible. We think, however, that this initiative may have promoted the greater acceptance of the basal-bolus insulin regimen recommended by the main national and international scientific bodies.2,11,25 The results show a more frequent prescription of the regimen in hospitals when compared to the results of studies conducted in centers with similar characteristics.
Although the recommendations contained in the HIP include the measurement of HbA1c at admission, this information was only available in 23.6% of the patients analyzed. No data were found on the frequency of measurement of HbA1c as part of the management of non-critically ill patients with hyperglycemia. Botella et al. reported that HbA1c values were available in 55% of the patients in their cohort, although the design of their study included laboratory data collected during hospitalization and in the six months prior to hospital admission.23 Since HbA1c levels are helpful for adequate diagnosis12 and for deciding on a therapeutic scheme at discharge,2,25,26 the systematic assessment of metabolic control at admission using HbA1c is a significant area for improvement in hospitalized patients.
An additional conclusion of our study is the different degree of application of the HIP in medical and surgical units, seen both in the prescription of the BBC regimen (63.1% vs 37.8% respectively) and in the availability of HbA1c at admission (27.7% vs 13.3% respectively). Data available regarding the management of in-hospital diabetes at surgical units in our environment are limited. Amor et al., in an interventional study to assess the efficacy for glycemic control of a proactive intervention supported by a point-of-care system, reported the use of the basal-bolus regimen in a surgical ward in 21.4% of patients in the phase prior to the evaluated intervention,24 lower than that found in our study. The scheduling of a basal-bolus regimen has not only been shown to be effective and safe for achieving glycemic control goals, but also for decreasing postoperative complications at general surgery units.13,27 An emphasis on adequate dissemination and implementation measures, especially those aimed at surgical units, is therefore a priority.
The use of sliding scale rapid-acting insulin regimens achieves poorer glycemic control as compared to a basal-bolus insulin regimen and is associated with higher postoperative morbidity.13,27 However, their use continues to be unacceptably high.2,11,28 Thus, a study analyzing 44 US centers concluded that 16% of patients with type 1 DM and 35% of patients with type 2 DM pretreated with insulin were receiving treatment with sliding scale rapid-acting insulin regimens during their hospital stay.9 In many of our centers, and in the absence of scheduled insulinization protocols, they represent the standard regimen for the management of type 2 DM.2 Recent studies show that sliding scales account for 40–65% of regimens used in hospitalized patients.9,23 Although no data are available regarding the use of sliding scale rapid-acting insulin regimens at SSPA hospitals before the implementation of the HIP, the percentage use revealed by our study was significantly lower than that estimated for them. Nevertheless, the eradication of sliding scale insulin regimens as standard clinical practice should remain an objective if we want to improve the quality of care for in-hospital diabetes.
The HIP provides basic recommendations on dosage for starting or adapting insulin therapy as a function of outpatient treatment before admission (OADs, insulin, or combined therapy with OADs and insulin). After analyzing insulin requirements during hospitalization, it may be concluded that both mean insulin dose (in insulin-naïve patients) and increase in total daily insulin dose (in patients on combined outpatient therapy) are superimposable on those recommended by the HIP. The HIP also proposes differentiated insulin correcting regimens (regimens A, B, and C), so that if greater daily insulin requirements exist, higher supplemental insulin doses can be prescribed, as happens with recommendations in other protocols. The prescription of the correction regimens used agreed with the recommendations in the HIP in 70.6% of the cases where regimen A was indicated, and decreased to 56.7% of cases where regimen B was prescribed. The proportion of patients in whom the correction regimen C was indicated and prescribed was only 20%, but the low number of patients eligible for this regimen (only five patients in the whole cohort) did not allow us to draw any conclusions. Despite this limitation and taking into account the appropriateness of the recommended A and B regimens, adequate, individualized selection of corrective insulin doses was identified as an area for improvement.
This study did not analyze the factors associated with deficient or incomplete use of the HIP in our environment or with the different implementation of the HIP in medical and surgical departments. Studies conducted with this objective concluded that the barriers to the optimum management of in-hospital hyperglycemia mainly result from the limited knowledge concerning insulin treatment in inpatients.29,30 Educational strategies aimed at correcting this limitation should therefore be designed and implemented. In this regard, the Diabetes Group of SAEN has developed a computer tool that facilitates the programming of the BBC insulin regimen (Insulinator®, v.2.00-Insulinization aid software).14 The group is also developing an initiative to promote the implementation of recommendations at discharge through the design and active dissemination of specific information triptychs with a particular focus on HbA1c testing before admission. This initiative, together with local dissemination and implementation strategies, especially aimed at professionals from surgical units, should promote an increasingly greater compliance with the proposed recommendations. Strategies that propose endocrinological proactive care models, facilitated by new technologies, look extremely interesting. Thus, the implementation of these schemes through point-of-care systems with the remote visualization of capillary blood glucose levels has been shown to increase the use of basal-bolus insulin regimens and to improve glycemic control of hospitalized patients in non-critical areas.24 This could be applicable in our environment.
This study had some limitations. First of all, not all medical and surgical departments from the participating centers were analyzed. Units were selected based on their greater possibility of patient recruitment. Thus, in the selected departments, the prevalence of in-hospital diabetes/hyperglycemia was high and patient stay was usually longer than 48h. On the other hand, other medical units were not included because of their high frequency of steroid prescription and the use of nutritional support measures, which preclude the use of the HIP. Another limitation of our study is that its results only analyzed data related to the implementation of HIP recommendations. It would be interesting to assess the results of HIP implementation in terms of the adaptation of glucose lowering treatment at discharge and the achievement of glycemic control and hypoglycemia rate goals. Multicenter studies including the complication rate during hospitalization, hospital stay and associated costs, thus allowing for the evaluation of HIP efficiency in the SSPA, are also needed.
To sum up, our study shows that although the scheduled BBC insulin regimen is used more frequently than in hospitals with similar characteristics, new strategies should be designed to increase the implementation of the subcutaneous insulinization hospital protocol, especially in surgical departments. Sliding scale rapid-acting insulin regimens continue to be the most common alternative to the insulinization recommended. The main areas for improving care to patients with hyperglycemia during their hospital stay include the promotion of metabolic control assessment upon admission and the replacement of sliding scale regimens by a scheduled insulin regimen.
Conflicts of interestThe authors state that they have no conflicts of interest.
We thank Maria Rosa Alhambra, Rocío Ortega, Pablo Ceballos, Martín López de la Torre, Eulalia Gómez, Diana Aradiel, Francisca Linares, Mercedes Guerrero, María Isabel Fontalba, Rosario Fernández, Maria Lainez, Catalina Díaz, Mariana Tomé, Maria Victoria Cózar, and Virginia Hernando for their collaboration in coordination and/or clinical data collection in the reported study.
We would like to thank all members of the Diabetes Group of SAEN for their active participation in the preparation, dissemination, and implementation of the “Hospital insulinization protocol for non-critically ill patients”. This project would not have been possible without them.
Please cite this article as: Martínez-Brocca MA, Morales C, Rodríguez-Ortega P, González-Aguilera B, Montes C, Colomo N, et al. Implementación del protocolo hospitalario de insulinización subcutánea para pacientes no críticos en hospitales andaluces de tercer nivel. Endocrinol Nutr. 2015;62:64–71.