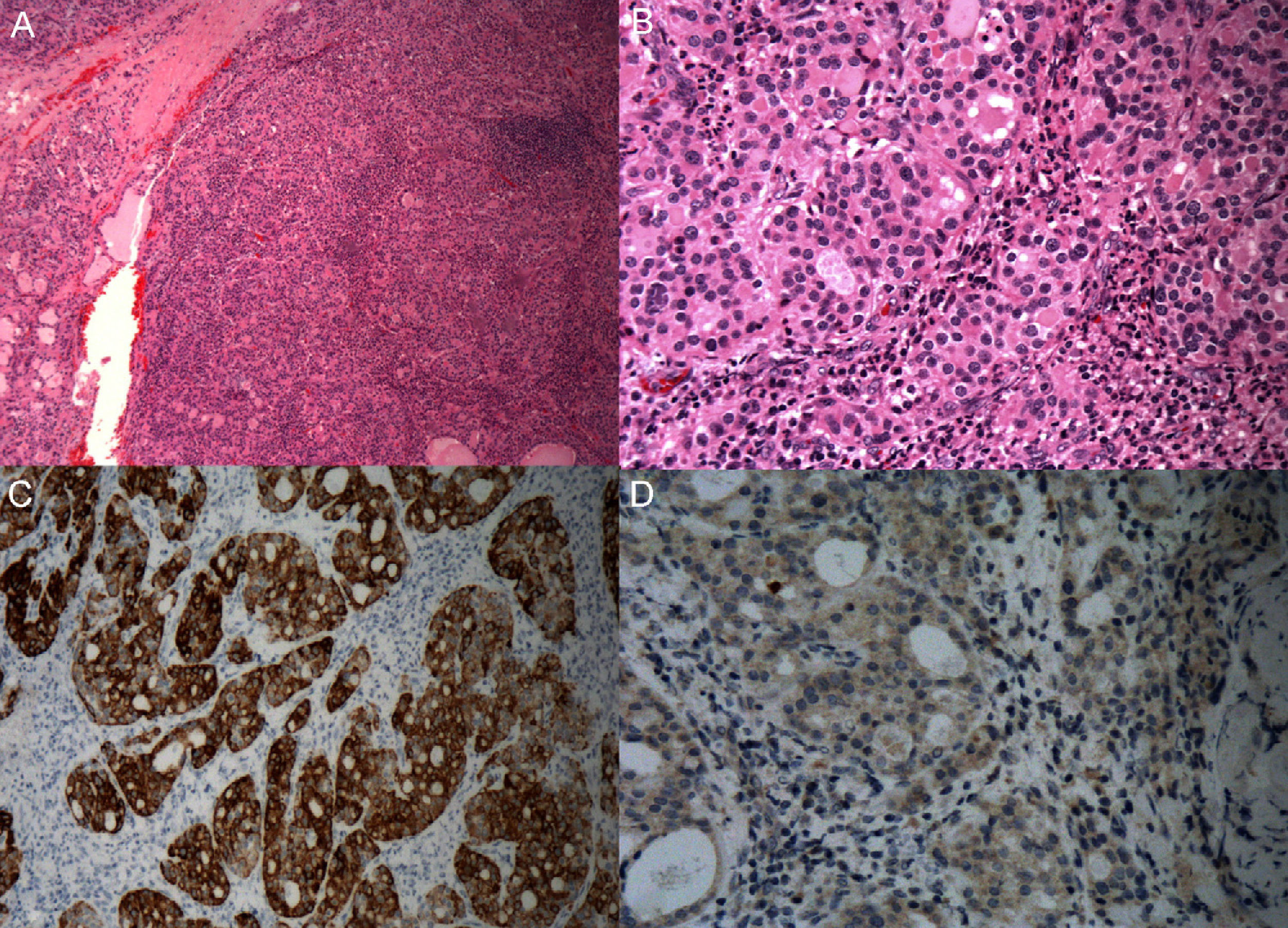
This was a 70-year-old female patient with a history of high blood pressure and breast carcinoma operated on 20 years before and in remission. Magnetic resonance imaging of the cervical spine incidentally revealed a thyroid nodule in the right thyroid lobe (RTL) that displaced the trachea. The patient was therefore referred to an endocrinology outpatient clinic for assessment. Thyroid ultrasonography showed multinodular goiter with a predominant nodule 2.2cm at largest diameter in RTL, apparently nonmalignant, and a 1.8cm hypoechoic nodule in the lower pole of RTL which was possibly an intrathyroid parathyroid gland. No suspect lymph nodes were seen. Laboratory test results included: calcium, 11.6mg/dL (8.5–10.5); ionic calcium, 5.69mg/dL (4.10–5.30); phosphorus, 2.71mg/dL (2.5–4.9); TSH, 1.39μU/mL (0.55–4.78); FT4, 1.14ng/dL (0.9–1.7); PTH, 133pg/mL (11–80); vitamin D, 28ng/mL (20–55). Based on the findings suggesting primary hyperparathyroidism, a parathyroid scan was performed before surgery and this confirmed the presence of a possible right lower parathyroid adenoma. Bone densitometry showed osteopenia in the lumbar spine and femoral neck. FNA of the right thyroid nodule was requested, but was inadequate for diagnosis. Resection of the right lower parathyroid adenoma and the thyroid nodule in RTL in one and the same surgical procedure was decided upon. The patient underwent right hemithyroidectomy and right lower parathyroidectomy. Pathological analysis of the thyroid nodule detected a nodular, solid neoplasm with infiltrating margins, with a growth pattern in hyperchromatic nests of epithelial cells with enlarged nuclei, as well as pseudofollicular structures with contents of a colloid appearance. Immunohistochemistry was positive for type IV collagen and cytokeratin 20, and negative for TTF-1, calcitonin, thyroglobulin, and PTH, which ruled out a thyroid and parathyroid origin of the tumor. It was also negative for CEA, chromogranin A, and synaptophysin, which excluded a neuroendocrine lineage. After ruling out the most likely origin based on the location, and based on the characteristics of the material, the tumor was categorized as a salivary adenocarcinoma not otherwise specified. P53 was negative (Fig. 1). A 1.7cm intrathyroid parathyroid adenoma was also found. The specimen sent as parathyroid tissue turned out to be a lymph node negative for malignancy. The patient was referred to the otolaryngology department, where a primary tumor in an orthotopic salivary gland was ruled out. PET-CT showed no uptake at salivary gland level or local or distant involvement. The patient has returned to the endocrinology outpatient clinic for regular monitoring, and one year after surgery no tumor relapse was seen in imaging tests. Normal PTH (31.7–66.5pg/mL) and plasma calcium levels (9.6–10.1) were found.
The presence of ectopic salivary tissue has been documented in areas such as the brain, neck, jaw, and ear. On the other hand parathyroid, thymic, adipose, striated muscle, and cartilaginous ectopic tissue have been found in the thyroid gland.1
Intrathyroid salivary tissue is an exceptional finding. Benign intrathyroid glandular tissue has been reported, but this is the first documented case of intrathyroid salivary gland carcinoma.
This finding could be due to an embryological alteration of the last branchial arch (LBA). The fourth pharyngeal pouch (the fifth, according to some authors) is the origin of the LBA in its ventral region. During the seventh week of pregnancy, the LBA becomes enclosed in the upper and middle part of the thyroid lobes, providing parafollicular or C cells.2 LBA persistence in adults is related to the appearance of solid cell nests (SCNs), which are groupings of epithelial lineage of endodermal origin and occur in clusters among follicular cells such as the ones detected in the reported case. SCNs represent a diagnostic challenge because they may be confused with squamous metaplasia, squamous papillary carcinoma, medullary carcinoma, or C-cell hyperplasia. Immunohistochemistry is indispensable to differentiate them from these conditions. In this regard, thyroglobulin, PTH, and TTF-1 are negative, because they are not thyroid or parathyroid cells. The typical immunohistochemical profile of SCNs is positive for CEA and cytokeratins. Our sample was positive for cytokeratin 20. Galectin-3 and p63 are more specific for identification.3,4 The prevalence of SCNs in adults has been estimated at 1.3%.5
It has been suggested that they may be the origin of follicular and C cells, and also of intrathyroid ectopic tissue of different cell lineages and some thyroid tumors.4,5 They have also been related to the appearance of thymic remnants and ectopic cartilage in the neck.3
Adenocarcinoma not otherwise specified accounts for 5.3% of malignant salivary gland tumors. Peak occurrence is seen at ages ranging from 40 to 60 years, and is more common in the major salivary glands.6 Classification is based on the TNM staging system of the International Union against Cancer.7 MRI and CT are the imaging tests of choice.
Surgery is the primary treatment, irrespective of tumor location. Wide resection, with free surgical margins, has been associated with longer survival. If size is greater than T1, more aggressive resection is recommended. Lymphadenectomy should be performed when there is clinical or radiographic evidence of nodal involvement, and for prophylactic purposes when greater than T2 or stage II.6
In some series, the use of adjuvant radiotherapy has been shown to decrease recurrence and to increase survival. The use of radiotherapy is recommended based on tumor size, free margins, locoregional invasion, and histological type. Tumors less than 4cm in size have a better prognosis, with less locoregional invasion and metastasis. Because of this, it is advised that tumors greater than 4cm should be given adjuvant radiotherapy. Chemotherapy using different drugs has achieved variable results, and has therefore no relevant role.8
The main prognostic factor is the TNM stage, together with surgical resection. Sex, grade, and location may have an influence to a lesser extent.6,8
Conflicts of interestNone of the authors has conflicts of interest.
Please cite this article as: Gómez Rodríguez S, Guijarro de Armas G, Modroño Móstoles N, Pérez Blanco C, Martín Hita AM. Adenocarcinoma de tipo glándula salivar y adenoma paratiroideo intratiroideos en paciente con bocio multinodular. Endocrinol Nutr. 2016;63:304–306.