Acute suppurative thyroiditis (AST) is an uncommon, potentially serious disease occurring mainly in children. The low prevalence of thyroid abscess is related to thyroid gland resistance to infection due to its fibrous capsule, high blood perfusion, high iodine contents, and significant lymphatic drainage, and to anatomical separation of the gland from the airway.1
AST may arise from hematogenous or lymphatic dissemination, continuity from adjacent organs, or direct inoculation after fine needle aspiration (FNA).2 The predisposing factors vary depending on age at presentation. In children, the most common predisposing factor is a pyriform sinus fistula (PSF), which is due to the abnormal development of the third or fourth branchial arch. The condition occurs on the left side in 87–95% of cases. This is explained by the asymmetry of the fourth branchial arch.3,4 PSF is uncommon in adults, in whom other factors such as prior thyroid disease (Hashimoto's thyroiditis, differentiated thyroid cancer, multinodular goiter) and immunosuppression, which promotes in turn infection by uncommon microorganisms, are more relevant.5
We report the case of a 17-year-old female patient with a history of anorexia nervosa who attended the emergency room for fever, pain in the anterior aspect of the neck, and increased size of the left thyroid space. Subacute thyroiditis was clinically suspected, and anti-inflammatory treatment (ibuprofen 600mg/8h) was started. Six days later the patient returned to the emergency room reporting no improvement. Prednisone (30mg/24h) was therefore added in a tapering scheme, and the patient was referred to the endocrinology department due to the persistence of the condition.
Physical examination revealed left thyroid lobe enlargement with pain and a palpated mass and increased temperature.
Laboratory tests results included: leukocytosis (WBC: 13,500mm–3, with 79.3% neutrophils) with elevated acute phase reactants (C-reactive protein: 108.40mg/L) (range: 0.1–10.0) and ESR: 122.00mm (range: 0.0–25.0) with normal thyroid function (TSH: 1.97μIU/mL) (range: 0.35–5.0), free T4 1.40ng/dL (range: 0.7–1.98) and free T3 2.54pg/mL (range: 2.3–4.2) and negative thyroid autoimmunity.
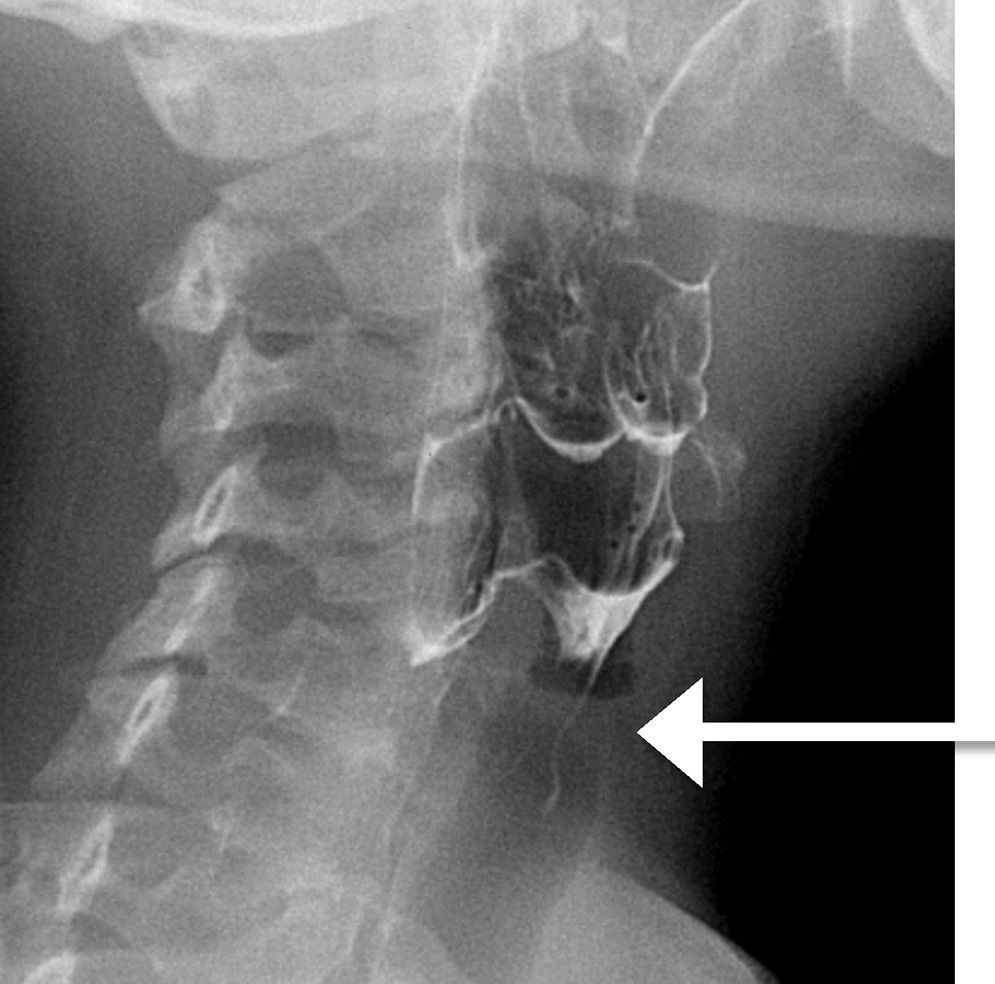
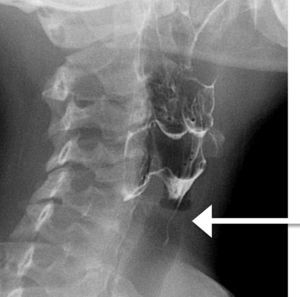
A thyroid ultrasound examination showed three hypoechogenic collections suggesting thyroid abscess. A culture of purulent material collected by FNA revealed the presence of penicillin-sensitive Lactococcus lactis. Blood cultures were negative. Barium esophagogram revealed a fistula in the left pyriform sinus which ended close to the thyroid gland (Fig. 1) and was subsequently confirmed in computed tomography of the neck.
The patient was treated with amoxicillin 2g/6h by the intravenous route for two weeks, resulting in the disappearance of pain and fever and progressive thyroid size decrease. Surgical drainage was therefore not considered. After resolution of the infection, the patient underwent elective exploratory cervicotomy, which could not show the fistulous tract, but allowed for the resection of the upper third of the left thyroid lobe. Pathological examination showed fibrosis and peripheral vascular congestion in thyroid parenchyma.
The patient has remained symptom-free, with preserved thyroid function and no recurrent thyroid infection, during 10 months of follow-up.
A diagnosis of AST should be suspected in patients with sudden, severe pain in the anterior neck which worsens on hyperextension, associated with an increased size of the thyroid space. Erythema and increased local temperature, as well as fever, dysphagia, or dysphonia, may also be found.1 Laboratory tests usually show leukocytosis and increased levels of acute phase reactants. Thyroid function is normal in 93% of cases.6
Thyroid ultrasound allows the thyroid abscess to be visualized, revealing it as a heterogeneous and hypoechoic lesion. As regards the diagnosis of PSF, laryngoscopy is considered by some authors to be the imaging procedure of choice.1 Other authors, however, think that a barium esophagogram or a CT scan “under trumpet maneuver”, i.e. using air as a contrast agent, represent the best procedures.7 These procedures provide the best results when performed at least 15 days after the resolution of the acute condition because the presence of the abscess may obliterate the fistula tract and cause a false negative result.4 Active search for PSF is mandatory in children with recurrent AST and recommended in all other cases.
Microbiological diagnosis is usually made based on the culture of material collected by FNA from the abscess. AST is usually caused by aerobic bacteria,1 but cases due to other microorganisms such as fungi or mycobacteria have also been reported.8 In our patient, the pathogen isolated from culture was Lactococcus lactis, which has never been reported to date as a microorganism responsible for thyroid abscess. It is a Gram-positive, facultative anaerobic coccus which is found as a part of human saprophytic flora and rarely causes disease. In a recent article, only 20 cases of abscesses related with this pathogen occurring in various locations (brain, liver, endocardium, lung) were reported.9 The most relevant risk factor for the infection included tooth decay, immunosuppression, and the consumption of non-pasteurized milk. None of these factors were found in our patient. As this is a poorly virulent microorganism that colonizes the gastrointestinal tract, it cannot be completely ruled out that it is a contaminant. However, there are reasons for considering it to be a true pathogen, including the fact that abscesses have been reported in other locations, that this was the only microorganism isolated, and that the sample was taken by percutaneous puncture, rather than from the aerodigestive tract.
Although it cannot be ruled out that vomiting related to the anorexia nervosa suffered by the patient could have facilitated the passage of food remains through the pre-existing fistula tract, this appears unlikely, as the patient denied any purgative behavior at that time. In addition, recurrent acute tonsillitis and retropharyngeal abscesses have been reported as complications of anorexia nervosa,10 but there is no evidence in the literature relating AST and eating disorders.
AST should be treated early with intravenous broad spectrum antibiotic therapy adequately covering Staphylococcus aureus and Streptococcus pyogenes.1 Surgical drainage of the abscess should be performed when a fluctuating abscess visible in the ultrasound examination exists. In patients in whom PSF is found, the fistula should be closed to prevent recurrence.6
In conclusion, it should be noted that this case was unique not only because AST is an uncommon condition in immunocompetent adults, but because it was caused by Lactococcus lactis, a microorganism which rarely causes disease.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Campos R, Pérez B, Armengod L, Múñez E, Ramos A. Absceso tiroideo por Lactococcus lactis en paciente inmunocompetente. Endocrinol Nutr. 2015;62:204–206.