Amyloidosis is an uncommon syndrome consisting of a number of disorders having in common an extracellular deposit of fibrillary proteins. This results in functional and structural changes in the affected organs, depending on deposit location and severity.
Amyloid infiltration of the thyroid gland may occur in 50% and up to 80% of patients with primary and secondary amyloidosis, respectively. Amyloid goiter (AG) is a true rarity, usually found associated to secondary amyloidosis. AG may require surgical excision, usually because of compressive symptoms.
We report the case of a patient with a big AG occurring in the course of a secondary amyloidosis associated to polyarticular onset juvenile idiopathic arthritis who underwent total thyroidectomy. Current literature is reviewed, an attempt is made to provide action guidelines, and some surgical considerations on this rare condition are given.
La amiloidosis es un síndrome poco frecuente, constituido por un conjunto de trastornos que tienen en común el depósito extracelular de proteínas fibrilares. De ello resultan alteraciones funcionales y estructurales de los órganos afectados, dependientes de la localización e intensidad del depósito.
La infiltración amiloide del tiroides puede verse en el 50% de la amiloidosis primaria y hasta en el 80% de la forma secundaria. El bocio amiloide (BA) es una verdadera rareza, habitualmente asociado a la forma secundaria. El BA puede tener indicación quirúrgica, generalmente justificada por problemas compresivos.
Comunicamos el caso de un paciente con un gran BA en el curso de una amiloidosis secundaria asociada a una artritis idiopática juvenil de inicio poliarticular, al que se le practicó una tiroidectomía total. Revisamos la literatura, intentando aportar pautas de actuación y algunas consideraciones quirúrgicas sobre esta rara afección.
Amyloidosis is an uncommon syndrome consisting of a number of disorders which have in common the extracellular deposition of fibrillary proteins. This results in functional and structural changes in the involved organs depending on deposit location and severity. Deposits have abundant sugars that provide starch-like staining characteristics, hence the term amyloid coined by Virchow in the 19th century. The staining of deposits with Congo red and typical “apple-green” birefringence when examined under polarized light microscopy is essential for diagnosis.
The cause of amyloid material production and deposition in tissue is unknown and lies in a complex disorder due to poor protein folding.1
Amyloid infiltration of the thyroid gland may occur in 50% and in up to 80% of cases of primary and secondary amyloidosis, respectively, usually in diffuse and mild form and often incidentally at autopsy. Amyloid goiter (AG) is a true rarity, and is usually associated with secondary amyloid.2,3
AG may require surgery, usually because of compression problems. Reports of surgery for AG are few and are limited to isolated cases or very small series.
We report the case of a patient with a large AG occurring in the setting of secondary amyloidosis associated with polyarticular onset idiopathic juvenile arthritis who underwent total thyroidectomy. A literature review is made, and an attempt is made to give action guidelines and some surgical considerations regarding this rare condition.
Case reportWe report the case of a 33-year-old male diagnosed with polyarticular onset idiopathic juvenile arthritis at two years of age. He received at different points in time treatment with low dose corticosteroids, methotrexate, and infliximab, which was discontinued due to associated complications.
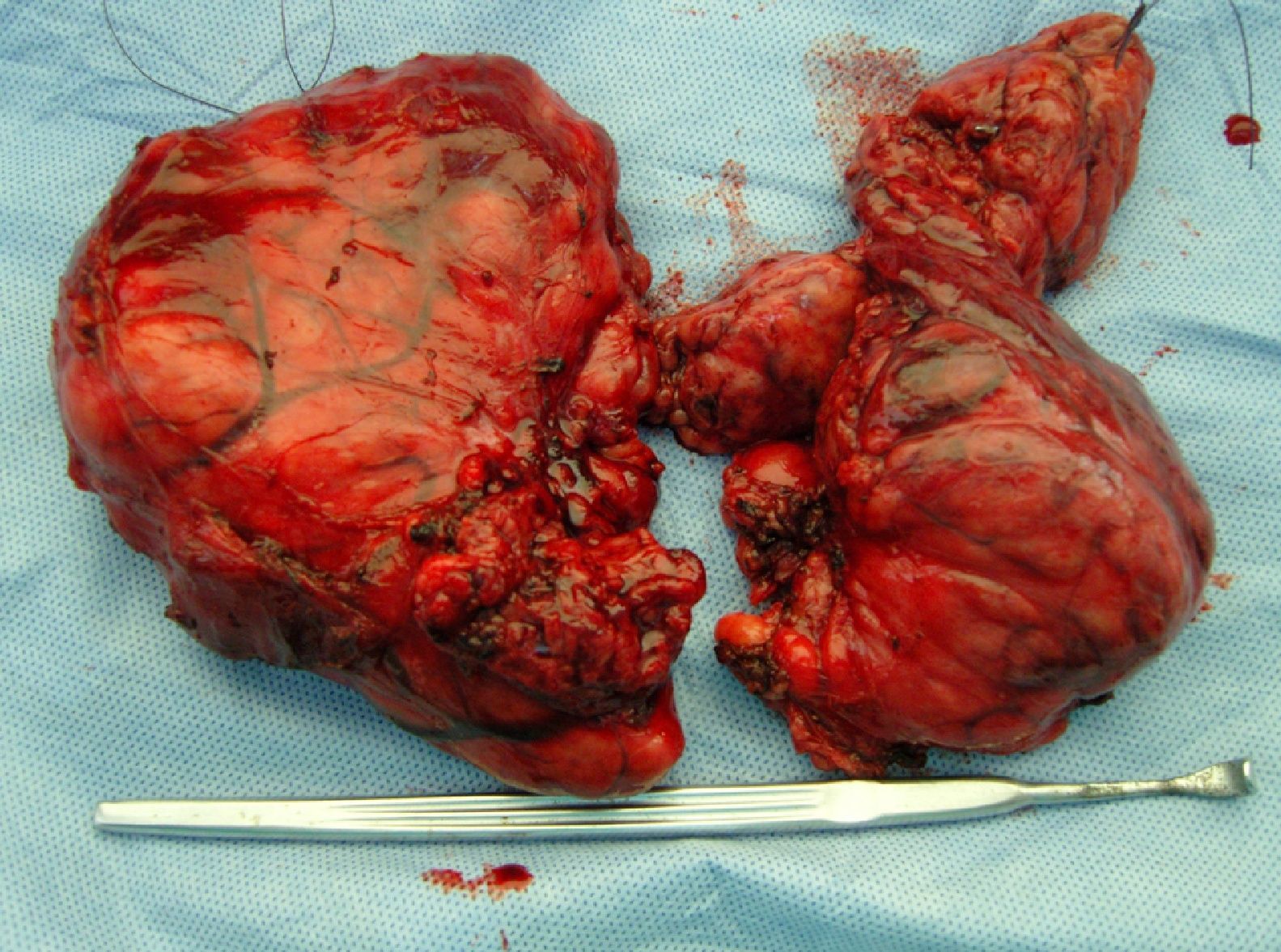
The patient had had a goiter for the previous 7 or 8 years which had enlarged considerably in the previous twelve months. The condition caused no thyroid dysfunction symptoms, only a sensation of cervical tightness (Fig. 1).
Clinical examination revealed moderate exophthalmos, a large goiter mainly affecting the right lobe with nodular surface, significant laterocervical and retrosternal extension, and cutaneous venous network, suggesting superior vena cava syndrome.
Laboratory test results included: TSH 0.003μIU/mL (0.350–4.950); free T4 1.520ng/dL (0.700–1.480); free T3 2.30pg/mL (1.71–4.53); negative antimicrosomal antibodies; and anti-thyroglobulin antibodies 598μL/mL. Other findings included positive rheumatoid factor (54.9IU/mL), elevated acute phase reactants with ESR 97mm/1h and CRP 87.7mg/L, and a 24-h protein level of 0.99g with no microhematuria or casts in urinary sediment.
A thyroid scan (99mTc) showed a large increase in thyroid size and irregular isotope distribution, with multiple normal and low uptake areas.
A CT scan of the neck and chest showed thyroid enlargement with decreased density and asymmetrical growth, particularly in the right lobe. Retropharyngeal extension and the airway was engulfed, displaced, and molded; nonspecific submaxillary glands (Fig. 2).
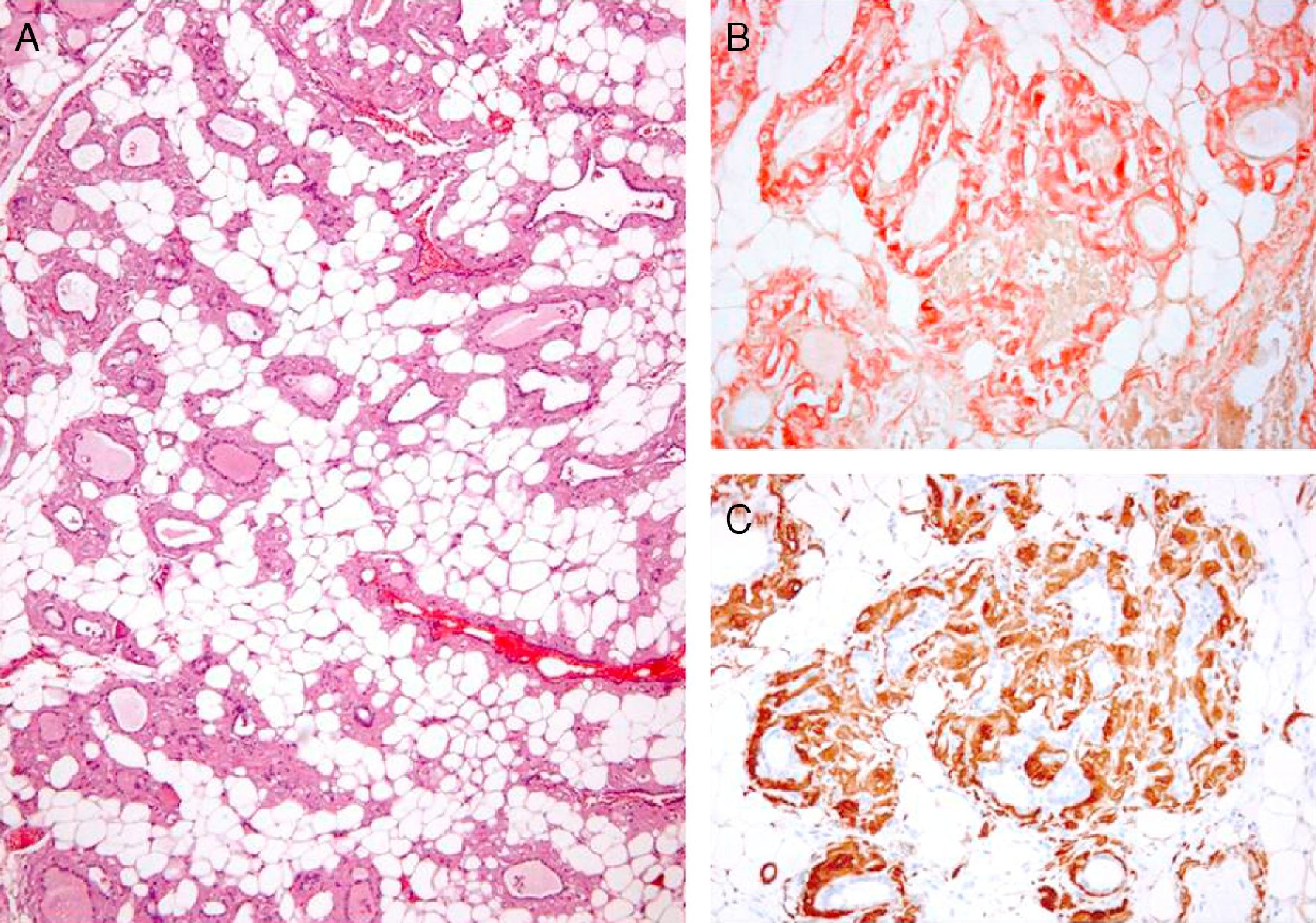
Fine needle aspiration of the right cervical mass demonstrated follicular cells of macrofollicular pattern with no atypia; an amorphous material of hyaline appearance strongly stained with Congo red and birefringent under polarized light; and abundant mature adipose tissue.
During surgery, intubation caused no complications. We found the following: transverse cervicotomy and section of prethyroid muscles on the right side; Large goiter, mainly at the expense of the right lobe, with retrosternal and retropharyngeal components; Lipomatous appearance, nodular surface with no dominant lesion, friable, easily bleeding, and with clear signs of venous congestion; Total thyroidectomy with identification of both recurrent nerves and three parathyroid glands; Complex surgery with diffuse, difficult to control bleeding; transfusion was not required; and Uneventful postoperative course.
Pathological report: right lobe measuring 12cm×9cm×5cm and left lobe 10cm×7.3cm×4cm in size; total gland weight, 408g (right lobe, 278g). We found a lobulated surface, hard consistency, and yellowish and slightly lobulated tissue on sectioning (Fig. 3).
Both lobes had similar histological characteristics, with a total loss of normal architecture and very extensive diffuse infiltration by mature adipose tissue with no cytological atypia. Thyroid follicles, found in a decreased number, were of variable size, distorted, and surrounded by amorphous, cell-free, and eosinophilic material, which was also seen in the vascular walls. This material stained with the Congo red procedure, showing greenish birefringency under polarized light and intense immunostaining for amyloid protein AA (Fig. 4).
DiscussionAmyloidosis is a disease of unknown etiology comprising a group of different conditions. It is characterized by an extracellular deposition in tissue of protein with an insoluble fibrillary structure, called amyloid, of an amount which is sufficient to impair the normal structure and functioning of the affected tissue or organ. This structure stains with Congo red and shows a characteristic greenish hue under polarized light.
The condition is highly uncommon, with an incidence in the US of eight cases per million population/year and a prevalence of five to 13 cases per million population/year.4
A distinction has traditionally been made between primary amyloidosis, with no associated disease, except for myeloma, and secondary amyloidosis, in which a relationship exists with long-standing infectious (tuberculosis, chronic osteomyelitis, bronchiectasis) or inflammatory (rheumatoid arthritis, ankylosing spondylitis, Crohn's disease, Sjögren's syndrome) diseases.2,5–7 There are other even less common forms, such as familial or hereditary amyloidosis linked to Mediterranean fever, senile amyloidosis, or amyloidosis in patients on hemodialysis.8
The current classification of amyloidosis is biochemical, based on the type of fibril accumulated and its origin. Three main types are distinguished: amyloidosis AL, linked to primary amyloidosis, where amyloid consists of light chains of immunoglobulins; amyloidosis AA, associated with the secondary form and with serum protein A (an acute phase reactant synthesized in excess in the liver) forming part of amyloid; and amyloidosis AF, related to a familial polyneuropathy and whose most common form is caused by a mutation in transthyretin, also known as prealbumin.8,9 In our case, immunostaining for amyloid protein AA was consistent with secondary amyloidosis.
The clinical manifestations of amyloidosis are diverse, nonspecific, and often masked by the causative disease (secondary), and depend on the intensity of the deposits and on the organs and structures involved. Renal involvement is virtually constant, and the liver, heart, joints, nervous system, skin, gastrointestinal tract, and adrenal glands may also be affected.4,9,10
Amyloid deposition in the thyroid gland is common, occurring in 20–50% of cases of primary amyloidosis and in up to 80% of cases of secondary amyloidosis. It causes no clinical signs and symptoms and is often detected at autopsy. By contrast, AG, defined by von Eiselberg in 1904, is highly uncommon, is usually euthyroid, and may cause compressive symptoms in neck structures because of its size. The literature references on AG are very scant and are limited to isolated cases or very small series. The estimated number of reported cases range from 200 to 250.3,6,11,12 Goiter is exceptional in primary amyloidosis (0.04), and when clinically apparent, it occurs associated with its secondary form.
AG is characterized by a relatively rapid growth, from between a few months to one year, and causes neck compression symptoms (dysphonia, dysphagia, difficult breathing) often suggesting a preoperative diagnosis of thyroid cancer or thyroiditis. The condition may also be difficult to diagnose for pathologists, because amyloid deposits are found in medullary and follicular thyroid carcinoma, and areas of focal thyroiditis are seen in amyloidosis.2,12,13
Thyroid function is usually unchanged, despite the fact that diffuse thyroid involvement by the amyloid deposit would seem to suggest a high probability of hypothyroidism. Hypothyroidism and hyperthyroidism are reported in some cases, but the mechanisms of dysfunction are not clear. Thyroiditis, or even Graves’ disease, are sometimes the underlying cause of these dysfunctions.2,6,14 Our patient had hyperthyroidism and moderate exophthalmos, clinically suggesting Graves’ disease.
Although AG is rare, it is a well established condition that should be differentiated from other more common types of goiter and from the forms of amyloidosis that may cause thyroid deposits. This requires a high index of clinical suspicion.
Amyloidosis is a progressive disease for which no specific treatment exists and it has a gloomy prognosis in which the main causes of death include renal failure, infection, and cardiac arrhythmia and heart failure. Primary amyloidosis is particularly severe. In secondary amyloidosis, a better result may be achieved in some cases with adequate treatment of the associated disease. In this regard, biological drugs have a promising role to play.
As to whether or not surgery should be performed for any amyloid goiter, the following should be taken into consideration:
- 1.
An adequate preoperative diagnosis of the type of goiter.
- 2.
A surgical indication based mainly on the compressive symptoms caused by the condition.
- 3.
Screening for thyroid cancer.
- 4.
The determination of the type of amyloidosis and its prognosis.
Its clinical presentation as a large goiter of relatively rapid growth, sometimes nodular, with areas of heterogeneous consistency and neck compression symptoms will suggest an anaplastic or medullary thyroid cancer as the first possibility. The differentiation of these two conditions is essential and has a great influence on the clinical suspicion index. An associated inflammatory or infectious disease or the finding of proteinuria suggesting nephrotic syndrome will suggest amyloid goiter, while high calcitonin levels or a diagnosis of MEN will suggest a medullary carcinoma.
The widespread use of fine needle aspiration for thyroid conditions may allow for preoperative diagnosis of AG by identifying the presence of amyloid material and adipose tissue in the absence of malignant cells. The literature references on the subject are scant and there is a diagnostic problem. The availability of an experienced pathologist is therefore essential.12,13,15 Many patients undergo surgery without an adequate preoperative diagnosis, most often because of a suspected colloid goiter with compressive symptoms, with or without suspected cancer. Although the indication for surgery in AG is usually based on compressive symptoms, it should not be forgotten that a final diagnosis of AG is histological, and the presence of thyroid cancer cannot always be ruled out based on fine needle aspiration. In the case reported, both clinical suspicion and information provided by cytology allowed for a preoperative diagnosis of AG.
Imaging tests provide information similar to that obtained from the study of goiters and thyroid nodules in general. In fact, CT is more warranted in AG in order to ascertain the relation of a large neck mass, usually asymptomatic, with neck structures. It may also provide information, combined with ultrasound, on a diffuse decrease in parenchymal density suggesting a lipomatous structure that contributes to the diagnosis, as occurred in our case.
Once a preoperative diagnosis of AG is established or suspected, the indication for surgery should be based on consideration of the following elements:
- •
The presence of compressive symptoms.
- •
The morbidity of surgery.
- •
The type of amyloidosis.
- •
The prognosis of amyloid disease.
Compressive symptoms are often the reason for surgery,16 and although hyperfunction may exist, as occurred in our case, we are not aware of any case where surgery was indicated for this reason. It is also important to know the type of amyloidosis, its prognosis, and the surgical risk derived from its course (renal failure, heart failure, etc.), as well as the risk of any associated disease. Good clinical judgment in the management of these factors is essential in order to achieve the maximum benefits in these patients.
Surgery is complex, and not free from complications. The main difficulties include the large size of AGs (the highest weight reported is 530g, and the AG of our patient weighed 408g),17 the poor delimitation from other neck structures, which makes the preservation of recurrent nerves and parathyroid glands extremely difficult, the fragility of thyroid parenchyma, and profuse, difficult to control diffuse bleeding. In agreement with other authors, surgery was considered “complex” in our case for all these reasons.18,19 These technical considerations should also influence any indication of surgery for an AG.
Our patient was diagnosed with idiopathic juvenile polyarthritis which had started 31 years before and was under good clinical control and allowed him an acceptable quality of life, and also with secondary amyloidosis (positive immunostaining for protein AA) where thyroid pathology was outstanding. The recent occurrence of proteinuria appeared to suggest AG associated with secondary amyloidosis with renal involvement. The patient had a large goiter, which had markedly grown in the previous months and compromised important neck structures in imaging studies, and non-relevant but evident compressive symptoms (venous hypertension). Surgery was indicated, and total thyroidectomy was considered to be warranted because we were dealing with a young patient with an acceptable prognosis of both amyloidosis and its associated chronic polyarthritis and because a team of professionals experienced in thyroid surgery was available. The decision to perform surgery was not influenced by the occurrence of hyperthyroidism in the preceding few months.
Some authors suggest that a good response to treatment for primary amyloidosis with dexamethasone may decrease goiter size and improve thyroid dysfunction, and that surgery should be subordinated to this possibility.20,21 The new therapies with monoclonal antibodies appear to be promising as regards improving the prognosis of amyloidosis. Further studies are needed in this regard, and also to establish the potential relationship between treatment for amyloidosis and AG response.9,20
Our efforts should be aimed at making a preoperative diagnosis of AG and at establishing the type of amyloidosis and its severity before surgery is indicated. This may be done based on clinical signs, fine needle aspiration, biopsy, immunological laboratory measurements, and imaging studies. A preoperative diagnosis is essential if we wish to perform surgery where there is an adequate risk/benefit relationship in patients in whom prognosis is mainly based on the characteristics and severity of amyloidosis.11,12,16
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: García Villanueva A, et al. Consideraciones quirúrgicas del bocio amiloide. Endocrinol Nutr. 2013;60:254–9.