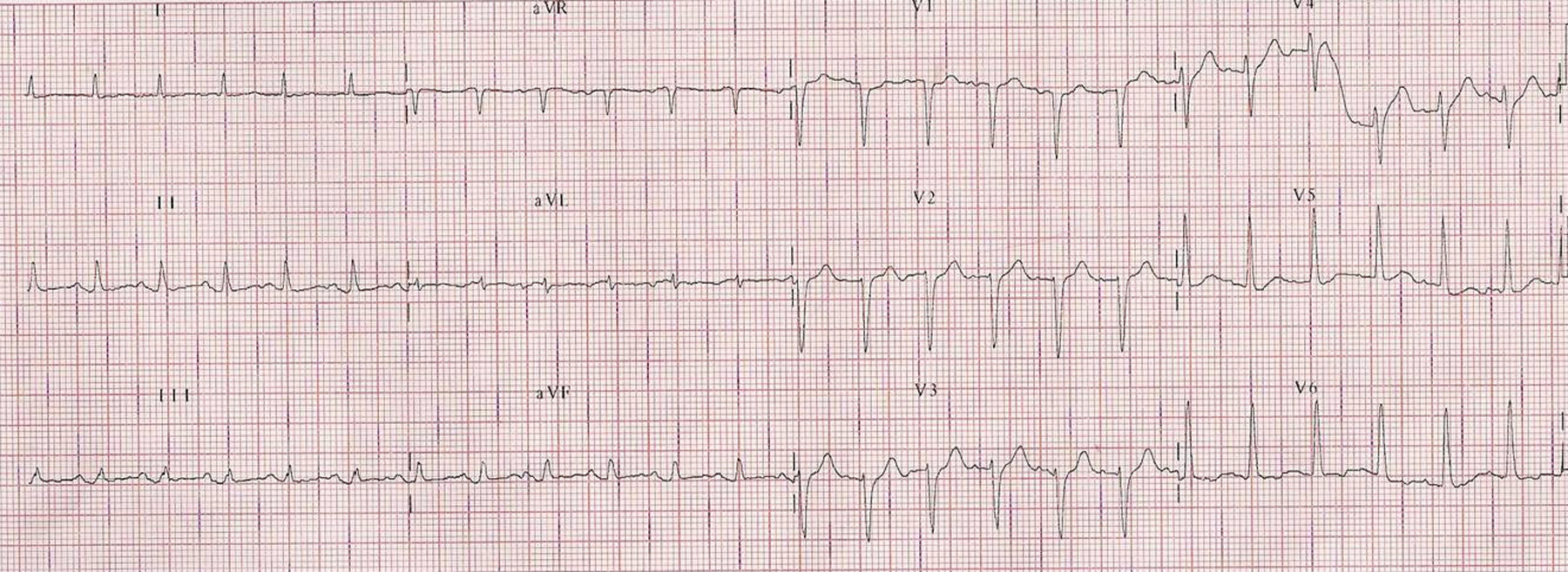
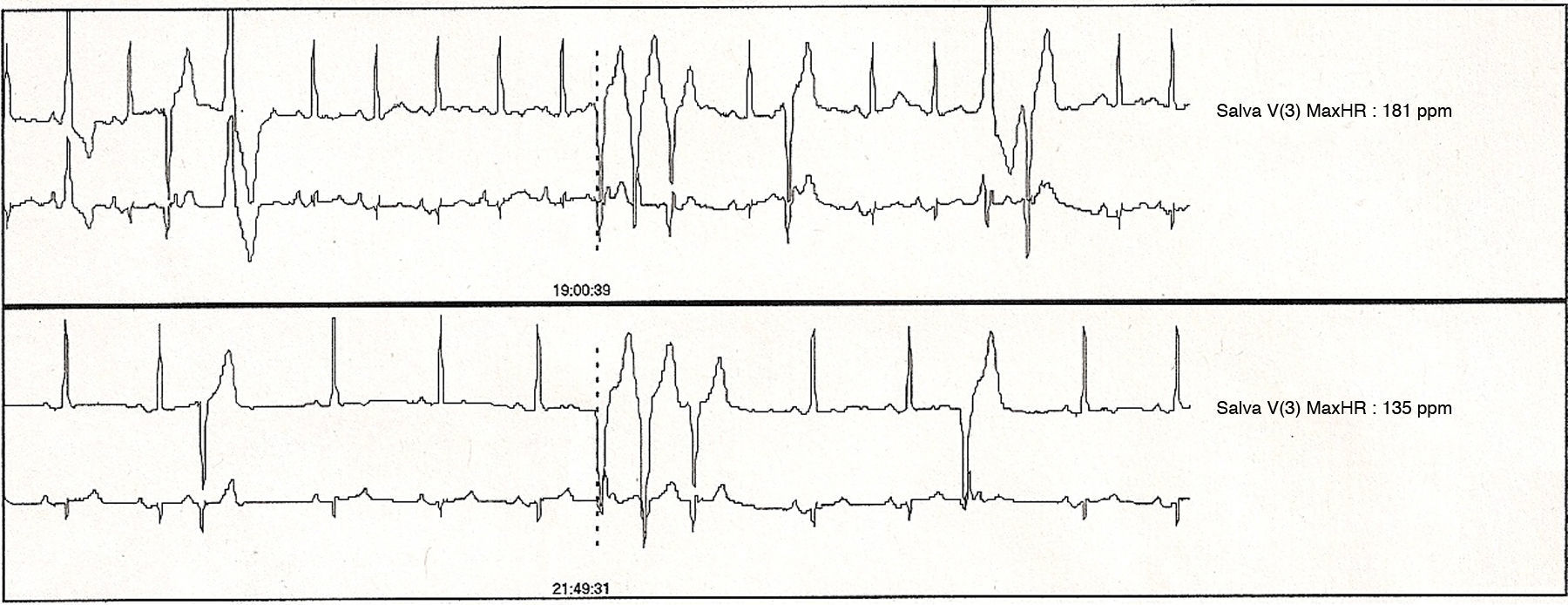
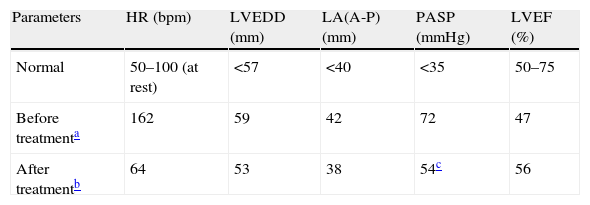
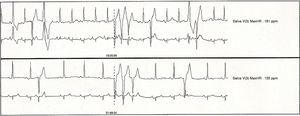
A 65-year-old male with a history of fibrothorax of tuberculous origin and chronic obstructive pulmonary diseases with moderate pulmonary artery hypertension was referred to the cardiology department due to frequent palpitations. The patient had stopped smoking 15 years before and had no other toxic habits or cardiovascular risk factors. His family history included a sister with euthyroid goiter, but no other cases of hyperthyroidism. Examination revealed grade II goiter and a rhythmic heart rate of 156bpm, but was otherwise unremarkable. A 12-lead electrocardiogram showed sinus tachycardia at 140bpm (Fig. 1). Laboratory tests showed normal TSH levels of 1.99μU/mL (0.27–5.91) and high levels of FT4 (3.5ng/dL, 0.8–1.8) and FT3 (6.06pg/mL, 2.57–4.43), which were confirmed in two subsequent measurements. Twenty-four hour Holter monitoring revealed sinus rhythm with maximum heart rate of 158bpm and minimum nighttime HR of 60bpm, with a mean HR of 102bpm, and monomorphic ventricular extrasystoles of moderate severity with doublets and triplets (Fig. 2). Echocardiography showed atrial and left ventricular dilation with mild systolic function, tricuspid insufficiency, and severe pulmonary artery hypertension (Table 1). Serologic testing for cardiotropic viruses was negative. Based on the suspicion of hyperthyroidism of a pituitary origin related to persistently elevated thyroid hormones with uncontrolled or inappropriately high TSH, the patient was evaluated by the endocrinology department. The results of baseline pituitary hormone assessment and tests for antithyroid antibodies and thyroid-stimulating immunoglobulin were normal or negative. Glycoprotein hormone subunit α level was 0.41mU/mL (normal <0.8), with a subunit α/TSH ratio of 0.20. A thyroid ultrasound examination revealed multinodular goiter, and a thyroid scan showed an enlarged gland with low uptake in the lower pole of the left lobe. Gadolinium-enhanced MRI of the sella turcica was normal, and a genetic study of the thyroid hormone receptor beta gene (THRβ), performed by sequencing exons 7, 8, 9, and 10, was negative. The TRH test was performed with 200μg IV to measure basal FT4 and TSH at 0, 20, and 60minutes. A maximum TSH increase to 28μU/mL was seen at 20minutes, but decreased to 5.1μU/mL in a repeat test performed after 10 days of oral treatment with 100μg of T3 (Werner test). A final diagnosis of tachycardia-induced cardiomyopathy secondary to hyperthyroidism due to selective pituitary resistance to thyroid hormones was made. Treatment was started with bisoprolol 10mg daily plus 3,5,3′triiodothyroacetic acid 1.4mg in two divided doses for six months. This treatment scheme improved patient symptoms, normalized heart rate, and reversed dilated cardiomyopathy (Table 1). After six months of treatment, TSH and FT4 levels were 0.64U/mL and 1.65mg/dL respectively.
Echocardiographic parameters before and after treatment with triiodothyroacetic acid.
| Parameters | HR (bpm) | LVEDD (mm) | LA(A-P) (mm) | PASP (mmHg) | LVEF (%) |
| Normal | 50–100 (at rest) | <57 | <40 | <35 | 50–75 |
| Before treatmenta | 162 | 59 | 42 | 72 | 47 |
| After treatmentb | 64 | 53 | 38 | 54c | 56 |
LA(A-P): left atrial anteroposterior diameter; LVEDD: left ventricular end-diastolic diameter; HR: heart rate; LVEF: left ventricular ejection fraction; PASP: pulmonary artery systolic pressure.
Thyroid hormone resistance (THR) is a genetic syndrome characterized by decreased tissue sensitivity to the action of thyroid hormones. Although a distinction was formerly made between generalized and selective pituitary resistance, these are now considered to be different forms of clinical expression of the same syndrome with a common molecular origin. Most cases are caused by mutations in the THRβ gene, which encodes for thyroid hormone receptors β1 and β2. Our patient had a selective pituitary resistance and no mutation in the β receptor was found. Mutations are not found in up to 15% of cases, which are considered to be of unknown cause. Such cases could be mosaicisms where the mutated receptor is not present in all tissues. A mutation in some of the co-factors (co-repressor or co-activator proteins) that interact directly or indirectly with the receptor, which eventually results in an impaired genetic transcription, is another possibility. On the other hand, TRα1 receptor mutations in humans have not been clearly identified yet.1
The most important condition to be considered in differential diagnosis is a TSH-secreting pituitary tumor (TSHoma). A subunit α/TSH ratio less than 1 and a negative pituitary MRI support the diagnosis of THR. An exaggerated TSH response to TRH stimulation with a partial and incomplete response to suppression with T3 supported the initial suspected diagnosis of THR, because TSHoma does not usually respond to any stimulus due to autonomous TSH secretion.2,3 Other causes of hyperthyroxinemia with inappropriately normal TSH, such as increased levels of thyroxine-binding globulin (TBG) or transthyretin, familial dysalbuminemic hyperthyroxinemia, the presence of anti-T4 antibodies or anti-TSH heterophile antibodies, or even the early stages of amiodarone treatment, should also be ruled out.4 A majority of these conditions are associated with increased total T4 levels, and patients are characteristically euthyroid, unlike our patient.
Approximately 6% of patients with hyperthyroidism have symptoms of heart failure, but less than 1% develop dilated cardiomyopathy, which could lead to tachycardia and could cause increased cytosolic calcium levels during diastole. These changes result in decreased ventricular contractility and secondary diastolic dysfunction.5 Recent studies have also suggested an association between pulmonary artery hypertension and hyperthyroidism, but the exact pathogenetic mechanism is not known. The most relevant hypothesis for explaining its occurrence is increased cardiac output resulting in endothelial damage, together with an increased metabolism of intrinsic pulmonary vasodilators.6 This type of pulmonary artery hypertension is also usually reversible after adequate treatment of the thyroid condition responsible. To our knowledge, no case has been reported to date of tachycardia-induced cardiomyopathy secondary to hyperthyroidism due to selective pituitary resistance to thyroid hormone. Our patient experienced left chamber dilation combined with severe pulmonary artery hypertension which was caused by persistent sinus tachycardia and frequent ventricular extrasystoles secondary to hyperthyroidism.
Triiodothyroacetic acid is a T3 analogue with a predominant pituitary and hepatic effect which has been shown to be of value for the treatment of selective pituitary resistance to thyroid hormones at doses ranging from 1.4 to 2.8mg/day,1,7 although partial or no response has been reported in some cases.8 Dextrothyroxine is another agent with a TSH-suppressing effect greater than levothyroxine which does not significantly affect cardiac function and has been shown to be effective in patients not responding to triiodothyroacetic acid. In the near future, new specific analogues of TRβ2 and TRβ1 receptors could be more effective for the treatment of pituitary resistance to thyroid hormones. On the other hand, ablation treatment with radioiodine and/or thyroid surgery may be detrimental in these patients, because it induces a chronic, sustained elevation of TSH levels with the probable subsequent occurrence of thyroid hyperplasia or adenoma.4,7 Treatment with bisoprolol 10mg/day before the final diagnosis of our patient was unable to control tachycardia or extrasystole. Once the final diagnosis of selective pituitary resistance to thyroid hormones had been made, treatment was started with triiodothyroacetic acid at a dose of 1.4mg daily, which achieved an excellent response at 6 months, with the disappearance of symptoms and thyroid hormone normalization. An adequate control of heart rate and 24-hour Holter monitoring (mean heart rate of 64bpm, no extrasystoles) was also achieved. Echocardiography showed a significant improvement in pulmonary artery pressure, with a return to the baseline state of moderate pulmonary artery hypertension and the disappearance of left ventricular and atrial dilation. Systolic function also normalized.
In conclusion, tachycardia-induced cardiomyopathy associated with hyperthyroidism due to selective pituitary resistance to thyroid hormones is an exceptional and reversible cause of dilated cardiomyopathy and pulmonary artery hypertension. Triiodothyroacetic acid is currently a safe and effective drug for the adequate management and treatment of this condition.
Please cite this article as: González-Duarte DJ, et al. Taquimiocardiopatía metabólica asociada a resistencia a las hormonas tiroideas. Endocrinol Nutr. 2013;60:100–2.