The aim of the study was to estimate the direct costs of healthcare provided to patients with type 2 diabetes mellitus (T2DM) in the Basque Country and to compare them with those of the population with chronic diseases.
Material and methodsA retrospective, cross-sectional, population-based study. Direct healthcare costs for patients aged over 35 years diagnosed with T2DM in the Basque Country (n=126,894) were calculated, stratified by age, sex and deprivation index, and compared to the costs for the population diagnosed with a chronic disease other than T2DM (n=1,347,043).
ResultsThe annual average healthcare cost of a person with T2DM was €3432. Cost gradually increased with age to €4313 in patients aged 80–84 years. Cost in males were €161 higher as compared to costs in females (P<0.001). In the most socioeconomically disadvantaged areas, cost per patient was €468 (14.9%) greater than in the most privileged areas (P<0.001). Moreover, cost was 68.5% higher (P<0.001) for patients with T2DM than for patients with other chronic diseases. Total annual direct costs amounted to €435.5 million, or 12.78% of total public health expenditure in the region.
ConclusionsDirect mean healthcare costs in the Basque Country for patients with T2DM were higher in males, in the most underprivileged areas, in patients with comorbidities, and in older age groups, and represented €3432 per person per year.
El propósito del estudio fue estimar los costes directos de la atención sanitaria prestada a pacientes con diabetes mellitus tipo 2 (DMT2) en el País Vasco y compararlos con aquellos de la población general con enfermedades crónicas.
Material y métodosPara este estudio transversal, calculamos los costes directos de la atención sanitaria para personas mayores de 35 años con diagnóstico de DMT2 residentes en el País Vasco (n=126.894) por edad, sexo e índice de privación, y los comparamos con los costes de la población con diagnóstico de una enfermedad crónica distinta a la DMT2 (n=1.347.043).
ResultadosLos costes sanitarios anuales de una persona con DMT2 ascendieron a 3.432€. Los costes se incrementaron progresivamente con la edad, hasta 4.313€ para personas entre 80 y 84 años. El gasto en hombres fue 161€ mayor que en mujeres (p<0,001). En las áreas más socioeconómicamente desfavorecidas, el coste por paciente fue 468€ (14,9%) mayor que en el segmento más favorecido (p<0,001). Además, los costes fueron un 68,5% mayores (p<0,001) para personas con DMT2 que para otros pacientes con enfermedades crónicas. Los costes directos anuales totales ascendieron a 435,5 millones de euros, lo que constituye un 12,78% del gasto total en sanidad de la región.
ConclusionesEn el País Vasco, el coste directo medio de la atención sanitaria a personas con DMT2 es de 3.432€. Este coste es mayor en hombres, en las zonas más desfavorecidas, en grupos de edad más avanzada y crece según el número de comorbilidades.
Type 2 diabetes mellitus (T2DM) is a chronic disease highly prevalent in Spain1 that has negative effects on health and quality of life of people. T2DM also represents a financial burden for society because of its high costs, both direct–related to treatments–and indirect–in terms of productivity losses.2 Patients with T2DM often experience chronic complications associated to the disease, both microvascular and macrovascular, as well as greater chronic multimorbidity.
In Spain, various studies and a systematic review have recently estimated healthcare costs incurred by the population with diabetes,2–6 updating the findings of the classical studies conducted in the first decade of the 21st century.7–10 The purpose of these studies was to estimate the costs associated to diabetes (considering T2DM costs only in some cases, and costs of both type 1 diabetes mellitus and T2DM in other studies), identifying the resources associated to provision of care for diabetes and its complications. All studies considered the direct costs associated to diabetes mellitus, while some of them also estimated indirect costs.
There is agreement in that calculation of healthcare costs associated to T2DM should take into account all episodes related to the disease, as well as use of the resources needed for prevention and treatment of complications. On the other hand, there is an increasing emphasis on the burden of morbidity in people with diabetes due to diseases other than T2DM or their associated complications.11 In this regard, Struijs et al.,12 among other authors, have shown that comorbidities not related to diabetes have an effect, in terms of healthcare costs, similar to or greater than that of comorbidities related to diabetes.
Because of the foregoing, we will focus on the direct healthcare costs associated to provision of care to patients with T2DM. As the annual healthcare costs incurred by patients with T2DM and no comorbidities had been estimated to be €721 greater13 than the costs for a healthy person in the Basque Country, it was decided to compare the costs of the population with T2DM and those of the population with chronic diseases in a context of high prevalence of chronicity.
To summarize, the objective of this study was to estimate the direct healthcare costs associated to provision of care to patients with T2DM in the Basque Country and to compare them to those of the overall population of chronically ill patients.
Patients and methodsThe study was approved by the research ethics committee of the Basque Country (PI2014074). Informed consent was not requested because the clinical histories of patients were anonymized before they were used for this analysis.
This cross-sectional study focused on the period from September 1, 2010 to August 31, 2011 to calculate the direct healthcare costs of all people over 35 years of age with diagnosis of T2DM in the Basque Country (n=126,894). For this, data were retrospectively collected using the PREST database.14
The Basque health system is a universal system based on taxes that virtually covers 100% of the population. In fact, the total population included in the PREST database was 2,262,707 (the official population is 2,191,000, but health services are also provided to irregular migrants and other population not appearing in the official census). The study population consisted of all people who were covered by the public health insurance of the Basque Country as of August 31, 2011 and who had been covered for at least six months in the previous year, whether or not they had used it or had had any contact with the Basque Health Service.
This database contains information from several sources on individual patients. Such information includes sociodemographic variables (age, sex, deprivation index); International Classification of Diseases, 9th revision, diagnosis codes15 Clinical Modification (ICD-9-CM) assigned at primary care, emergency room, and during hospital admission; use of services in primary care, emergency room, and hospital ward, and procedures performed and prescriptions coded in accordance to the Anatomical Therapeutic Chemical (ATC) classification system.16
A methodology already reported in prior publications was used to identify patients with chronic diseases.13 A listing of 52 health problems that were considered to be chronic because they usually require a long treatment period (more than 12 months) or cause disorders that affect quality of life and restrict physical or social activities during that same period. People who had one or more of those diseases (excluding those with T2DM) form the population of “patients with chronic diseases”.
Several algorithms have been proposed in the literature to identify patients with diabetes in administrative databases.17,18 In this study, the method used for including patients with T2DM was to consider all patients who, according to databases of the Basque Health Service, had received any diagnosis related to T2DM or oral antidiabetic drugs at any time during their lives, regardless of whether or not they had had any contact with the health service during the study period. Patients diagnosed with type 1 diabetes mellitus and with an unspecified type of diabetes mellitus who were treated with insulin only were excluded.
The deprivation index of the census section of residence was used as social indicator. A section is the smallest territorial unit to which information from the population census may be disaggregated, and is mainly defined by population volume criteria, being also delimited by geographical or urban features of the territory. Median population by census section is 1200 inhabitants. This small size favors homogeneity of the households that comprise each section. This index was constructed from indicators relating to work (unemployment, manual and eventual workers) and education (inadequate education, overall and in young people). For this study, the deprivation index was categorized into quintiles, with quintile 1 representing the area with least social deprivation and quintile 5 the most deprived area.
The costs corresponding to each item were assessed as follows. Costs of prescriptions were directly taken from the registry of prescriptions of each patient. For emergency care, rehabilitation sessions, visits to outpatient clinics and visits to primary care physicians and nurses, laboratory tests and imaging studies requested in outpatient care, and some treatments such as dialysis, radiation therapy, and chemotherapy received at the day hospital, the number of service provided to each patient was multiplied by the standard costs at our health service. Finally, costs of hospitalization and outpatient major surgery procedures were estimated based on weight of their corresponding diagnosis-related groups.
Services whose data could not be accessed were excluded from the first cost estimations. Such services included admissions to psychiatric hospitals, home hospital services, and day hospital (except the above mentioned procedures), healthcare transport services, and prostheses and other equipment for use at home, as well as self-testing materials (test strips, needles and syringes, etc.).
Analyses were performed after stratification by patient sex and age and by deprivation index. A descriptive analysis was made of the costs separately considering several components. Mean costs and their standard deviations were calculated by age and sex group. A nonparametric ANOVA analysis was used to assess differences in cost distribution by age, age range, or deprivation index, and between patients with T2DM and those with at least one chronic disease other than T2DM. Statistical analysis was performed using Stata software for data analysis and statistics, version 12 (StataCorp, LP, College Station, TX).
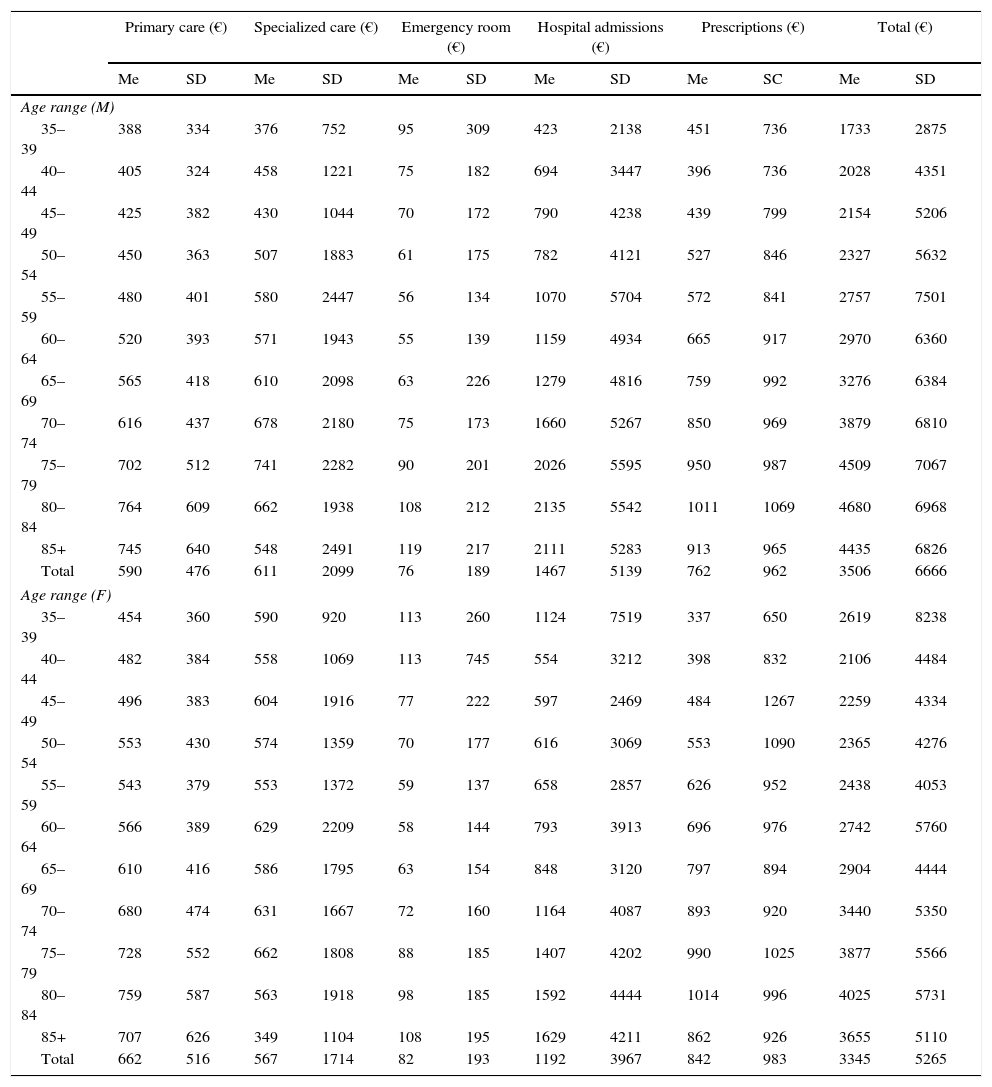
ResultsMean healthcare costs by patient with DMT2 and year were €3432 (Table 1) and €3506 and €3345 for men and women respectively. That is, expense was 4.81% higher in men with T2DM as compared to women with the disease (P<0.001). When are ranges were considered, a progressive increase was found in healthcare costs with age, with a peak of €4132 by patient in the group aged 80–84 years.
Mean and standard deviation of costs by patient with T2DM by sex and age range.
| Primary care (€) | Specialized care (€) | Emergency room (€) | Hospital admissions (€) | Prescriptions (€) | Total (€) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Me | SD | Me | SD | Me | SD | Me | SD | Me | SC | Me | SD | |
| Age range (M) | ||||||||||||
| 35–39 | 388 | 334 | 376 | 752 | 95 | 309 | 423 | 2138 | 451 | 736 | 1733 | 2875 |
| 40–44 | 405 | 324 | 458 | 1221 | 75 | 182 | 694 | 3447 | 396 | 736 | 2028 | 4351 |
| 45–49 | 425 | 382 | 430 | 1044 | 70 | 172 | 790 | 4238 | 439 | 799 | 2154 | 5206 |
| 50–54 | 450 | 363 | 507 | 1883 | 61 | 175 | 782 | 4121 | 527 | 846 | 2327 | 5632 |
| 55–59 | 480 | 401 | 580 | 2447 | 56 | 134 | 1070 | 5704 | 572 | 841 | 2757 | 7501 |
| 60–64 | 520 | 393 | 571 | 1943 | 55 | 139 | 1159 | 4934 | 665 | 917 | 2970 | 6360 |
| 65–69 | 565 | 418 | 610 | 2098 | 63 | 226 | 1279 | 4816 | 759 | 992 | 3276 | 6384 |
| 70–74 | 616 | 437 | 678 | 2180 | 75 | 173 | 1660 | 5267 | 850 | 969 | 3879 | 6810 |
| 75–79 | 702 | 512 | 741 | 2282 | 90 | 201 | 2026 | 5595 | 950 | 987 | 4509 | 7067 |
| 80–84 | 764 | 609 | 662 | 1938 | 108 | 212 | 2135 | 5542 | 1011 | 1069 | 4680 | 6968 |
| 85+ | 745 | 640 | 548 | 2491 | 119 | 217 | 2111 | 5283 | 913 | 965 | 4435 | 6826 |
| Total | 590 | 476 | 611 | 2099 | 76 | 189 | 1467 | 5139 | 762 | 962 | 3506 | 6666 |
| Age range (F) | ||||||||||||
| 35–39 | 454 | 360 | 590 | 920 | 113 | 260 | 1124 | 7519 | 337 | 650 | 2619 | 8238 |
| 40–44 | 482 | 384 | 558 | 1069 | 113 | 745 | 554 | 3212 | 398 | 832 | 2106 | 4484 |
| 45–49 | 496 | 383 | 604 | 1916 | 77 | 222 | 597 | 2469 | 484 | 1267 | 2259 | 4334 |
| 50–54 | 553 | 430 | 574 | 1359 | 70 | 177 | 616 | 3069 | 553 | 1090 | 2365 | 4276 |
| 55–59 | 543 | 379 | 553 | 1372 | 59 | 137 | 658 | 2857 | 626 | 952 | 2438 | 4053 |
| 60–64 | 566 | 389 | 629 | 2209 | 58 | 144 | 793 | 3913 | 696 | 976 | 2742 | 5760 |
| 65–69 | 610 | 416 | 586 | 1795 | 63 | 154 | 848 | 3120 | 797 | 894 | 2904 | 4444 |
| 70–74 | 680 | 474 | 631 | 1667 | 72 | 160 | 1164 | 4087 | 893 | 920 | 3440 | 5350 |
| 75–79 | 728 | 552 | 662 | 1808 | 88 | 185 | 1407 | 4202 | 990 | 1025 | 3877 | 5566 |
| 80–84 | 759 | 587 | 563 | 1918 | 98 | 185 | 1592 | 4444 | 1014 | 996 | 4025 | 5731 |
| 85+ | 707 | 626 | 349 | 1104 | 108 | 195 | 1629 | 4211 | 862 | 926 | 3655 | 5110 |
| Total | 662 | 516 | 567 | 1714 | 82 | 193 | 1192 | 3967 | 842 | 983 | 3345 | 5265 |
SD: standard deviation; M: male; F: female; Me: mean.
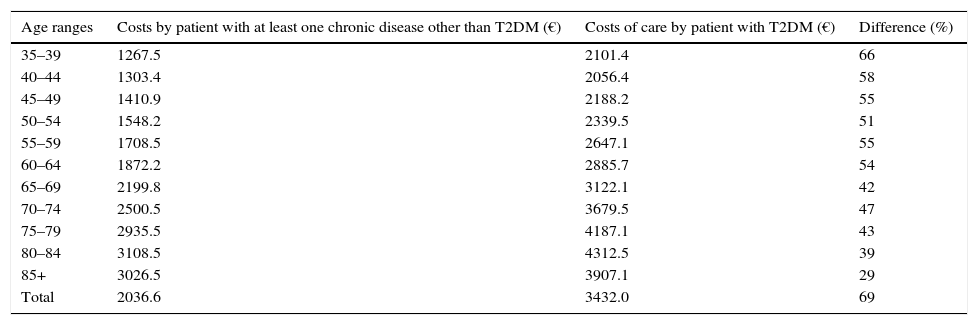
When data from patients with T2DM were compared to those of patients with other chronic diseases, costs were greater in those with T2DM in all age ranges considered (Table 2). Specifically, mean healthcare costs for a patient with a chronic disease other than T2DM were €2036.5, almost 69% lower than those of a patient with T2DM, with differences in healthcare costs being significant for all age groups analyzed.
Comparison of costs by person between patients with T2DM and those with at least one chronic disease other than T2DM.
| Age ranges | Costs by patient with at least one chronic disease other than T2DM (€) | Costs of care by patient with T2DM (€) | Difference (%) |
|---|---|---|---|
| 35–39 | 1267.5 | 2101.4 | 66 |
| 40–44 | 1303.4 | 2056.4 | 58 |
| 45–49 | 1410.9 | 2188.2 | 55 |
| 50–54 | 1548.2 | 2339.5 | 51 |
| 55–59 | 1708.5 | 2647.1 | 55 |
| 60–64 | 1872.2 | 2885.7 | 54 |
| 65–69 | 2199.8 | 3122.1 | 42 |
| 70–74 | 2500.5 | 3679.5 | 47 |
| 75–79 | 2935.5 | 4187.1 | 43 |
| 80–84 | 3108.5 | 4312.5 | 39 |
| 85+ | 3026.5 | 3907.1 | 29 |
| Total | 2036.6 | 3432.0 | 69 |
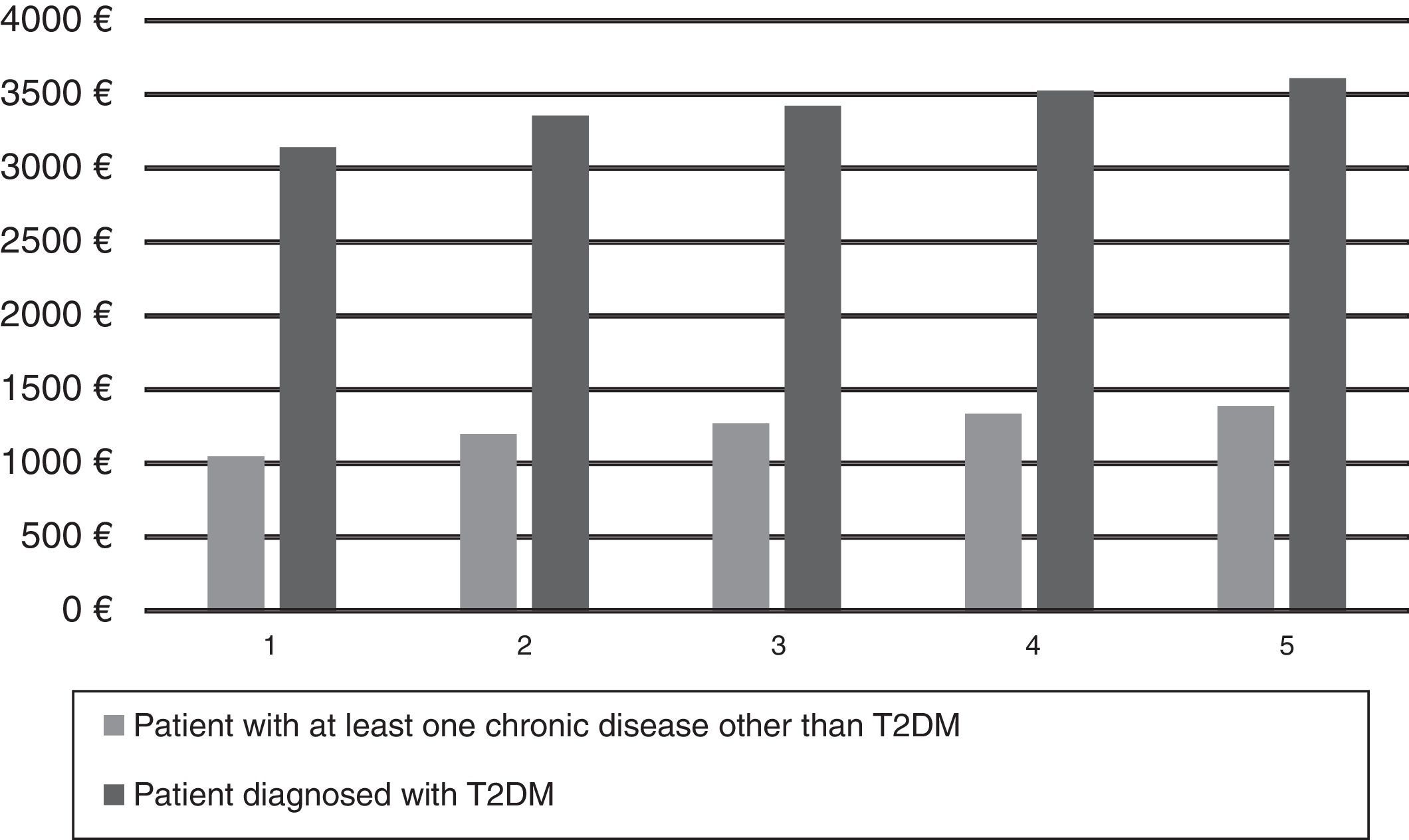
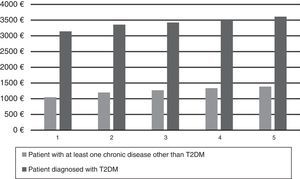
As regards costs as a function of the social deprivation index, Fig. 1 shows that a socioeconomic gradient exists in costs associated to T2DM: the greater the deprivation level, the higher the healthcare costs. The difference in healthcare costs between the richest patients (deprivation index 1) and the poorest patients (deprivation index 5) was €468, i.e. 14.9% (P<0.001). Differences between all socioeconomic groups were statistically significant.
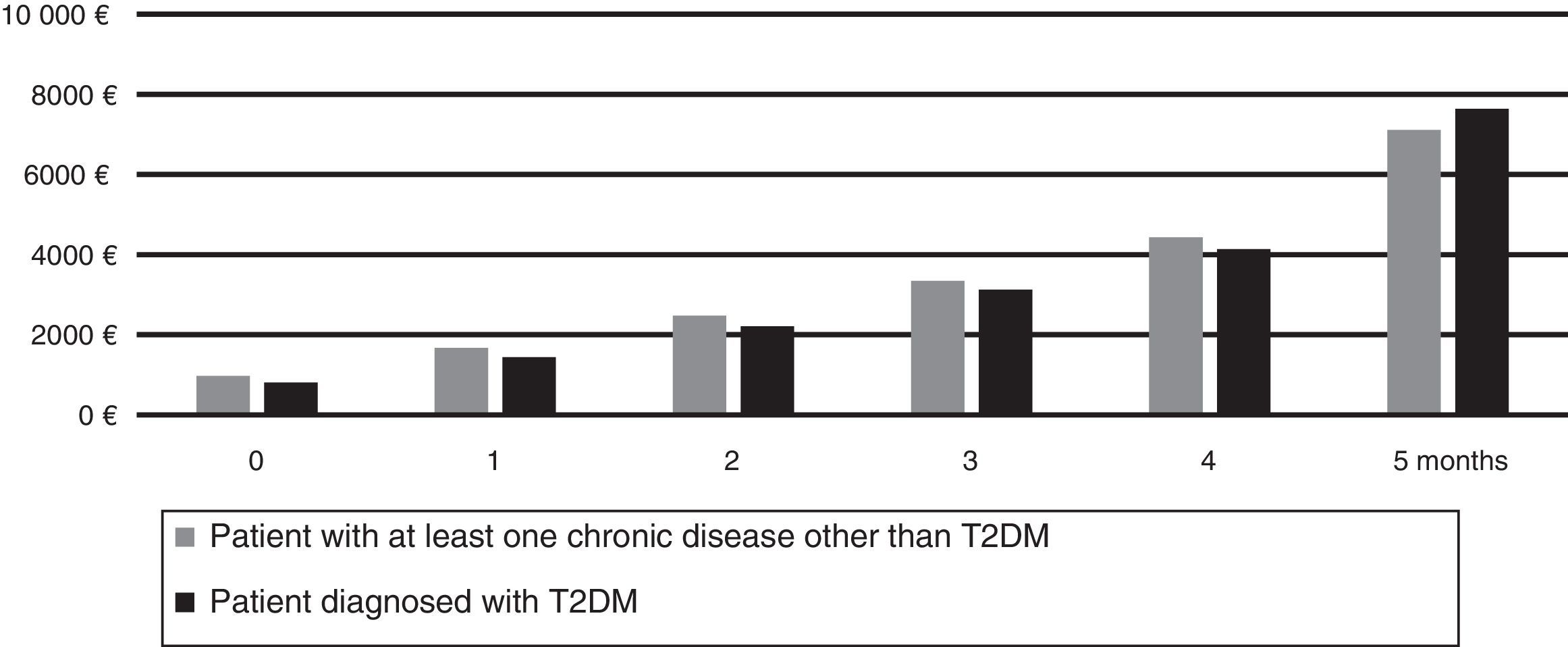
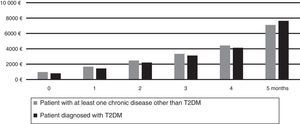
With regard to comorbidity, Fig. 2 shows how costs gradually increase as the number of comorbidities increase, and that mean cost is greater in patients with no T2DM who have up to four chronic diseases, and is lower in those with five or more chronic diseases.
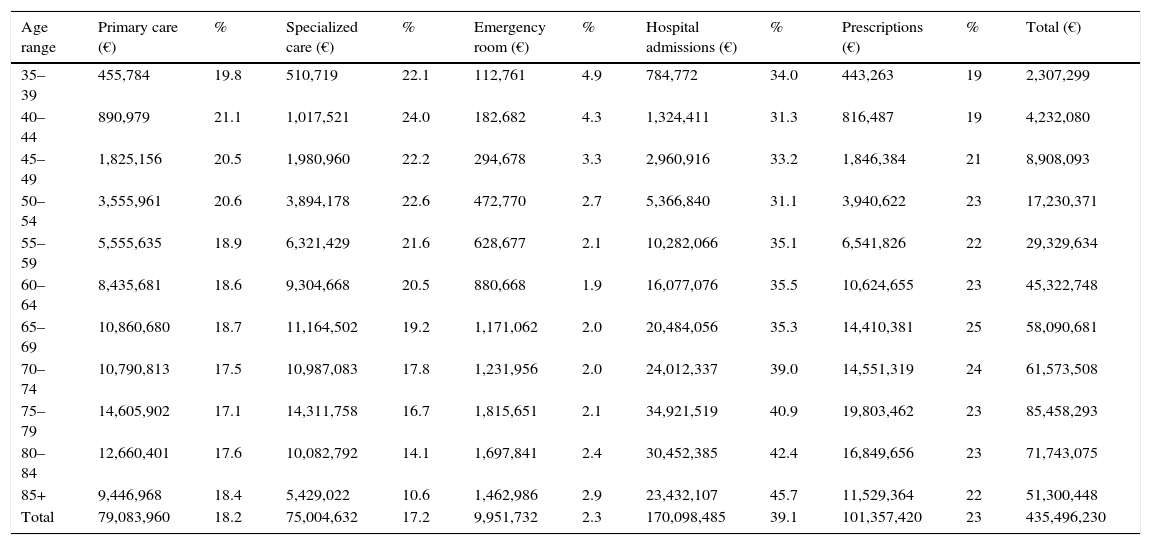
As to the total costs associated to care of patients with T2DM, the estimations provided in Table 3 were obtained taking into account the prevalence of the disease and mean costs in men and women. Overall healthcare costs associated to care of patients with T2DM were €435.5 million, with hospital admissions accounting for the greatest part, €170 million. Moreover, although younger groups made a greater use of primary care and specialized services and the number of prescriptions and hospital admissions was higher in the older groups, distribution of healthcare costs in each age group by item was very similar. Provision of care to patients with T2DM in the Basque Country accounted for 12.78% of the total public health budget in 2011.19
Costs for patients with T2DM, overall and by item (%).
| Age range | Primary care (€) | % | Specialized care (€) | % | Emergency room (€) | % | Hospital admissions (€) | % | Prescriptions (€) | % | Total (€) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 35–39 | 455,784 | 19.8 | 510,719 | 22.1 | 112,761 | 4.9 | 784,772 | 34.0 | 443,263 | 19 | 2,307,299 |
| 40–44 | 890,979 | 21.1 | 1,017,521 | 24.0 | 182,682 | 4.3 | 1,324,411 | 31.3 | 816,487 | 19 | 4,232,080 |
| 45–49 | 1,825,156 | 20.5 | 1,980,960 | 22.2 | 294,678 | 3.3 | 2,960,916 | 33.2 | 1,846,384 | 21 | 8,908,093 |
| 50–54 | 3,555,961 | 20.6 | 3,894,178 | 22.6 | 472,770 | 2.7 | 5,366,840 | 31.1 | 3,940,622 | 23 | 17,230,371 |
| 55–59 | 5,555,635 | 18.9 | 6,321,429 | 21.6 | 628,677 | 2.1 | 10,282,066 | 35.1 | 6,541,826 | 22 | 29,329,634 |
| 60–64 | 8,435,681 | 18.6 | 9,304,668 | 20.5 | 880,668 | 1.9 | 16,077,076 | 35.5 | 10,624,655 | 23 | 45,322,748 |
| 65–69 | 10,860,680 | 18.7 | 11,164,502 | 19.2 | 1,171,062 | 2.0 | 20,484,056 | 35.3 | 14,410,381 | 25 | 58,090,681 |
| 70–74 | 10,790,813 | 17.5 | 10,987,083 | 17.8 | 1,231,956 | 2.0 | 24,012,337 | 39.0 | 14,551,319 | 24 | 61,573,508 |
| 75–79 | 14,605,902 | 17.1 | 14,311,758 | 16.7 | 1,815,651 | 2.1 | 34,921,519 | 40.9 | 19,803,462 | 23 | 85,458,293 |
| 80–84 | 12,660,401 | 17.6 | 10,082,792 | 14.1 | 1,697,841 | 2.4 | 30,452,385 | 42.4 | 16,849,656 | 23 | 71,743,075 |
| 85+ | 9,446,968 | 18.4 | 5,429,022 | 10.6 | 1,462,986 | 2.9 | 23,432,107 | 45.7 | 11,529,364 | 22 | 51,300,448 |
| Total | 79,083,960 | 18.2 | 75,004,632 | 17.2 | 9,951,732 | 2.3 | 170,098,485 | 39.1 | 101,357,420 | 23 | 435,496,230 |
In a context where “the most common chronic disease suffered by adults is multimorbidity”,20 greater emphasis should be placed on individuals and the population affected by a disease or series of diseases, rather than analyze the costs attributable to a specific disease.
This study quantified the direct healthcare costs associated to provision of care to patients (over 35 years of age) with T2DM in the Basque public health system. Many studies have previously been conducted to try and estimate the costs associated to diabetes in Spain using different approaches and methods.2–10 None of those studies is directly comparable to ours, because they focused on estimation of the costs associated to T2DM in a population, whereas the present study estimates the direct healthcare costs in a population diagnosed with T2DM. In addition to that substantial difference in the perspective adopted, other differences exist in how costs and categories of costs used are estimated, and also in the sourced and quality of data used. Moreover, in terms of cost comparisons, this study compared a population with T2DM to a population diagnosed a chronic disease, while other studies used a population without diabetes for comparison.
Despite methodological differences, however, some parallelism exists with studies by Mata3 and Mata et al.6 in Catalonia, recently conducted and using similar approaches (population base, direct cost, etc.). Thus, a mean cost of €3110 and an additional cost ratio of 1.77 were reported for Catalonia, as compared to €3432 and a ratio of 1.69 in this study. Interestingly, hospitalizations had a similar weight in both studies: 41% in Catalonia and 39% in the Basque Country.
As regards the impact on public health expense, care of T2DM was estimated to account for 8.2% in Spain,4 as compared to 12.78% for the Basque Country in this study. Comparisons with international study have many limitations. However, to quote some examples, costs of care for diabetes account for only 5.8% of the total healthcare budget in Finland,21 but for more than 20% in the USA.11
We have also shown that healthcare costs associated to T2DM increase with comorbidity, age (except for a plateau or slight decline at more advanced ages), and deprivation. Several studies have found an association between the socioeconomic level and prevalence of T2DM,22,23 with greater prevalence of the disease in the most disadvantaged groups. Our data also underline the difference in costs between people of socioeconomic levels, according to the findings of Larrañaga et al.,24 who reported that the lower the socioeconomic level of patients with T2DM, the greater the level of risk factors and chronic complications and the poorer the control of disease, despite more frequent visits to primary care.
An additional strength of our study is access to population databases containing information about use and costs of healthcare services for all patients covered by the public health system in an autonomous community. This allowed for developing a methodology focused on people with T2DM rather than on the disease itself, so that the analysis was based on resource utilization by each patient diagnosed with T2DM obtained from direct information sources. In addition, comparison between patients with T2DM and those with no T2DM but diagnosed with a chronic disease gives an idea of excess cost of diabetes as compared to other chronic diseases. Finally, analysis of costs by socioeconomic group is another strength of the study, as this is a disease where this factor has a significant impact on costs.
This study also has limitations, some of them inherent to the characteristics of population databases, in which some information may be lacking. Thus, actual healthcare costs associated to patients with T2DM may have been underestimated, because costs calculated in this study are based on the diagnosed prevalence, i.e. on the known cases, but a significant proportion of people with T2DM are not diagnosed yet.1 In addition, some direct healthcare costs are not included due to the lack of information that allows for their adequate imputation. Data on private healthcare expense is not included either because they cannot be accessed. Indirect and intangible costs have not been considered because of the nature of the study and the methods and sources used.
On the other hand, it should be admitted that this type of cost in studies of diseases only provides descriptive information, which is helpful to increase awareness of a health problem, but is poorly adequate for decision making.
To sum up, it was shown that healthcare costs associated to provision of care to patients with T2DM account for almost 13% of total public healthcare expense in the Basque Country. Costs are higher in men and in the most disadvantaged population groups, and increase with age (except in patients older than 85 years) and comorbidity.
AuthorshipAuthors contributed to this study were as follows: EAM, JFO, and RNS designed the study. EAM and JFO participated in data collection. EAM analyzed the data. JMAA, PEL, and SG provided expert knowledge. All authors contributed to data interpretation and to preparation and revision of the manuscript. All authors read and approved the final manuscript.
Roberto Nuño-Solinís is the guarantor of the study and, as such, has full access to study data and assumes responsibility for data integrity and accuracy of data analysis.
Conflicts of interestThe authors declare a conflict of interest associated to external funding of the manuscript by Sanofi-Aventis. However, Sanofi-Aventis had no role in study design and conduct; data collection, management, analysis, and interpretation; or preparation, revision, or approval of the manuscript.
The authors thank the pharmaceutical company Sanofi-Aventis for collaboration in funding and for support to increase awareness of diabetes, and also thank Nuria Toro Polanco, Iñaki Fraile, and Mariluz Marqués for their contributions to the study.
Please cite this article as: Nuño-Solinís R, Alonso-Morán E, Arteagoitia Axpe JM, Ezkurra Loiola P, Orueta JF, Gaztambide S. Costes sanitarios de la población con diabetes mellitus tipo 2 en el País Vasco (España). Endocrinol Nutr. 2016;63:543–550.