Diabetes mellitus (DM) is a highly prevalent disease worldwide which currently affects 347 million people according to the World Health Organization. There are complications of diabetes which are little known either to healthcare professionals or to the patients themselves, including periodontal disease and other manifestations in the oral cavity such as xerostomia, a burning sensation, and increased infection.1,2 The aim of this study was to assess whether patients with DM have a greater frequency of xerostomia.
A descriptive study was conducted in 200 patients, 100 with DM and 100 with no DM, who attended the outpatient endocrinology clinic of the hospital from January 2012 to January 2013. Patients gave their written informed consent to participate in this study. Study variables included age, sex, type of DM, time since the onset of DM, and glycosylated hemoglobin. As the dependent variable, the frequency of symptoms which have been related to the presence of xerostomia was assessed using the Xerostomia Inventory, translated into Spanish from the original English version.3 This consists of 11 questions on symptoms related to dry mouth. Answers to each of the questions were “hardly ever” (1 point), “occasionally” (2 points), and “fairly often/very often” (3 points). The patients completed the questionnaire after the medical visit as previously instructed by the physician in charge. Laboratory tests were always performed after fasting for 12h. Exclusion criteria included: age older than 65 years, smoking, the use of drugs related to the occurrence of xerostomia, a history of radiation to the head and neck, and diseases causing dry mouth. The statistical software used was SPSS® version 15.0. Quantitative variables are given as mean and standard deviation, and dichotomic variables as percentages. Student's t test was used to study differences in total score in the Xerostomia Inventory between patients with or without diabetes.
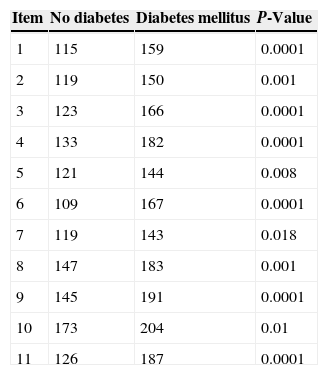
Among the 100 patients with no DM, 42 (42%) were male and 58 (58%) female. The mean patient age was 41.5±13.4 years. Of the 100 patients with diabetes, 50 (50%) were male and 50 (50%) female. The mean age of these patients was 49.3±13.4 years. No statistically significant differences were found between the two groups in these data. Thirty-six patients with DM (36%) had type DM, and 64 (64%) had type 2 DM. The mean time since DM onset was 12±8.6 years, and the mean HbA1c was 7.88±1.19%. Forty patients (42%) were treated with insulin alone, 37 patients (37%) with oral antidiabetic drugs alone, and 23 patients (23%) with both insulin and oral antidiabetic drugs. Individual analysis of each Xerostomia Inventory item revealed statistically significant differences in all of them between DM patients and the control group (Table 1). No statistically significant differences were found between patients with T1DM and T2DM. As regards the HbA1c value, a difference was only seen in item 3, where patients with HbA1c greater than 7% had higher scores as compared to those with HbA1c levels of 7% or less (Chi-square test: p=0.037). No significant differences were found either as regards time since DM onset between patients with 10 or fewer years and those with 10 or more years.
Xerostomia is a relatively common condition in the general population, with rates ranging from 13% to 63%.4 Multiple studies show that xerostomia is the most common oral manifestation in diabetic patients.5–7 According to Tommasi,5 the most common oral manifestations in diabetic patients include xerostomía, a burning sensation, ulcers, pharyngeal candidiasis, cheilitis, lichen planus, salivary gland swelling, gingival problems, periodontal problems, abscesses, and the loss of alveolar bone.
This study found a greater prevalence of dry mouth in diabetic as compared to non-diabetic patients, but with no differences by type of DM, time since disease onset, or degree of metabolic control. This association appears to be little recognized. A recent study of 200 young diabetic patients with a mean age of 42 years, 58% of whom had T2DM, found that only 14% of them visited their dentists annually.8 Investigating awareness of the general complications associated with the disease, they found that 90% of patients had been advised on coronary disease and 85% on kidney disease, but only 50% were aware of the risk of periodontitis, tooth decay, and oral infections. Moreover, 76% of patients had dry mouth, and only 30% of these had been warned about the potential consequences of dry mouth on their oral health.
Our study has several limitations. First of all, the translated version of the Xerostomia Inventory has not been validated in Spanish. In addition, a hospital sample was used, which limits the generalizability of our results. The difficulty of measuring the degree of xerostomia, which is based on subjective sensations, should also be taken into consideration.
In conclusion, xerostomia is a common manifestation in diabetic patients which, according to the published studies, appears to have an influence on the occurrence of periodontal disease. Despite this, the association is not sufficiently recognized, which makes early diagnosis and adequate treatment of the condition difficult. Because of the high frequency and significance of this disease, we recommend that further studies be conducted and that more information be provided to both healthcare professionals and patients.
FundingNo funding was received for this research.
AuthorshipStudy conception and design, data collection, data analysis, manuscript writing, and critical review: Cristina Navea Aguilera.
Data collection, data analysis, and critical review: M. Guadalupe Guijarro de Armas, María Merino Viveros, and Clara Torán Ranero.
Study conception and design, data collection, critical review, and approval of the final version for publication: Susana Monereo Megías.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Navea Aguilera C, Guijarro de Armas MG, Monereo Megías S, Merino Viveros M, Torán Ranero C. Relación entre xerostomía y diabetes mellitus: una complicación poco conocida. Endocrinol Nutr. 2015;62:45–46.