The patient was a 63-year-old man with a medical history of active smoking and high blood pressure under dietary management. He consulted due to clinical symptoms involving four days of pain in the joints of his shoulders, elbows, knees and left ankle, associated with myalgia of proximal predominance in the four extremities and fever of 38.2°C. He had no respiratory, gastrointestinal, genitourinary or dermatological symptoms. He did not remember any tick bites, and nor did he live with animals. He denied sexually transmitted infections (STIs). Physical examination revealed an increase in the volume of the aforementioned joints, with local heat and pain on palpation with semiology of joint effusion predominantly in the left knee; the rest of the physical examination showed no alterations. With the initial diagnosis of reactive arthritis vs. microcrystalline arthritis he was admitted for study and symptomatic management. In the admission laboratory tests, the following were noteworthy: complete blood count with 14,000 leukocytes/mm3, neutrophils 11,300, normal haemoglobin and platelets, C-reactive protein 236 mg/l, ESR 79 mm/h, ferritin 376 µg/L. The rest of the laboratory tests, which included creatinine, sodium, potassium, calcium, uric acid, transaminases, bilirubin, alkaline phosphatase, LDH, creatine kinase, TSH, and procalcitonin, presented no abnormalities. The immunological study revealed positive antinuclear antibodies 1:80 with a homogeneous pattern, with negative antibodies to extractable nuclear antigens, normal immunoglobulins, negative rheumatoid factor and C3-C4 complement, as well as normal CH50. Syphilis, HBV, HCV, VDRL and HIV serology tests were negative. X-rays of the affected joints were requested, which showed no alterations.
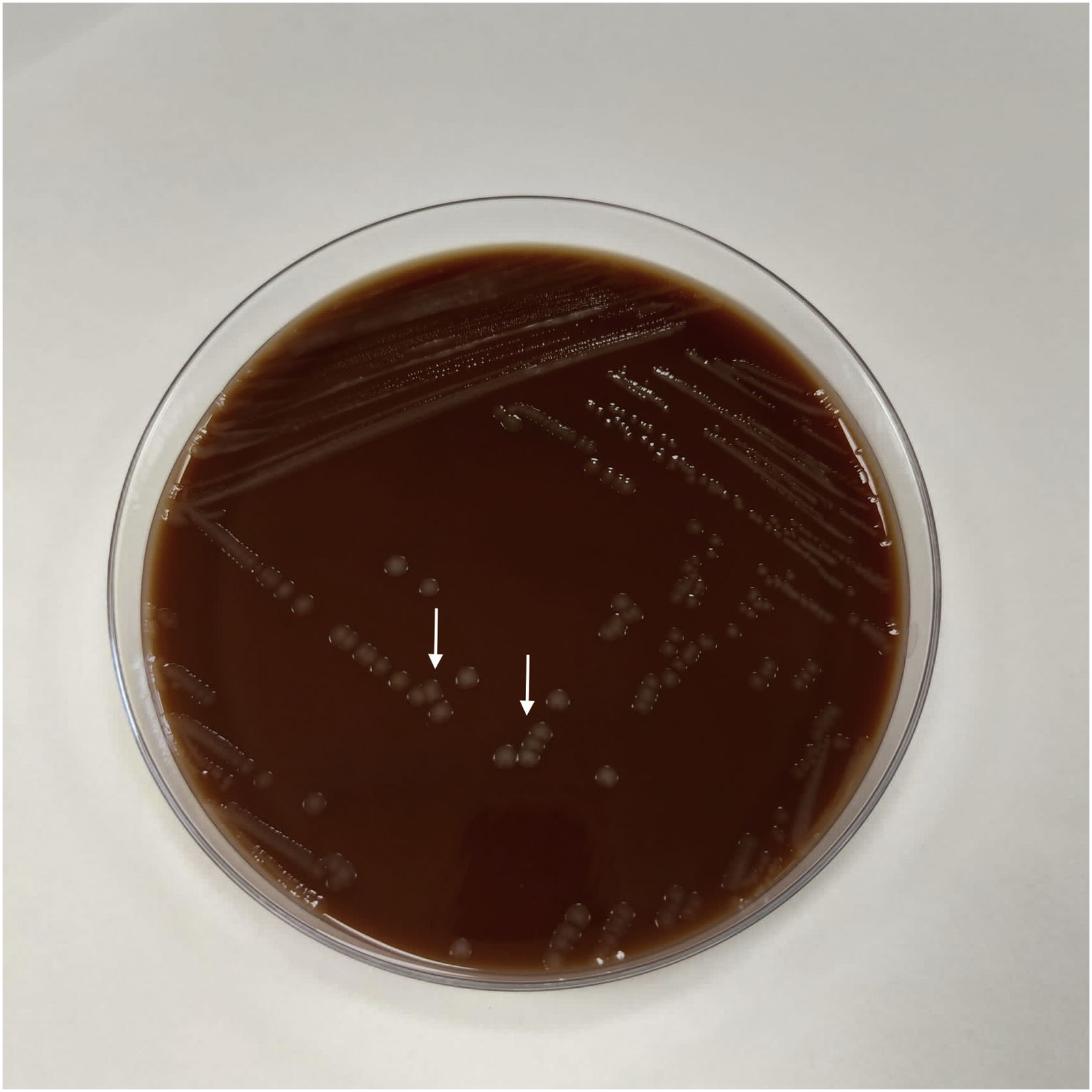
Clinical courseSymptomatic treatment with non-steroidal anti-inflammatory drugs was started, without a significant improvement. A left-knee arthrocentesis was performed, with an output of intense yellow fluid with the presence of 47,641 leukocytes/mm3, 97% normal neutrophils, proteins and glucose, and no microcrystals observed. Gram stain revealed gram-negative bacteria that were grouped in the form of diplococci (Fig. 1). Culture was performed in fluid medium (thioglycolate) and subsequently subcultured in chocolate agar, showing growth of colonies at 24 h that were identified by MALDI-TOF as being consistent with Neisseria gonorrhoeae (Fig. 2), confirming the diagnosis of gonococcal arthritis. Blood and urine cultures were negative, as was urine polymerase chain reaction for Neisseria gonorrhoeae and Chlamydia trachomatis. The patient was interviewed again after the results and he confirmed risky sexual relations. Treatment with intravenous ceftriaxone, 1 g every 24 h for 4 days, was started (the intravenous route was considered due to the significant clinical involvement), with significant improvement, then continuing with cefixime 400 mg every 12 h until 10 days of treatment had been completed based on the antibiogram (ceftriaxone and cefixime sensitive with MIC < 0.016 µg/mL, intermediate susceptibility to penicillin with MIC of 0.125 µg/mL and resistance to ciprofloxacin with MIC of 4 µg/mL). With this treatment, the symptoms remitted and a considerable reduction in the inflammatory parameters was observed.
Infection by Neisseria gonorrhoeae is one of the primary causes of STIs. Disseminated infection is the most common complication and can occur in up to 3% of patients who acquire the infection and do not receive timely treatment.1–3
The mechanism by which disseminated infection occurs consists of a migration of the bacteria from a primary infection of the genital, anal or oropharyngeal mucosa; in the latter case, the primary infection is usually asymptomatic in up to 90% of patients. The main systemic manifestations of the disease are usually migratory polyarthralgia, tenosynovitis and fever, often accompanied by dermatitis, which is why it is often called arthritis-dermatitis syndrome.2,4,5
The diagnosis is made with the analysis of synovial fluid, which usually shows a cell count between 10,000 and 50,000/mm3, predominantly polymorphonuclear. In the Gram stain, the presence of cocci that are grouped in pairs (gram-negative diplococci) can guide the diagnosis. However, the final identification is made by culture, one of the most common being Thayer–Martin medium.3 Another method of microbiological identification ispolymerase chain reaction of samples of genital, anal or oropharyngeal mucosa. Treatment should be guided according to the antibiogram, although Neisseria gonorrhoeae usually has good susceptibility to third-generation cephalosporins, such as ceftriaxone and cefixime.6,7 However, it is worth noting that an increase in resistance to third-generation cephalosporins has been observed, with resistance rates of 8.7% reached in Europe between 2010 and 2013. In 2016, the resistance rate for cefixime in Spain was 1.6% and was 0.2% for ceftriaxone, while it was 57.5% for ciprofloxacin and 4.1% for azithromycin.8 The duration of treatment can vary between 7 and 10 days. Treatment of the partner or sexual contacts is essential to avoid reinfection.
This case, in addition to being a rare presentation of Neisseria gonorrhoeae infection, highlights the need for an active search for STIs, even in the absence of genitourinary manifestations. In summary, gonococcal arthritis should be considered as a differential diagnosis in adults of any age group but mainly in those of active sexual age, with migratory polyarthritis and fever and with risky sexual relations (unprotected) or previous STI.