This was a 49-year-old woman with a history of type 2 diabetes mellitus, former injecting drug user, CDC stage A2 human immunodeficiency virus (HIV) infection with adequate immunological and virological control and undetectable viral load, treated hepatitis C virus infection in cirrhotic stage with portal hypertension and oesophageal varices, and splenectomy following trauma with subsequent pneumococcal vaccination. Two months prior to the current admission, the patient had pneumococcal sepsis with joint involvement affecting the shoulder and hip, for which she received three weeks of meropenem (1g every 8h) followed by four weeks of oral amoxicillin (1g every 8h); other foci were ruled out by transthoracic echocardiogram and computed tomography (CT).
The patient went to the Accident and Emergency department with a three-day history of neck pain with paraesthesia in the upper limbs and chills. On physical examination, she had a fever of 38.7°C and pain on bilateral cervical paravertebral palpation without associated neurological abnormalities. Blood tests showed C-reactive protein of 17mg/dl, 18,000 leucocytes/microlitre and sedimentation rate raised to 120mm. After extraction of blood and urine cultures, she was started on treatment with intravenous meropenem 1g every 8h.
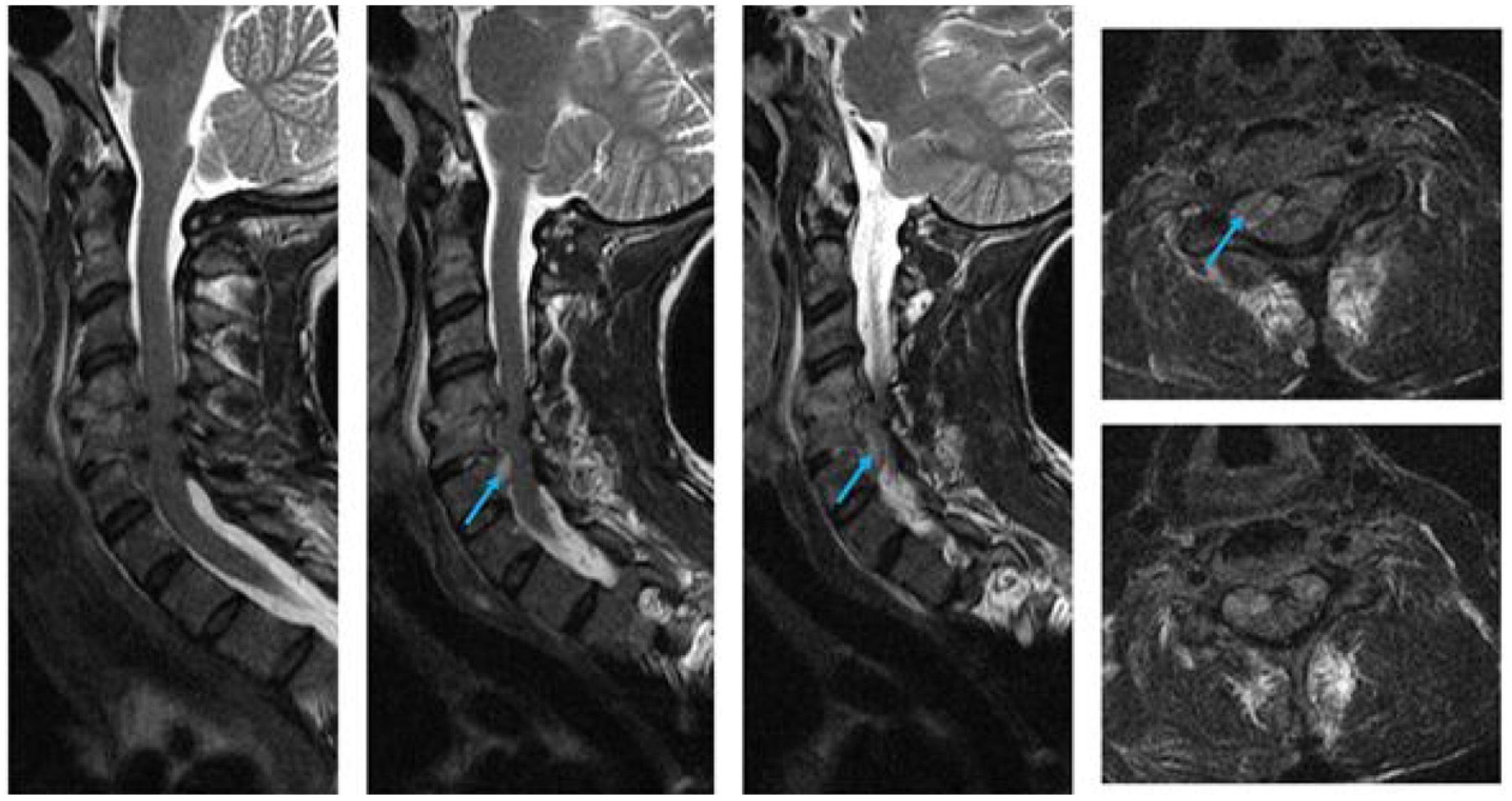
ProgressLateral neck X-ray (Fig. 1) showed loss of height between the C4–C5 spaces and the computed tomography scan revealed irregularity of the C4 and C6 endplates as well as soft tissue enlargement obliterating the anterior epidural space. Investigations were completed with MRI of the neck (Fig. 2), which revealed C4–C6 spondylodiscitis with two associated anterior epidural abscesses.
Twenty-four hours later, Gram-positive cocci were identified in chains that were subsequently identified as Streptococcus pneumoniae susceptible to penicillins and cephalosporins, so antibiotic therapy was optimised to intravenous ceftriaxone 2g every 24h. Transthoracic echocardiogram ruled out infective endocarditis. In the absence of neurological symptoms, surgery was not considered, opting to maintain antibiotic therapy for six weeks. The patient’s condition resolved, both clinically and radiologically, with no subsequent recurrence at the two-year follow-up.
DiscussionStreptococcus pneumoniae is a microorganism commonly involved in upper and lower respiratory tract and ear, nose and throat infections. In some cases it can develop into invasive pneumococcal disease (IPD), defined as the isolation of S. pneumoniae in sterile tissues or fluids. The risk factors for IPD are: being male; being under the age of two years or over 65; having chronic disease (cardiovascular, hepatic, renal or pulmonary); diabetes mellitus; and immunosuppression.1 Our patient was asplenic and had cirrhosis, HIV infection and diabetes mellitus.
Spondylodiscitis is infection of the vertebral body and/or adjacent bodies, with its pathogenesis based predominantly on haematogenous spread from a distant focus, although other known aetiologies are direct inoculation or contiguous spread from adjacent tissues. The most common location is lumbar (58%), followed by thoracic (30%) and cervical (11%).2
In our case, an extension study had been performed during the patient's previous admission, looking for other infectious metastatic foci with an echocardiogram and abdominal CT. We cannot therefore completely rule out that there was not a prior asymptomatic incipient cervical focus which manifested later. A broader extension study could be useful in such complex cases with metastatic involvement at different levels in order to optimise therapeutic management.
The most common microorganism to be isolated in spondylodiscitis is Staphylococcus aureus (50%), followed by Gram-negative and coagulase-negative staphylococci.3 In contrast, S. pneumoniae is an unusual causal agent in spondylodiscitis, with very few reports in the literature, the lumbar region being the most common location. Only 10–30% affect the cervical region, which makes our case even more unusual.3
The most common symptoms of spondylodiscitis are pain in the lower back, mid back or neck accompanied by fever and, on occasions, sensory or motor disturbances, particularly in the case of associated abscesses. Magnetic resonance imaging is the gold standard for locating and characterising these abscesses.3
The diagnosis of spondylodiscitis should be completed with a transthoracic echocardiogram to rule out endocarditis and cultures of blood and/or of the lesion in order to establish the causative agent and thus optimise antibiotic therapy.1
Initiating empirical antibiotic therapy will be determined by whether the patient has sepsis, neurological symptoms or immunosuppressive factors, as in our case. Treatment should be maintained for six to eight weeks, depending on how the patient progresses, and if the patient's condition deteriorates despite antibiotic therapy, surgery should be considered.2
With our case, we opted for an intravenous regimen for six weeks to ensure treatment compliance, due both to concern about lack of adherence to the oral antibiotic therapy regimen and the persistence of positive cultures for S. pneumoniae. After the treatment, the patient was followed up for two years, with no signs of recurrence of S. pneumoniae infection.
In conclusion, we need to be aware that, although unusual, infectious spondylodiscitis can affect the cervical segment. This makes it essential to perform an exhaustive microbiological study in order to identify very unlikely aetiological agents, such as S. pneumoniae, and thus optimise the most appropriate antibiotic therapy.