Rickettsial diseases transmitted by ticks in Spain are usually classified into three groups: Mediterranean button fever (MBF), caused by Rickettsia conorii subsp. conorii; MBF-like, similar to the MBF but produced by other rickettsiae; and dermacentor-borne necrosis erythema and lymphadenopathy (DEBONEL), produced mainly by Rickettsia slovaca or other species.1–3 Due to their difficult diagnosis, the relationships of the traditionally known rickettsiae are not clearly known. However, new molecular biology techniques have made it possible to identify more species.
We present a case in Madrid of lymphangitis-associated rickettsiosis (LAR), a variant of the MBF-like clinical picture, caused by rickettsia sibirica mongolitimonae.
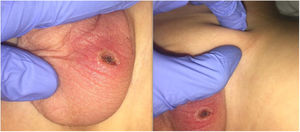
The patient was a five-year-old boy brought to the emergency room for left testicular pain of three days duration. His parents reported a tick bite five days earlier on the scrotum, with the formation of a scab and discharge, as well as a mild fever for two or three days. The family live in a rural area (Illescas) and lately they have observed ticks on their dog. On physical examination, the patient presented a fever of 38.6 °C and a crusty lesion with surrounding erythema and sublesional swelling, without fluctuation in the scrotum of the left testicle, associated with an ipsilateral inguinal adenopathy, hard, painful on palpation and without erythema (Fig. 1). The blood test showed: C-reactive protein 36.1 mg/l, GOT 68 U/l and GPT 73 U/l.
WIth the suspicion of a superinfection of the bite, the patient was admitted and treated with intravenous amoxicillin-clavulanate. At 12 h after admission, a generalised, erythematous, maculopapular rash appeared without palmoplantar involvement. Due to the possibility of rickettsiosis, a short course of intravenous doxycycline was started (2.2 mg/kg/dose every 12 h for 36 h). The fever was controlled in 24 h and the lesions progressively disappeared.
For the aetiological diagnosis, a sample of the crust was collected and sent to the Centro de Investigación Biomédica de la Rioja (CIBIR) [Biomedical Research Centre of La Rioja], where a polymerase chain reaction (PCR) test was carried out. Bands compatible with infection by Rickettsia of the group of spotted fevers were detected, using as targets fragments of the ompA and ompB genes (conventional PCR), and 23S rRNA (real-time PCR). Definitive identification was obtained by molecular sequencing of ompA and ompB (491 and 464 bp, respectively), which revealed a 100% identity match with Rickettsia sibirica subsp. mongolitimonae. Serology tests for Borrelia burgdorferi and Rickettsia conorii were negative.
LAR is a variant of MBF-like, with maximum incidence in spring and summer. Cases have been described in Europe and Africa, the majority being found in France, Spain and Portugal.1 However, there is little reference to this pathology in paediatric patients.
There is no clinical-aetiological correlation to a specific rickettsia subtype, since it can be caused by several, including Rickettsia sibirica mongolitimonae, transmitted by the tick of the genera Rhipicephalus and Hyalomma.2–4 The symptoms are regional adenopathies (with or without lymphangitis), fever and a discrete maculopapular rash. Clinically, it can be confused with DEBONEL due to the presence of crust and adenopathy, but this affects the upper half of the body and does not usually present with fever.2,3 In most cases, it constitutes a mild condition, although complications such as myopericarditis, encephalitis, septic shock, etc. have been described.5,6
Diagnostic confirmation is carried out with PCR on blood or on crust material (more sensitive), allowing a rapid and specific diagnosis, or with indirect immunofluorescence, a more sensitive but slow test that requires seroconversion (two to three weeks).7
Given the clinical suspicion, treatment should be started empirically, pending the results. Regardless of the age of the patient, doxycycline continues to be the treatment of choice. Although it is contraindicated in children under eight years of age due to changes in the colouration and enamel of the teeth, the side effects are minimal if it is used in short cycles.8
There are different treatment regimens: the classic regimen – 2.2 mg/kg/dose every 12 h for 5–7 days; and short regimens – 2.2 mg/kg/dose every 12 h for 36 h, or 200 mg/dose every 12 h for 24 h (the latter used successfully in adults).2,9,10 Oral administration is the route of choice, especially if it is diagnosed in the first five days, reserving the intravenous route for severe cases.9 The new macrolides (azithromycin and erythromycin) can be considered an option, but they have shown less effectiveness.2
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Salazar Alarcón E, Guillén-Martín S, Callejas-Caballero I, Valero-Arenas A. A propósito de un caso: no toda rickettsiosis es fiebre botonosa mediterránea. Enferm Infecc Microbiol Clin. 2022;40:44–45.