The aim of this study was to describe the distribution of Streptococcus pneumoniae serotypes in isolates from pleural fluid in the Madrid Autonomous Community between the years 2007–2018.
MethodsInvasive pneumococcal disease strains isolated during the period 2007–2018 were studied. The frequency of serotypes from pleural fluid was compared with that observed in other samples.
ResultsA total of 6,115 pneumococcal invasive isolates were processed. Of them, 182 (3%) were isolated from pleural fluid. A total of 70.9% of isolates belonged to some of the following six serotypes: 1, 3, 19A, 8, 7F and 5. The serotypes 3 and 8 increased significantly from 9.6% to 30.8%, and from 5.3% to 20.5%, respectively, over the periods 2007−2010 to 2015−2018.
ConclusionsPneumococcal serotypes 3 and 8 are currently significant causes of infection of pleural fluid in our region.
El objetivo de este estudio es describir la distribución de serotipos de Streptococcus pneumoniae en aislados de líquido pleural en la Comunidad de Madrid (CM) entre los años 2007–2018.
MétodosSe estudiaron las cepas de episodios de enfermedad neumocócica invasora aisladas en la CM durante el periodo 2007–2018. La frecuencia de serotipos en líquido pleural se comparó con la observada en otras muestras.
ResultadosSe procesaron 6.115 cepas invasoras de neumococo. Ciento ochenta y dos (3%) se aislaron en muestras de líquido pleural. El 70,9% de los aislados pertenecía a alguno de los 6 siguientes serotipos: 1, 3, 19A, 8, 7F y 5. Los serotipos 3 y 8 aumentaron significativamente, pasando del 9,6% al 30,8%, y del 5,3% al 20,5%, respectivamente, entre los períodos 2007−2010 a 2015−2018.
ConclusiónLos serotipos 3 y 8 son actualmente causas importantes de infección del líquido pleural en nuestra área.
Invasive pneumococcal disease (IPD) is microbiologically defined as detection of Streptococcus pneumoniae in typically sterile clinical samples. Although there are many S. pneumoniae serotypes, only a limited number of them cause most infections. Distribution of pneumococcal serotypes varies by disease, the type of clinical sample studied and geographical region. S. pneumoniae causes a broad spectrum of diseases and represents a significant cause of empyema.1
The greater or lesser tropism of particular strains for pleural fluid can cause the frequency with which different serotypes are detected to vary in cases of empyema. Serotypes isolated in pleural fluid may be different depending on vaccination policies. The 7-valent pneumococcal conjugate vaccine (PCV7) to protect against serotypes 4, 6B, 9V, 14, 18C, 19F and 23F was placed on the Spanish market in 2001. In 2006, the Autonomous Community of Madrid added this vaccine to its childhood vaccination schedule, and in 2010, it replaced it with the PCV13 vaccine, which added serotypes 1, 3, 5, 6A, 7F and 19A to the PCV7 vaccine. In 2012, the PCV13 vaccine was removed from that vaccination schedule and continued to be recommended on an individual basis. In 2015, the Autonomous Community of Madrid re-added PCV13 to its childhood vaccination schedule.2
IPD is a reportable disease in the Autonomous Community of Madrid, and the Laboratorio Regional de Salud Pública [Regional Laboratory of Public Health] acts as a reference centre for serotyping and monitoring antibiotic susceptibility. The objective of this study is to report changes in the distribution of serotypes in isolates from pleural fluid and their tropism for this type of sample in patients of all ages in the Autonomous Community of Madrid between 2007 and 2018.
MethodsStrains from episodes of IPD were examined in samples sent by public and private hospitals in the Autonomous Community of Madrid to the Laboratorio Regional de Salud Pública between 2007 and 2018. Serotyping was performed by means of latex agglutination (Pneumotest-Latex) and the Quellung reaction, using specific antisera (Statens Serum Institut, Copenhagen, Denmark). Determination of antibiotic susceptibility to penicillin, erythromycin and levofloxacin was done by ETEST (bioMérieux, France) according to EUCAST criteria for interpretation3 (minimum inhibitory concentration [MIC] against penicillin ≤0.06mg/l susceptible and >2mg/l resistant; erythromycin ≤0.25mg/l susceptible and >0.5mg/l resistant and levofloxacin ≤0.001mg/l susceptible and >2mg/l resistant). The frequency of serotypes from pleural fluid samples was compared to that seen in other samples that are typically sterile (such as blood, cerebrospinal fluid, as citic fluid, synovial fluid, pericardial fluid, etc.) using the χ2 test and the odds ratio (OR) with a 95% confidence interval. Changes over time (across the four-year periods of 2007−2010, 2011−2014 and 2015−2018) were analysed using the χ2 test for linear trend.
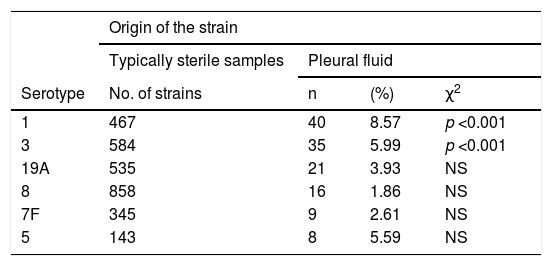
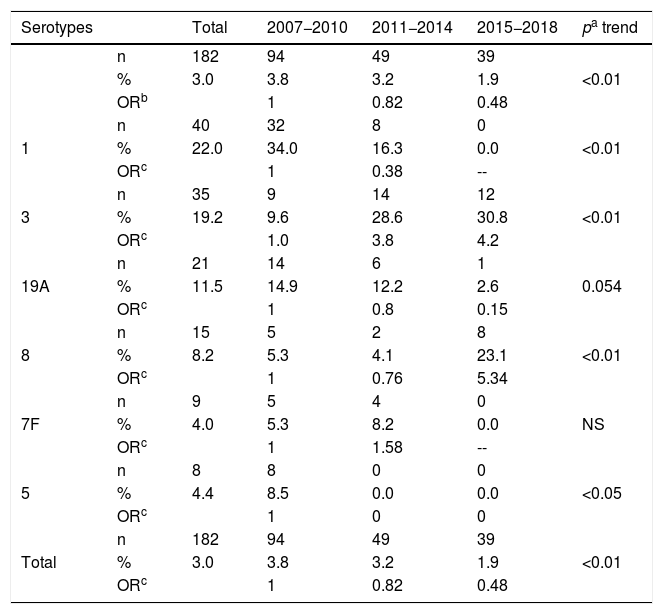
ResultsOf the 6,115 invasive pneumococcal strains that were processed, 182 (3%) were isolated in samples of pleural fluid (70 in children and 112 in adults). Of these strains, 95.6% were identified at the serotype level (27 different serotypes) and 4.4% were only identified at the serogroup level (3 different serogroups). In 70.8% of pleural fluid isolates, at least one of the following 6 serotypes were identified: 1 (22.0%), 3 (19.2%), 19A (11.5%), 8 (8.8%), 7F (4.9%) and 5 (4.4%). Among them, 2 serotypes appeared more frequently in pleural fluid than in other locations (p <0.001), with higher tropism for this location: 1 (OR: 3.63; 95% CI: 2.52–5.23) and 3 (OR: 2.33; 95% CI: 1.60–3.41). Table 1 shows the proportions of strains isolated in pleural fluid in the most common serotypes in this sample out of all cases of IPD. Serotypes 1, 3 and 5 were isolated in pleural fluid in more than 5% of all strains causing IPD. The total frequency of strains isolated in pleural fluid decreased over the course of the study period (p<0.001) (Table 2). Among the 6 most frequent serotypes, 1, 5, 19A and 7F decreased (there were no isolates of serotypes 1, 5 or 7F and only one isolate of 19A from 2015 to 2018) and the reduction in the frequency (in terms of proportions) achieved statistical significance in the first 2. Conversely, serotypes 3 and 8 showed a statistically significant increase in frequency (reaching percentages in pleural fluid of 30.8% and 23.1%, respectively, in 2015−2018). Both serotypes were isolated, particularly in adults (for serotype 3, 21 strains were isolated in adults out of a total of 35; for serotype 8, 14 strains were isolated in adults out of a total of 16).
The most common serotypes of Streptococcus pneumoniae isolated in pleural fluid in cases of invasive pneumococcal disease. Autonomous Community of Madrid 2007–2018.
| Origin of the strain | ||||
|---|---|---|---|---|
| Typically sterile samples | Pleural fluid | |||
| Serotype | No. of strains | n | (%) | χ2 |
| 1 | 467 | 40 | 8.57 | p <0.001 |
| 3 | 584 | 35 | 5.99 | p <0.001 |
| 19A | 535 | 21 | 3.93 | NS |
| 8 | 858 | 16 | 1.86 | NS |
| 7F | 345 | 9 | 2.61 | NS |
| 5 | 143 | 8 | 5.59 | NS |
Changes in the main serotypes of Streptococcus pneumoniae isolated in pleural fluid in cases of invasive pneumococcal disease. Autonomous Community of Madrid. 2007-2010, 2011-2014 and 2015-2018.
| Serotypes | Total | 2007−2010 | 2011−2014 | 2015−2018 | pa trend | |
|---|---|---|---|---|---|---|
| n | 182 | 94 | 49 | 39 | <0.01 | |
| % | 3.0 | 3.8 | 3.2 | 1.9 | ||
| ORb | 1 | 0.82 | 0.48 | |||
| 1 | n | 40 | 32 | 8 | 0 | <0.01 |
| % | 22.0 | 34.0 | 16.3 | 0.0 | ||
| ORc | 1 | 0.38 | -- | |||
| 3 | n | 35 | 9 | 14 | 12 | <0.01 |
| % | 19.2 | 9.6 | 28.6 | 30.8 | ||
| ORc | 1.0 | 3.8 | 4.2 | |||
| 19A | n | 21 | 14 | 6 | 1 | 0.054 |
| % | 11.5 | 14.9 | 12.2 | 2.6 | ||
| ORc | 1 | 0.8 | 0.15 | |||
| 8 | n | 15 | 5 | 2 | 8 | <0.01 |
| % | 8.2 | 5.3 | 4.1 | 23.1 | ||
| ORc | 1 | 0.76 | 5.34 | |||
| 7F | n | 9 | 5 | 4 | 0 | NS |
| % | 4.0 | 5.3 | 8.2 | 0.0 | ||
| ORc | 1 | 1.58 | -- | |||
| 5 | n | 8 | 8 | 0 | 0 | <0.05 |
| % | 4.4 | 8.5 | 0.0 | 0.0 | ||
| ORc | 1 | 0 | 0 | |||
| Total | n | 182 | 94 | 49 | 39 | <0.01 |
| % | 3.0 | 3.8 | 3.2 | 1.9 | ||
| ORc | 1 | 0.82 | 0.48 |
Among the 182 strains isolated in pleural fluid, 37 (20.3%) demonstrated intermediate susceptibility to penicillin and 3 (1.6%) were resistant to it; 2 (1.1%) presented intermediate susceptibility to erythromycin and 47 (25.8%) were resistant and, lastly, 8 (4.4%) were resistant to levofloxacin. Of the isolates of serotype 19A, 20 (95.2%) were not susceptible to penicillin (13 of them [61.9%] were isolated in 2007−2010 and only 1 [4.8%] was isolated in 2015−2018), and all were resistant to erythromycin. In serotype 8, 4 (25.0%) of the strains were resistant to erythromycin and 3 (18.8%) of the strains were resistant to levofloxacin.
DiscussionIn the era prior to the use of conjugate vaccines (1997–2000), the serotypes covered by PCV7 accounted for half to one-third of isolates in pleural fluid in Spain. During the PCV7 post-marketing period (2001–2008), Spain saw a significant decrease in these serotypes in pleural fluid and an increase in others, such as 1, 3 and 19A,4 which were not included in PCV7 but were included in PCV13 and seem to show a marked tropism for pleural tissue.5 Other serotypes covered by PCV13, such as 5 and 7F, have also been predominant in this type of infection.6 In the pre-PCV13 era, the serotypes included in this vaccine represented the most common cause of paediatric parapneumonic effusion.5,7 After PCV13 was introduced, a reduction in pleural fluid infection occurred with a drop in these vaccine serotypes and a rising trend among non-vaccine serotypes,8 with there being no clear replacement at that time.5
This study showed a drop in levels of pneumococcal infection in pleural fluid since 2007. Six serotypes (1, 3, 19A, 8, 7F and 5) accounted for more than 3/4 of isolates in pleural fluid in the study period. The changes in serotypes 1 and 3 are of great significance, given that both showed higher tropism for this location. Serotype 1 presented a very marked decrease following the introduction of PCV13: it went from accounting for 1/3 of cases in 2007−2010 to accounting for no cases in 2015−2018. The significant decrease in this serotype in pleural fluid infections has also been seen in other studies.8 Another declining serotype is serotype 5, which disappeared in 2011, perhaps due to cyclical epidemic factors and not merely as a direct result of the vaccine.9 On the other hand, the increase in serotype 3 is striking, as it increased in frequency despite being included in the PCV13 vaccine. Some studies have suggested that PCV13 has limited efficacy against this serotype,10 which could have accounted for this trend somehow.
Although, all things considered, a general decrease in levels of pneumococcal infection in pleural fluid has been seen since 2007, with a significant decrease in the frequency of serotype 1, the increase in serotypes 3 and 8 (with the 2 accounting for half of cases in 2015−2018) is an problem that deserves attention. These 2 serotypes have a high incidence in the Autonomous Community of Madrid, particularly among adult patients.3 It should be noted that serotype 19A isolates in pleural fluid have a high rate of resistance to erythromycin and non-susceptibility to penicillin. This can make them more difficult to treat. Fortunately, the frequency of this serotype has been decreasing since PCV13 was introduced. That which is seen in pleural fluid is comparable to that which is seen in IPD in general, with a decrease associated with elimination of vaccine serotypes and an increase in other non-vaccine serotypes such as serotype 8.
Conflicts of interestJCS has attended conferences funded by Pfizer.
Please cite this article as: Sanz JC, Miguel S, Ordobás M, García Comas L. Evolución de la distribución de serotipos de Streptococcus pneumoniae aislados en líquido pleural en la Comunidad de Madrid entre los años 2007 y 2018. Enferm Infecc Microbiol Clin. 2021;39:25–28.