Six years ago, we had the honour of publishing a review in Enfermedades Infecciosas y Microbiología Clínica under the title “Utilidad de los biomarcadores de inflamación e infección en los servicios de urgencias” [Usefulness of inflammation and infection biomarkers in the Emergency Department].1 The goal of this review was to set out the published scientific evidence, clarify existing points of debate, compare the usefulness of the main inflammation and infection biomarkers (IIBMs) and, based on these, produce a number of recommendations for the use thereof in order to improve the diagnosis, prognostic assessment and management of patients with infection in the emergency department. The different models for predicting bacteraemia published up to then were also reviewed, from the most widely used and validated in emergency departments (EDs), such as that by Shapiro et al.,2 to other simpler ones that have also been used and even validated following the publication of the review, such as that by Cuervo et al.3 However, we then concluded that it was necessary to continue the search for a more useful bacteraemia model that was easier to obtain in patient care in EDs, so that it could be implemented in regular clinical practice.1 In the same way, reference was made to different considerations in indicating and acquiring blood cultures in EDs. Although even today there are no definitive answers to all the questions that were raised back then, there has indeed been significant progress, just as we sought back then and continue to do so now,4 through collaborative efforts from scientific associations in the fields of emergency medicine and infectious disease with shared problems, language and realities.5
The end of that review highlighted, in one of its concluding remarks, that, in the near future, other variables, including IIBMs,6 would eventually be incorporated into the classic models used almost exclusively up to then, such as that by Shapiro et al.2 In this vein, following six years of research, procalcitonin (PCT) can be said to have filled a significant gap in the latest predictive models published, which are better able to offer a prognosis as to the presence of bacteraemia7; this has been acknowledged by various authors who, in recent articles, have individually investigated predictive factors for bacteraemia. For these, the finding of a PCT level ≥0.51 ng/ml yielded the best prognostic performance among the different variables analysed, with an odds ratio of 4.52 (95% confidence interval [CI]: 4.20–4.84, p < 0.001).8 Similarly, in articles comparing the results of several IIBMs for predicting sepsis and bacteraemia in patients diagnosed with serious infection in EDs,9,10 PCT yielded a similar performance for the diagnosis of sepsis than, for example, presepsin. However, its power was significantly superior to presepsin for predicting bacteraemia in blood cultures obtained in the ED from patients with suspected serious infection.4,9 All this has enabled the development and validation in a recently published study of a predictive model for bacteraemia with five variables (“5MPB-Toledo”).7 The model includes temperature >38.3 °C (1 point), Charlson Comorbidity Index ≥3 (1 point), respiratory rate ≥22 respirations per minute (1 point), leukocyte count >12,000/mm3 (1 point) and PCT ≥0.51 ng/ml (4 points). Patients are categorised as low-risk (0–2 points), moderate-risk (3–5 points) or high-risk (6–8 points), with a likelihood of bacteraemia of 1.1%, 10.5% and 77%, respectively. The area under the curve of the receiver operating characteristic (AUC-ROC) for the model following re-sampling was excellent: 0.946 (95% CI: 0.922–0.969).
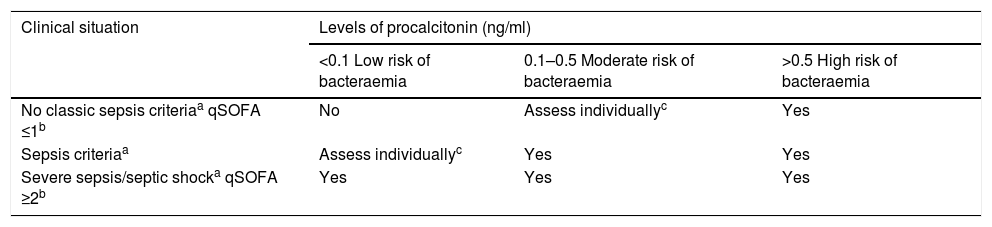
Therefore, as suspicion of bacteraemia from EDs is extremely important for patients and for the system (taking blood cultures, administering suitable antimicrobials early, deciding to admit or to discharge, etc.),4 we have updated the recommendations published six years ago in the above-mentioned review1 (Table 1), taking into consideration new cut-off points chosen for PCT and definitions of sepsis (classic definitions and Sepsis-3, used in EDs).5 Thus, “six years later”, we continue to make progress and we shall carry on conducting research for the benefit of our patients.
Recommendations for taking blood cultures in emergency departments by likelihood of bacteraemia.
| Clinical situation | Levels of procalcitonin (ng/ml) | ||
|---|---|---|---|
| <0.1 Low risk of bacteraemia | 0.1–0.5 Moderate risk of bacteraemia | >0.5 High risk of bacteraemia | |
| No classic sepsis criteriaa qSOFA ≤1b | No | Assess individuallyc | Yes |
| Sepsis criteriaa | Assess individuallyc | Yes | Yes |
| Severe sepsis/septic shocka qSOFA ≥2b | Yes | Yes | Yes |
Adapted from Reference 6.
Sepsis criteria: systemic inflammatory response syndrome (SIRS) plus infection. SIRS with two of the following four criteria: temperature >38 °C or <36 °C; leukocytosis >12,000 or <4000/mm3 or >10% band cells; tachypnoea >20 respirations per minute (rpm) or PaCO2 <32 mmHg; and tachycardia >90 beats per minute. Severe sepsis: sepsis with organ dysfunction, hypotension or hypoperfusion (hyperlactacidaemia). Septic shock: persistent hypotension despite fluid replacement requiring vasopressors.
No funding was received for this work.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rubio Díaz R, Nieto Rojas I, Julián-Jiménez A. Importancia de la predicción de bacteriemia en los servicios de urgencias: seis años después. Enferm Infecc Microbiol Clin. 2021;39:109–110.