Periprosthetic joint infections (PJI) usually cause the failure of the implant. Apart from some virulent microorganisms associated to early infection, anaerobes are a main cause of late infection. Parvimonas micra (P. micra) is a fastidious, slow-growing, Gram-positive anaerobic cocci normally found in the oral cavity and gastrointestinal tract.1P. micra has been identified as a cause of oral infections.1 Recently, this pathogen has been increasingly isolated in other infections (spondylodiscitis,2 endocarditis,3 meningitis,4 among others). Here we present a case of P. micra knee arthroplasty infection without fever and systemic infection but with the presence of local pain.
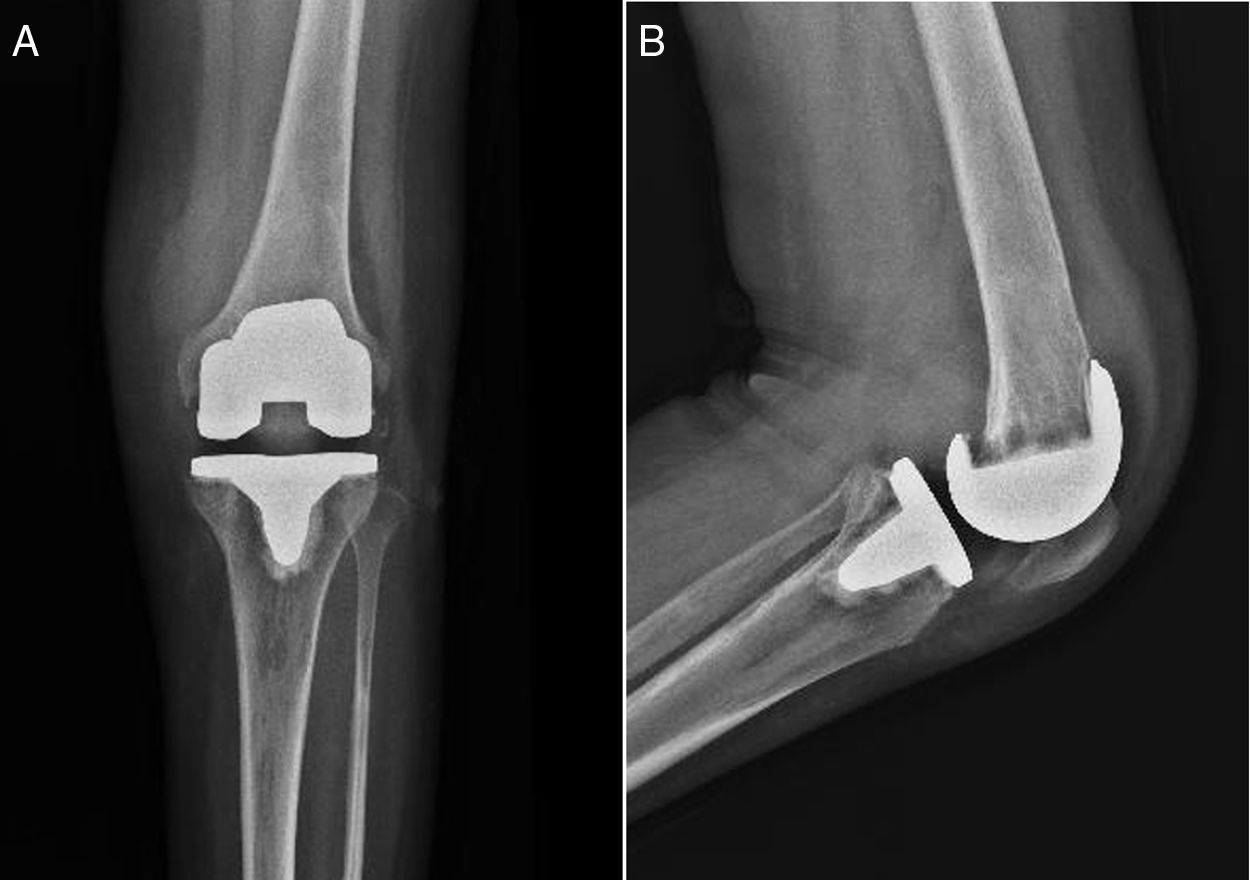
A 39-year-old woman presented at the Trauma and Orthopedic Surgery Department with an 8-week history of severe progressive swelling and pain of the left knee. Her medical record revealed a rheumatoid arthritis (RA) for 7 years, arthritis and bone destruction of the left knee with treatment of a left total joint replacement 3 years ago. She endured several treatments for RA, by taking oral drugs such as hydroxychloroquine sulfate, methylprednisolone and iguratimod. Palpation was painful at the lateral joint space. Flexion/extension of the knee was 0-0-90 degrees. Blood examination showed leucopenia with an inflammatory syndrome. Her white cell count was 3.50×109/L (4.0–10.0×109/L), with both high C-reactive protein level (18mg/L) and erythrocyte sedimentation rate (70mm/h). X-ray studies revealed a postoperative state of arthroplasty (Fig. 1A and B). Joint fluid obtained was bloody, introduced both in aerobic and anaerobic blood culture bottles and sent to the laboratory for analysis by using an automated blood culture system (Becton Dickinson, USA). Only the anaerobic bottle (pre-reduced anaerobically sterilized medium including yeast extract, vitamin K and mercaptan) was positive within 24h. Then, the sample from the anaerobic bottle was inoculated into two blood agar plates (OXOID, England). One plate was incubated aerobically (5% CO2), and another anaerobically (in anaerobic bags), for 48h. A single colony of a small Gram-positive cocci was isolated on the anaerobic blood agar. Then, this colony was identified by the Vitek-compact 2 automatized system (bioMérieux, France), and results were consistent with these obtained by MALDI-TOF MS (Autobio, Zhengzhou, China) (P. micra, score 9.594). The isolate was initially suspected to be a contaminant, until the organism obtained from the culture of joint fluid inspected next day showed the same result and it was the only organism isolated from the sample. Subsequently, P. micra was identified by 16S rRNA gene sequence analysis (GenBank No. NR_114338.1, 100%). Cultures for aerobic bacteria and fungi remained negative for five days. The patient was treated with antibiotics and surgical debridement and was discharged 2 weeks later.
Anaerobic organisms as the monomicrobial etiology of joint infections are really rare. In the past, growth of anaerobic bacteria was often difficult to obtain given the limitations in our conventional culture protocol. Furthermore, previous antibiotic therapy is often received by a proportion of patients prior to hospitalization, further decreasing the culture yield.5 Several studies have shown that the selection of appropriate enrichment media such as thioglycollate broth is helpful and necessary for the isolation of bacteria, especially anaerobic bacteria.6,7 In this patient, anaerobic cultures showed growth of P. micra, which was identified by Vitek-compact 2 analysis, MALDI-TOF MS, and 16S rRNA sequencing,8,9 demonstrating the etiology of the infection. The patient presented with only local swelling and pain but no fever, and the low cell count might be due to the low-grade infection or weak virulence of the anaerobe. However, the limitations of conventional culture without the use of an enrichment broth can increase the risk of false negative results, and prolonged incubation is necessary when using conventional media. Moreover, conventional culture media needs to be enriched in order to obtain more efficient results and to shorten the incubation time. In addition, appropriate sample collection is essential for the recovery of the organisms in culture. Apart from synovial fluid, other samples including tissue biopsies are important for the diagnosis of prosthetic joint infection. Especially, periprosthetic tissue is a valuable sample for the detection of the causative organism.10 The culture of different samples is also helpful for the best release of bacteria.7 In conclusion, we present a patient with a prosthesis septic infection of the knee caused by P. micra. A reference culture method including appropriate media and time of incubation as well as an adequate sample preparation should be established in order to confirm an infection caused by anaerobic bacteria.
FundingThis reported study was supported by research grant from the National Natural Science Foundation of China (No. 81703830).