There are no guidelines to screen haemato-oncologic children when a tuberculosis (TB) outbreak is suspected.
MethodsAfter exposition to an adult with active TB, children exposed from a haemato-oncology unit were screened according to immunosuppression status and time of exposure. Until an evaluation after 8–12 weeks from last exposure, isoniazid was indicated to those with negative initial work-up.
ResultsAfter 210 interventions, we detected a case of pulmonary TB, and another with latent TB infection. Pulmonary findings and treatment approach were challenging in some patients.
ConclusionsThe TB screening of oncologic children required a multidisciplinary approach, and clinicians managed challenging situations.
No existen pautas para el cribado de niños hematooncológicos cuando se sospecha de un brote de tuberculosis (TB).
MétodosDespués de la exposición a un adulto con TB activa, se evaluó a los niños expuestos de una unidad de hematooncología según el estado de inmunosupresión y el tiempo de exposición. Hasta una evaluación después de ocho a12 semanas desde la última exposición, se indicó isoniazida para aquellos con un proceso inicial negativo.
ResultadosTras 210 intervenciones se detectó un caso de tuberculosis pulmonar y otro con infección por TB latente. Los hallazgos pulmonares y el método de tratamiento fueron un desafío en algunos pacientes.
ConclusionesEl cribado de TB en niños oncológicos requirió un método multidisciplinario y los médicos manejaron situaciones complejas.
According to the nature of tuberculosis (TB), the risk of transmission can be stratified depending on the exposition, contagiousness of index case and contact susceptibility.1 Regarding susceptibility, immunocompromised patients and children have an increased risk of developing severe disease.
Although existing guidelines are useful to design a strategy when a TB case is diagnosed, there is no specific approach for exposed children with haemato-oncological conditions.1,2
The aim of this report is to describe our experience when the mother of a patient admitted to a paediatric haemato-oncology unit was diagnosed with active pulmonary TB and the medical actions derived from this situation.
Material and methodsA 28-year-old woman from Honduras was diagnosed with smear-positive pulmonary TB while her daughter was an inpatient receiving chemotherapy for a low-grade glioma. She had previously accompanied her daughter to all medical visits. Therefore, once diagnosed, all the clinic days, daycare visits and admissions of her daughter, for the previous 3 months, were tracked.1 All potential exposed patients were detected.
Following guidelines1 adapted to inhospital exposure, patients were stratified into different “exposure circles”: circle 1, if the patient had shared more than 8h of cumulative exposure in the same enclosed space (ward or outpatient clinic) and circle 2, if the child had shared less than 8h or had been admitted simultaneously but in a different room. In case it was not possible to precise the time of exposure for each patient in the same enclosed space with the index case, that patient was considered from circle 1. A high-risk (HR) group included those patients receiving active immunosuppressive therapy during exposure. Children included in circle 1 and/or HR group were immediately studied; those from circle 2, and not included in the HR group, were screened once evaluation of circle 1 was completed.
All patients underwent a medical interview, physical examination, tuberculin skin test (TST), interferon-gamma release assay (IGRA) (QuantiFERON® TB Gold In-Tube-QFT-GIT-, Cellestis, Ltd.) and chest X-ray. Tests were repeated 8–12 weeks after last exposure, when first evaluation had been performed before 8 weeks. A cut-off value of 5mm was considered positive for TST in this cohort.
The study of potential exposition/infection of healthcare workers and patients’ relatives was delegated on the Department of Occupational Medicine and Public Health. Results are not included in this study.
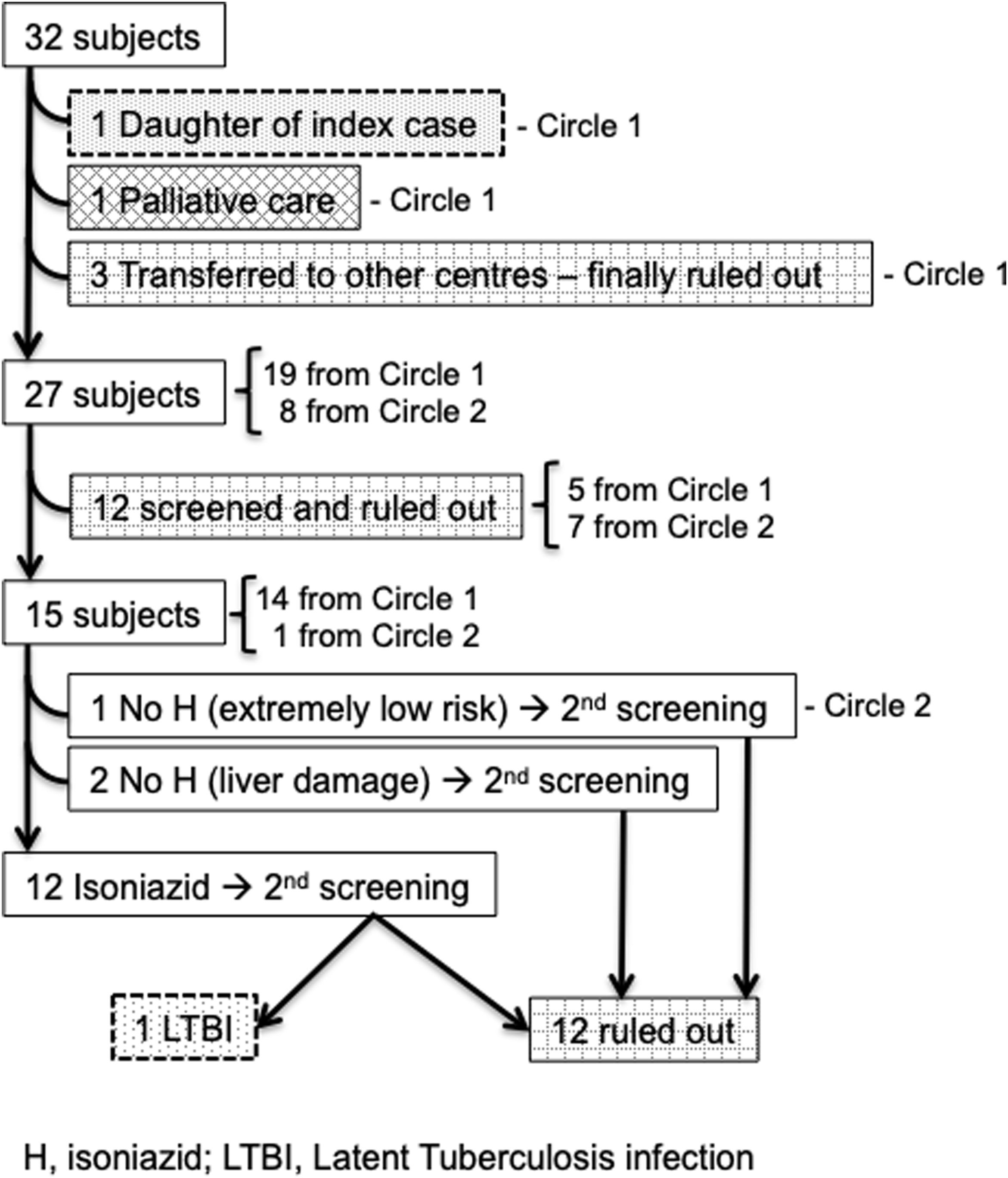
ResultsThirty-two patients were considered for screening. Synopsis of demographics and results of diagnostic tests are included in Table 1. All cases were HIV negative. The screening flowchart is shown in Fig. 1.
Socio-demographic, clinical and tuberculosis screening data of patients.
| Patient | Age (years) | Baseline diagnosis | First TST (mm) | First QFT | First chest X-ray | Time until evaluation (1st/2nd)** | Second TST (mm) | Second QFT | Second chest X-ray | Final diagnosis | Comments |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 12 | Low grade glioma | 15 | I | Infiltrate in lung | 1/NP | NP | NP | NP | Pulmonary TB | Daughter of index case |
| 2* | 7 | B-cell ALL | 0 | N | Normal | 5/11 | 6 | N | Normal | TB contact – LITB | H until 2nd, then Tx |
| 3* | 2 | B-cell ALL | 0 | I | Normal | 5/10 | 0 | N | Normal | TB contact | No prophylaxis due to hepatitis |
| 4* | 11 | HLH | 0 | N | Normal | 4/9 | 0 | N | Normal | TB contact | No prophylaxis due to hepatitis |
| 5* | 13 | Classic HL | 0 | N | Normal | 2/10 | 0 | N | Normal | TB contact | H until 2nd |
| 6* | 2 | B-cell ALL | 0 | N | Normal | 4/12 | 0 | N | Normal | TB contact | H until 2nd |
| 7* | 3 | Medulloblastoma | 0 | N | Normal | 3/11 | 0 | N | Normal | TB contact | H until 2nd |
| 8* | 3 | CMMRD, T-cell ALL | 0 | N | Normal | 4/11 | 0 | N | Normal | TB contact | H until 2nd |
| 9* | 3 | B-cell ALL | 0 | N | Normal | 3/11 | 0 | N | Normal | TB contact | H until 2nd |
| 10 | 4 | LCH | 0 | N | Normal | 6/14 | 0 | N | Abnormal→Normal | TB contact | H until 2ndInfiltrate resolved with antibiotics |
| 11 | 6 | Burkitt lymphoma | 0 | N | Normal | 7/11 | 0 | N | Normal | TB contact | H until 2nd |
| 12 | 3 | B-cell ALL | 0 | N | Normal | 5/11 | 0 | N | Normal | TB contact | H until 2nd |
| 13 | 13 | Thyroid Ca | 0 | N | Normal | 3/9 | 0 | N | Normal | TB contact | H until 2nd |
| 14 | 4 | Pilocytic astrocitoma | 0 | N | Normal | 10/NP | NP | NP | NP | TB contact | – |
| 15 | 5 | B-cell ALL | 0 | N | Normal | 11/NP | NP | NP | NP | TB contact | – |
| 16 | 5 | Burkitt lymphoma | 0 | N | Normal | 14/NP | NP | NP | NP | TB contact | – |
| 17 | 2 | Neuroblastoma | 0 | N | Normal | 7/11 | 0 | N | Normal | TB contact | H until 2nd |
| 18 | 2 | Pro-B LLA | 0 | N | Normal | 7/13 | 0 | N | Normal | TB contact | H until 2nd |
| 19 | 14 | Classic HL | 0 | N | Nodule | 8/NP | NP | NP | NP | TB contact | Nodule due to oncological process |
| 20 | 1 | Cerebellar tumour | 0 | N | Normal | 12/NP | NP | NP | NP | TB contact | – |
| 21* | 4 | Pre-B B-cell LLA | 0 | N | Normal | 5/12 | NP | N | Normal | TB contact | Transferred to other hospital |
| 22* | 7 | B-cell ALL | NP | N | Normal | 2/15 | NP | N | Normal | TB contact | Transferred to other hospital |
| 23* | 6 | B-cell ALL | NP | N | Normal | 7/14 | NP | N | Normal | TB contact | Transferred to other hospital |
| 24* | 7 | Ependymoma | NP | NP | NP | NP/NP | NP | NP | NP | TB contact | Palliative care |
| 25* | 14 | B-cell ALL | 0 | N | Normal | 3/11 | NP | N | Normal | TB contact | No Px due to minimum risk for isolation |
| 26* | 13 | CIDP | 0 | N | Normal | 9/NP | NP | NP | NP | TB contact | – |
| 27* | 9 | Nephrotic Sd. | 0 | N | Normal | 12/NP | NP | NP | NP | TB contact | – |
| 28 | 2 | SCD | 0 | N | Normal | 10/NP | NP | NP | NP | TB contact | – |
| 29 | 12 | SCD | 0 | N | Normal | 12/NP | NP | NP | NP | TB contact | – |
| 30 | 12 | Burkitt ALL | 0 | N | Normal | 12/NP | NP | NP | NP | TB contact | – |
| 31 | 3 | ITP | 0 | N | Normal | 11/NP | NP | NP | NP | TB contact | – |
| 32 | 11 | SCD | 8 | N | Normal | 14/NP | NP | NP | NP | TB contact | BCG vaccine, negative QFT |
Above slashed line, are patients who belonged to circle 1 (>8h with index case).
I, indeterminate; N, negative; NP, not performed; H, isoniazid; ALL, acute lymphoblastic leukaemia; HLH, hemophagocytic lymphohistiocytosis; HL, Hodgkin lymphoma; LCH, Langerhans cell histiocytosis; CIDP, chronic inflammatory demyelinating polyneuropathy; ITP, idiopathic thrombocytopenic purpura; SCD: sickle cell disease; LITB, latent tuberculosis infection; Tx, treatment; Px: prophylaxis.
The daughter of the index case presented a positive TST (15mm), an indeterminate IGRA result, an infiltrate in the chest X-ray and she was diagnosed with pulmonary TB; no TST was performed before chemotherapy started. Her chemotherapy was withheld while she received treatment against TB.
After second evaluation, a patient with an intermediate risk B-cell acute lymphoblastic leukaemia turned a previous negative TST to positive. IGRA tests were negative and chest X-rays were normal, so he was diagnosed of latent tuberculosis infection (LTBI) and received isoniazid for 6 months; study of householders was negative for TB. He continued chemotherapy as scheduled. He was part of circle 1 and from the HR group.
In 2 cases chest X-ray evaluations were challenging: 1 patient with Hodgkin lymphoma presented a pulmonary nodule (a later biopsy revealed progression of his underlying disease), and another patient's chest X-ray evaluation was performed during an episode of fever and neutropenia and showed an infiltrate, with a complete resolution after the febrile episode.
Screening with TST before immunosuppressive treatment had been performed in 16/28 (57%) (14/26 – 54% – of those with haemato-oncological diagnosis) and none of them had screening with IGRA. No adverse events were reported related to TB medication. Finally, 210 hospital activities were necessary, including 84 interviews throughout 4 months.
DiscussionDiagnosing TB in a patient with immunosuppression is challenging, especially in paediatric population.1,3–6 Stefan et al. described discordant results when using 3 different tests (TST and two IGRA methods: T-SPOT.TB and QFT-GIT) to rule out TB in a group of 34 oncological children. They prompted to combine different tests to confirm or rule out infection, due to discrepancies between cases.6 Carvalho et al. stated that T-SPOT is more accurate to identify TB infection when compared to QFT-GIT in children with lymphocytopenia, after testing 18 patients with this condition.4 In our case, T-SPOT was not available, so we decided to use TST, QFT-GIT and chest X-ray, given the aforementioned difficulties in this population.
Erkens et al. suggested to stratify contacts in circles given the time shared in the same enclosed space with a source case and encouraged to evaluate these contacts prioritizing by personal conditions, as an increased risk for developing TB after infection.1 This is the rationale we used to stratify patients and prioritize their screening. It was impossible to ascertain the time of exposure, so we considered one day of shared visit (if admitted or sharing waiting room/treatment room in daycare) as spending at least 8h sharing an enclosed space and we investigated them as in the Italian cohort.4 We differentiated urgent screening or to be done as soon as possible, according to individual risk. This implied a considerable use of resources in a short period of time, so planning rationally from the beginning was crucial.
The importance of ruling out TB infection after exposure to an index case in this population is out of discussion, not only because of the patient's personal benefit but also because of the potential risk of dissemination.1,3,4,6,7 In our cohort, we detected a case of LTBI and there are other cases of TB infection after inhospital exposure reported, not only in patients but also in relatives and workers.4,7
Timely diagnosis and treatment of TB infection could avoid challenging situations due to interactions of TB drugs, as well as treating LTBI with shorter and simpler schemes than in pulmonary TB. Hepatotoxicity of isoniazid, rifampin and pyrazinamide is well known and these drugs can interact with many others, delaying chemotherapy. Two patients did not receive prophylactic therapy with isoniazid due to elevation of liver enzymes, caused by underlying oncological condition, but symptoms were carefully monitored until second evaluation 8-weeks after last exposure was done, which concluded no TB infection.
Diagnosis is not only challenging due to test discrepancies and potential false negatives results, but also due to a possible pulmonary involvement of the underlying disease or other respiratory infections that can mimic TB. Therefore, we should bear in mind these possibilities as occurred in two of our patients; similar cases have been reported.3,6,8,9
Moreover, TB should be ruled out before starting chemotherapy due to the risk of progression of a latent TB infection when immunosuppression is started.3,8,10 Stefan et al. reported 17.6% of diagnosis of TB in a cohort of 34 children screened before chemotherapy in South Africa, a country with a high TB incidence.6,11 On our cohort, only 14 children (54%) had TST prior to starting chemotherapy. Some of them were referred from other hospitals or received urgent chemotherapy treatment, but in other cases there were no reasons for this lack of testing. Even in a low TB incidence country like Spain TB is convenient to be ruled out before immunosuppressive therapy.
It is advisable that as soon it is known that a patient requires immunosuppressive therapy, TB screening is performed. Whether it is not possible to wait for screening results, at least it would be convenient to perform TST and/or IGRA before starting immunosuppression. Despite the convenience of TB screening for all these patients, it is especially important for those coming from medium-high burden TB countries and if there has been a potential contact to a TB case. Adaptation of local guidelines to screen TB before starting chemotherapy could benefit haemato-oncological patients preventing progression from latent to active TB.
Management of TB contacts in a paediatric haemato-oncology unit is challenging. Underlying diseases might mimic TB and diagnostic tests can show discrepancies and lower performance than in healthy patients.
The approach to oncologic children exposed to TB involved a multidisciplinary team and a considerable use of resources in a short period of time.
EthicsResearch ethics committee from Hospital 12 de Octubre approved this work, in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments
Authors’ contributionsAll authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by CDG, CE, MBF, ARSS, DBG, CL, PLR, PGG and CM. The first draft of the manuscript was written by Carlos Daniel Grasa Lozano and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
FundingCDG is funded by the Spanish Ministry of Science and Innovation—Instituto de Salud Carlos III and Fondos FEDER (Contrato Río Hortega CM19/00015).
Conflicts of interestNone of the authors have conflict of interest, financial or otherwise related to this manuscript.
We would like to acknowledge all the workers from paediatric haemato-oncology, paediatric infectious diseases, paediatric radiology and microbiology departments.