A 21-year-old Mexican male was admitted to the hospital with intermittent fever, night sweats and weight loss of six weeks duration. He denied dyspnea, cough, headache, or gastrointestinal symptoms.
On examination, the patient was febrile (38.5°C), hemodynamically stable and had intact sensorium. Small, non-tender, soft cervical and inguinal lymph nodes were palpable. Abdominal examination showed asymmetrical distension of the abdomen, with hepatosplenomegaly; other system examinations were normal.
Initial work-up done included a chest X-ray showing nodular hiliar and mediastinal infiltrates. Complete hemogram showed hemoglobin 10.5g/dl, total leukocyte count 4100/mm3 with 14% monocytes and normal platelets. Other laboratory examination disclosed LDH at 380U/l. Human immunodeficiency virus (HIV) antibody-based test was non-reactive, and the tuberculin skin test was negative. Interferon-Gamma Release Assays were not performed.
In light of these findings, excisional biopsy of the lymph nodes was pursued.
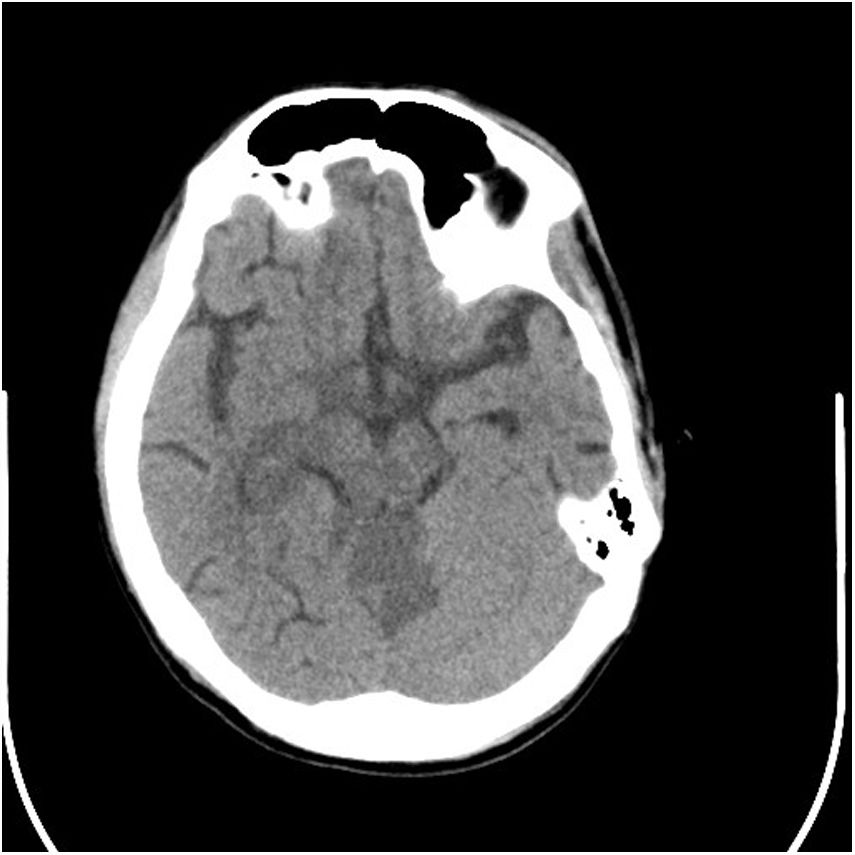
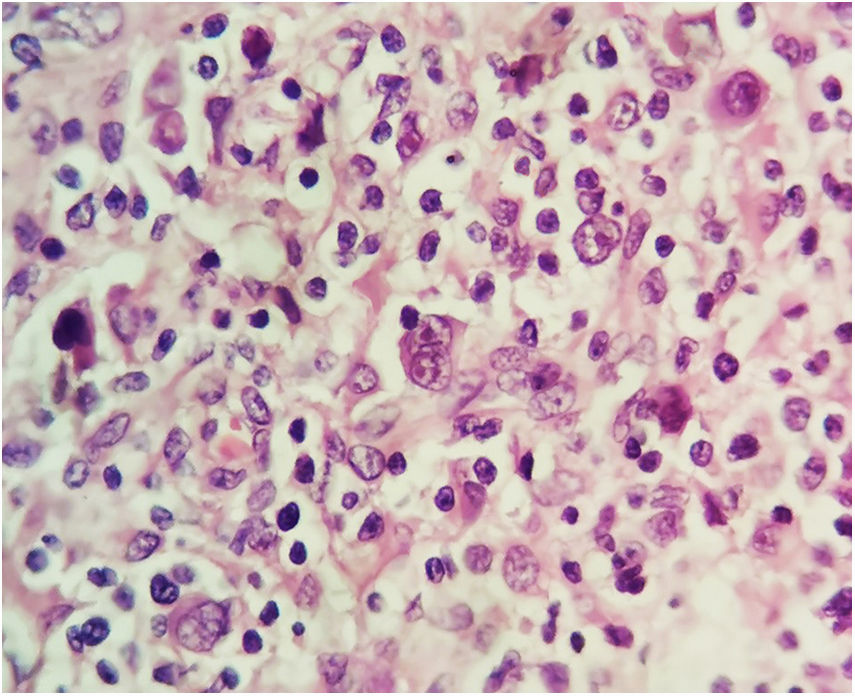
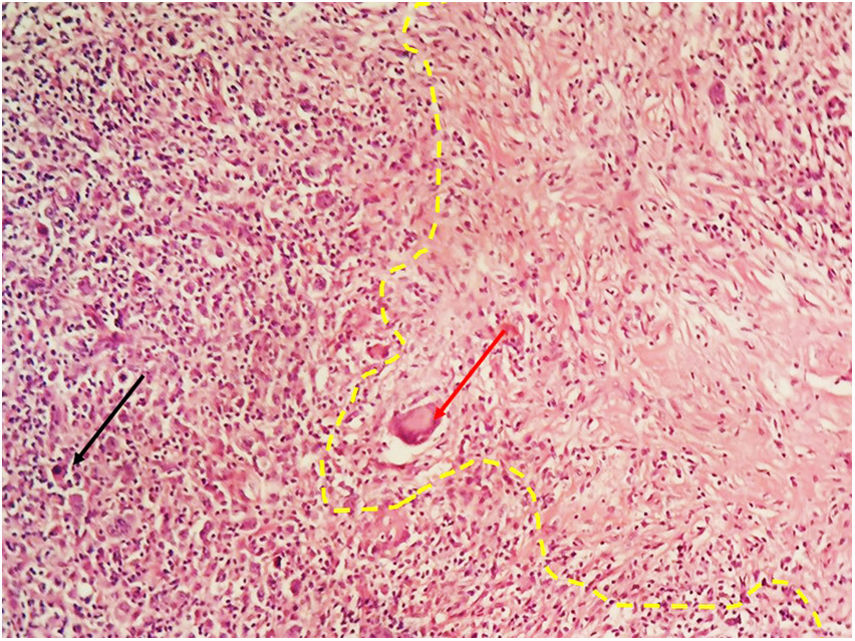
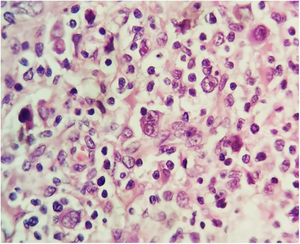
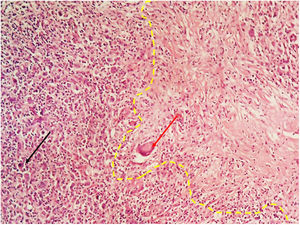
EvolutionWhile undergoing work-up, the patient developed severe headache and tonic–clonic seizures of more than five minutes duration. A diagnosis of convulsive status epilepticus was made clinically and emergent neuroimaging was pursued. A brain CT depicted multiple infarcts located in the brainstem, thalamus and cerebellum (Fig. 1); CSF analysis showed 27cells/mm3 (38% lymphocytes), protein 164mg/dl, glucose 18mg/dl. Antituberculous drugs were administered empirically along with intravenous corticosteroids. GeneXpert MTB/RIF in cerebrospinal fluid was positive for Mycobacterium tuberculosis. A few days later, conventional microscopy examination of the lymph node biopsy showed Hodgkin lymphoma (HL), mixed cellularity type. Numerous binucleate and multinucleate Hodgkin Reed–Sternberg cells were seen (Fig. 2). Immunohistochemistry of tumor cells expressed CD 3, CD 15, CD 20 and CD 30. Surprisingly, there were focal areas showing caseous necrosis (Fig. 3), although stains for acid-fast bacilli were negative.
The patient continued to deteriorate and died on day 12 after admission.
CommentsLymphoma and tuberculosis share common presentations that may lead to misdiagnosis. Both conditions, however, rarely coexist at the same time in the same patient.
M. tuberculosis has the potential to modulate macrophage polarization, being capable of inducing direct DNA damage and apoptosis inhibition, which increase mutagenesis of progenitor cells.1,2
Immune suppression is a well-known condition in HL, where cellular immune deficiency may result in secondary infection. The presence of certain pathogens can also precede HL and some can contribute to HL development. Karakas et al.3 reported tuberculosis associated with HL in 14 of 70 children. Of these 14 patients, the diagnosis preceded that of HL in 3, in 2 there was a concomitant diagnosis, and 7 developed tuberculosis during HL treatment.
The presence of HL and tuberculosis in the same patient has been reported in the literature.4 Symptoms such as fever, weight loss, night sweats, hepatosplenomegaly and an elevated LDH can be present in both entities. Generalized lymph node enlargement is also common, leading to an incomplete—or erroneous—classification of Hodgkin disease. Besides, caseating or necrotizing granulomatous lesions typical for tuberculosis can also be found in HL.
Tuberculosis accompanying malignant lymphomas is often characterized by an atypical clinical course, with unusual extrapulmonary localizations. Confirmatory diagnosis of tuberculosis in such cases is difficult given the invasiveness entailed to access involved organs. Mantoux test is often negative by virtue of the impaired cellular response characteristic of HL patients. GeneXpert MTB/RIF on cerebrospinal fluid has a sensitivity and specificity of 82% and 99%, respectively,5 and it was the procedure which gave us the diagnosis of tuberculous meningitis. In addition, in our case, tuberculosis bacilli were absent in the biopsied lymph nodes.
Tuberculous meningitis is sub-acute disease and its symptoms are usually present for several days prior to diagnosis. After a period of non-specific signs, such as fever, headache, or personality changes which can last several weeks, patients can develop more severe headache, altered mental status, seizures, cranial nerve deficit and, in about 25% of patients, stroke.6,7 Inflammatory exudates near the area of circle of Willis are considered to be the main culprits for ischemia. Vasculitis, thrombosis or vasospasm in this area typically leads to multifocal infarctions in the basal ganglia, internal capsule and thalamus (the so-called “TB zone”). Less than a fifth of patients evaluated in the published literature had involvement of brainstem and cerebellum.8
Clinicians should consider co-existing tuberculosis in patients with lymphoma; an association that must be considered to prevent serious clinical consequences related to both disorders, especially in countries where tuberculosis is endemic.
FundingNone.
Authors’ contributionCarlos A. Andrade-Castellanos: conceived and wrote the manuscript.
Beatriz A. Paz-Velarde: participated in the design and coordination.
Elsa E. Carreón-Bautista: collected the data.
Luis I. Pozos-Ochoa: performed the histopathology.