Syphilis, an infectious disease caused by Treponema pallidum, has been described as the “great imitator” in medicine, especially in its secondary stage.1 Far from being a topic restricted to the pre-antimicrobial era, this disease is now a public health problem, with 7.1 million new cases per year in adults worldwide.2 This means it has to be considered as part of the differential diagnosis for numerous clinical manifestations, many of which are shared with systemic rheumatological diseases such as lupus and Still’s disease.
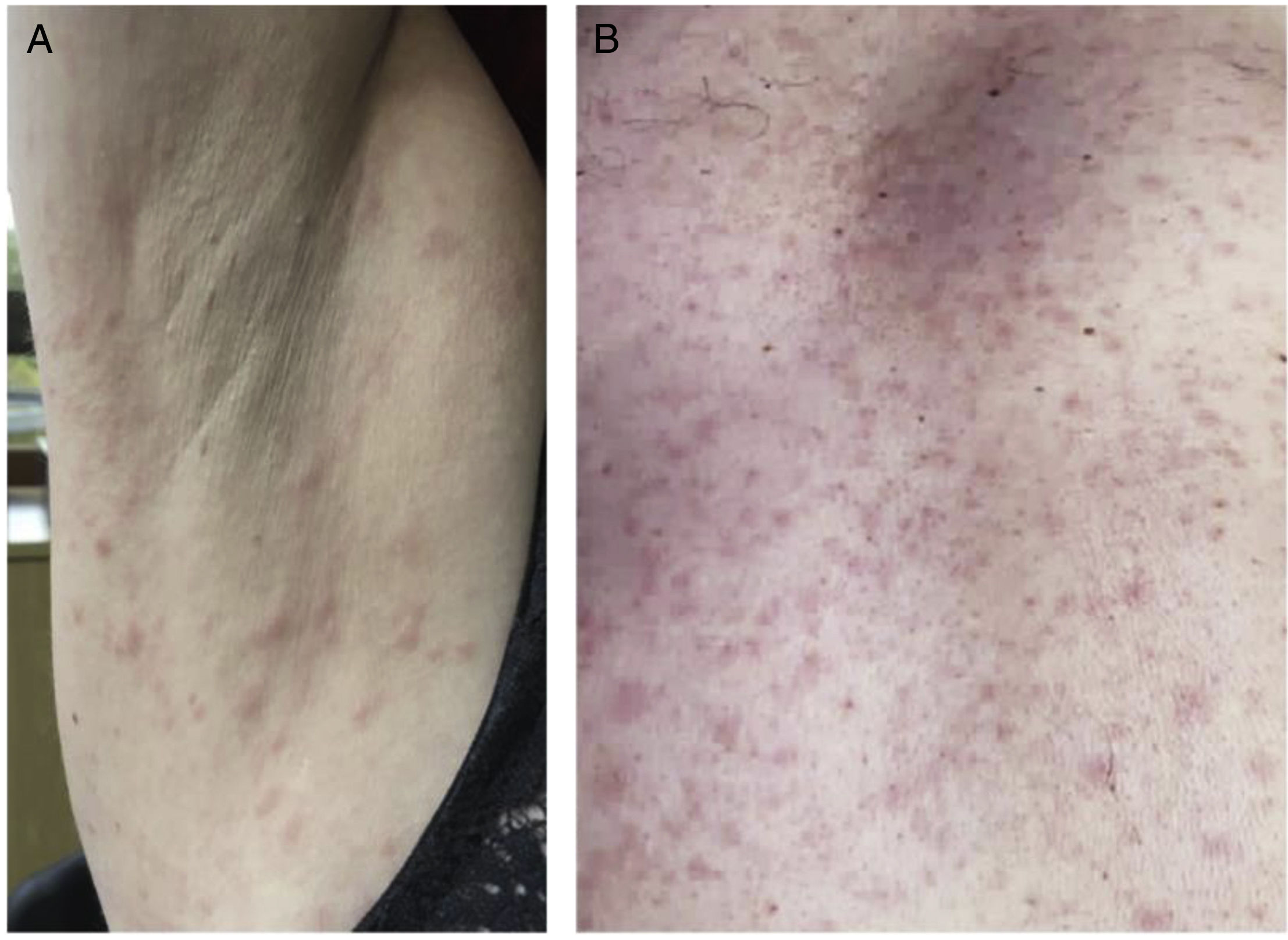
We present the case of a 42-year-old woman, with a sister with rheumatoid arthritis, who consulted for two months of polyarthralgia of small and large joints, associated with odynophagia, episodes of unquantified febrile sensation and maculopapular rash on the chest, abdomen and upper limbs, without palmoplantar involvement, pain or pruritus. Physical examination revealed only the described rash (Fig. 1A). Full blood count showed white blood cells of 6900/mm3, lymphocyte count of 1104/mm3 and an erythrocyte sedimentation rate of 63 mm/h. The rest of the general examinations were normal. Anti-nucleocytoplasmic antibodies (ANA) were positive (1/80 with homogeneous pattern), with negative anti-ENA, anti-DNA, rheumatoid factor and anti-neutrophil cytoplasm, as well as normal complements C3 and C4.
Despite denying risk factors, a VDRL (Venereal disease research laboratory) test was requested and was positive (1/64), as was the MHA-TP (microhaemagglutination assay for T. pallidum antibodies). HIV, HBV and HCV were negative. The patient was given benzathine penicillin (2.4 million IU) as a single dose, with excellent clinical response.
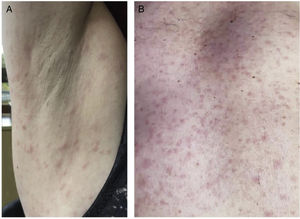
Another case was that of a 63-year-old male, with a sister with lupus nephropathy, who consulted with a two-month history of papular rash on his trunk and upper limbs, with involvement of the palms, associated with episodes of unquantified febrile sensation. He also reported polyarthralgia of small and large joints, mild oedema of the lower limbs and odynophagia. Physical examination revealed rash (Fig. 1B), mild soft oedema on both legs, painless cervical lymphadenopathy and two mouth ulcers, one on the hard palate and the other on the right lateral border of the tongue. Full blood count showed leucocyte count 6200/mm3, lymphocyte count 1099/mm3 and erythrocyte sedimentation rate 37 mm/h. The rest of the general examinations were normal. Positive ANA test with titre 1:640 with speckled pattern, with negative anti-ENA, anti-dsDNA, rheumatoid factor and anti-neutrophil cytoplasm, as well as normal complements C3 and C4.
Despite denying risky sexual behaviour, a VDRL test was requested and was positive (1/64), as was MHA-TP. HIV, HBV and HCV were negative. The patient was given benzathine penicillin (2.4 million IU) as a single dose, with excellent clinical response.
One to two months after the primary syphilitic lesion, which may go unnoticed, secondary manifestations arise due to haematogenous spread of T. pallidum. These can include symptoms such as fever, rash, odynophagia, lymphadenopathy, polyarthralgia or arthritis, mucosal lesions, alopecia, hepatitis and renal involvement.3 The rash, present in more than 80% of patients, is characteristically non-pruritic and involves the whole body, including palms and soles, which is considered key for clinical suspicion. It is usually maculopapular, symmetrical and sometimes even scaling, similar to psoriatic plaques.4 The diagnosis of secondary syphilis is confirmed by a positive VDRL and treponemal tests, such as the MHA-TP. Regarding treatment, there is consensus on the single-dose schedule with benzathine penicillin 2,400,000 IU.5
The cases described have a number of similarities. They both consulted rheumatology in the first instance and had a family history of autoimmune diseases. The symptoms were very similar, as was having a lymphocyte count at the lower limit, an aspect not consistent with the literature, which generally describes lymphocytosis, except when it occurs in patients with HIV, in whom lymphopenia predominates.6 Both patients had a positive ANA, which can occur in infectious diseases, especially tuberculosis and syphilis.7 The fact that 24% of lupus patients can have false-positive VDRL can make the differential diagnosis even more difficult.8
In conclusion, both conditions had clinical features of systemic autoimmune diseases, such as lupus and Still's disease, especially polyarthralgia and rash associated with fever and mouth ulcers. Secondary syphilis should therefore always be considered in the differential diagnosis of diseases that appear to be of rheumatic aetiology.
FundingNone.
Conflicts of interestThe authors have no conflicts of interest to declare.