Syncephalastrum spp. is a mucoral that rarely produces pathology. Fungal balls caused by this genus are infrequent. It requires early diagnosis and treatment to avoid associated morbidity and mortality.
MethodsWe describe two clinical cases of sinus fungus balls caused by Syncephalastrum spp. and review the literature.
ResultsTwo patients were treated for sinus fungus balls. When their samples were analysed, the aetiology was determined to be Syncephalastrum spp. A case of pulmonary fungus ball due to Syncephalastrum spp. is described in the literature. All cases, including these described in the present study, had a good evolution after treatment.
ConclusionsSyncephalastrum spp. is a filamentous fungus that should be considered as an aetiology of sinus fungus ball.
Syncephalastrum spp. es un mucoral que excepcionalmente produce patología. Las bolas fúngicas causadas por este género de hongos son infrecuentes. Requiere un diagnóstico y tratamiento precoces para evitar morbimortalidad asociada.
MétodosSe describen dos casos clínicos de bola fúngica sinusal por Syncephalastrum spp. y se realiza revisión bibliográfica.
ResultadosDos pacientes fueron tratadas de sendos casos de bola fúngica sinusal. Al ser analizadas sus muestras se determinó que su etiología era Syncephalastrum spp. En la literatura se describe un caso de bola fúngica pulmonar por Syncephalastrum spp. Todos los casos, incluyendo los descritos en el presente estudio, tuvieron una buena evolución tras tratamiento.
ConclusionesSyncephalastrum spp. es un hongo filamentoso que debe ser considerado como etiología de bola fúngica sinusal.
Syncephalastrum spp. is a genus of fungi of the Mucorales order frequently found in organic substrates, excrement, food and plants.1,2 Few clinical cases have been described for this genus in infections of varying severity and location, including rhino-orbital, rhino-orbitocerebral, nail, lung, abdominal, skin and soft tissues.3–6
The fungus ball causes a type of non-invasive fungal rhinosinusitis formed by a dense collection of hyphae which does not penetrate the tissue of the body cavity in which it resides, producing little inflammatory reaction.7
The outcome of these conditions is benign after endoscopic sinus surgery (ESS). They do not require antifungal treatment and there are few recurrences. In immunocompromised patients they can end up being invasive and fatal.7–9
This article presents two cases of fungus ball caused by Syncephalastrum spp. and includes a review of the literature.
MethodsWe report two cases of fungus ball caused by Syncephalastrum spp. We conducted a literature search in Embase, PubMed and Scopus, using the terms "Syncephalastrum sp.", "Syncephalastrum spp.", "Syncephalastrum monosporum" and "Syncephalastrum fungus ball". We reviewed age, gender, country, comorbidities or risk factors, pathology, treatment and outcome of the cases found.
ResultsCase report 1The subject is a 79-year-old woman, resident in Valladolid, with a history of right peripheral facial paralysis of unknown aetiology, type 2 diabetes mellitus and hypertension. In March 2022, she went to the Neurology Department due to post-paralysis spasms, which had increased in intensity over the previous three years, and the presence of headache in the last month.
A chance finding on the computed tomography (CT) scan of her brain was an occupation of the right maxillary sinus with a hyperdense, serpiginous structure inside and periosteal thickening, compatible with the presence of a fungus ball.
The patient reported no symptoms compatible with a fungus ball, but was referred to Ear, Nose and Throat (ENT). In the right nasal fossa, abundant purulent mucus was seen through the drainage ostium of the right maxillary sinus and a CT scan of the paranasal sinuses was requested with identical results as the previous CT scan. A median meatotomy was performed via ESS, which proceeded to flush out the sinus until all the fungal material was removed. Tissue samples were collected from the maxillary sinus and of the contents for microbiology and pathology study.
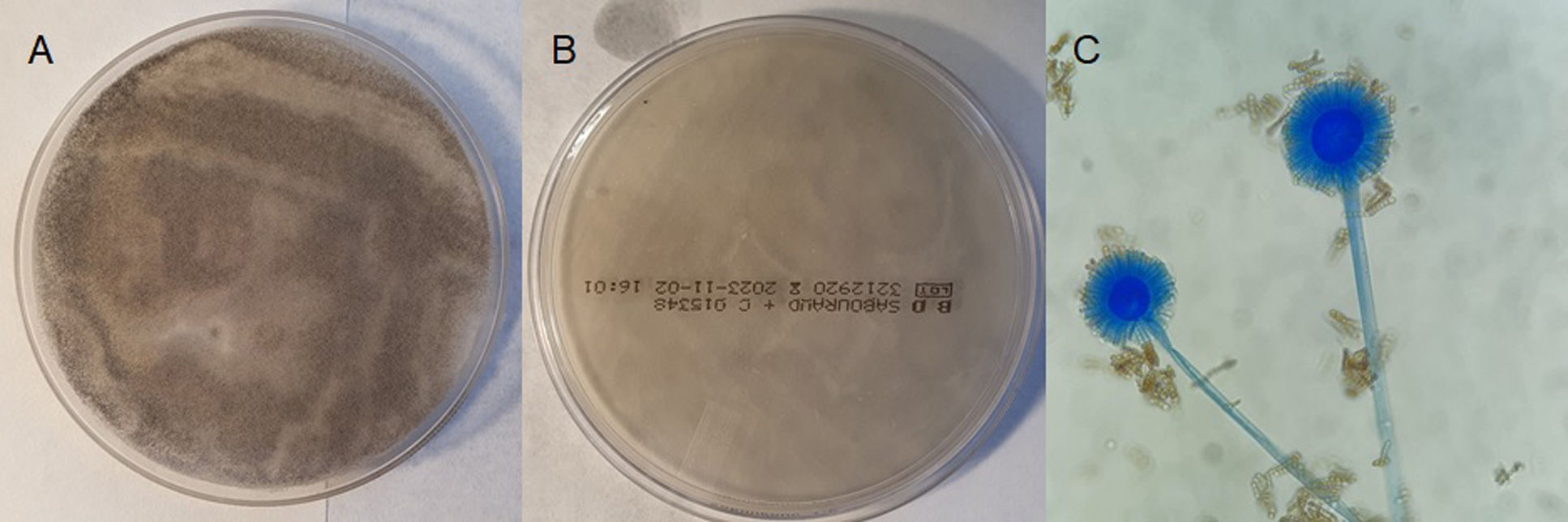
The Microbiology department conducted bacteriology and mycology studies. After 24 h on Sabouraud agar medium with chloramphenicol (Becton Dickinson, Franklin Lakes, United States) at 37€°C, three white colony-forming units grew on both the front and back, with a cotton-like appearance (Fig. 1). After 48 h they turned grey, fainter at the back. The fungus was identified by MALDI-TOF mass spectrometry (Bruker Daltonics MALDI Biotyper, Billerica, United States) as Syncephalastrum monosporum (S. monosporum), with a score of 2.21. Microscopic examination with lactophenol blue revealed non-septate, hyaline hyphae and sporangiophores with a terminal vesicle surrounded by thin-walled cylindrical merosporangia, narrower at the base than at the end. Each merosporangium had seven merospores or less and very few rhizoids were found. The phenotypic characteristics did not allow the species to be differentiated from Syncephalastrum.3,6
The strain was sent to Spain's National Microbiology Centre, where it was only possible to sequence part of the internal transcribed spacer (ITS) region of the ribosomal DNA. The sequence coincided firstly with Syncephalastrum racemosum and secondly with S. monosporum. Sequencing of the D1/D2 region of the 28S rRNA gene was unable to distinguish between the two species, as they have the same sequence.
Histopathology of the tissues showed accumulations of hyphae and spores, as well as polymorphic inflammatory infiltration with plasma cells, lymphocytes and polymorphonuclear leucocytes.
Following the intervention, the patient now has a patent maxillary sinus and has had no recurrences.
Case report 2The subject is a 54-year-old woman, resident in Valladolid, a smoker with no comorbidities, referred from Primary Care to the ENT outpatient clinic in September 2023 for assessment of long-standing impaired nasal breathing. Having undergone septoplasty on two occasions, her symptoms had worsened after suffering a nasal trauma.
When examined in the clinic, left septal deviation and purulent mucus were seen in the middle meatus of her right nasal fossa. Preoperative sinus CT showed septal deviation, occupation of the right sphenoid sinus with calcifications inside, as well as sclerosis of the bone margins. Occupation of the left frontal recess, bilateral ethmoidal cells and both maxillary sinuses was also identified. In the light of these findings, it was decided to perform endoscopic sinus surgery (ESS) in the same surgical intervention as septoplasty.
The patient underwent surgery in October 2023, with findings of a probable right sphenoidal mycetoma, as well as thickened/polypoid mucosa in right and left anteroposterior ethmoid sinuses and mucus/pus in posterior ethmoid and left sphenoid sinuses. Samples of the right sphenoid fungus ball were sent for microbiological culture and of the ethmoid, right maxillary and right sphenoid sinuses for pathology study.
In the microbiological culture of the sphenoid sinus, a fungus grew at 24 h with the same macro and microscopic characteristics as clinical case 1, being compatible with the presence of Syncephalastrum spp., which was identified by MALDI-TOF as S. monosporum, with a score of 2.17. This isolate was not sent to the National Microbiology Centre given the benign nature of the disease and the non-worthwhile nature of sequencing observed in case 1.
The histopathology examination of the respiratory mucosa of the left ethmoid sinus revealed changes due to chronic inflammation and non-invasive fungal forms, while in the sample obtained from the right sphenoid sinus, only fungal forms were evident, with no viable tissue found to assess for invasion. The rest of the samples did not contain fungal forms.
The patient is presently asymptomatic.
Literature reviewThe literature only describes one case of fungus ball due to Syncephalastrum spp., reported in 1979, which was occupying a cavity in the upper lobe of the left lung.10 The patient was a 61-year-old man from the United States with no comorbidities who, despite having no signs of invasion, underwent a left upper lobectomy after developing massive haemoptysis, with subsequent cure.
DiscussionThis study presents the first two cases to be reported of sinus fungus ball caused by Syncephalastrum spp. This is a rare condition which, when symptomatic, is similar to other types of chronic rhinosinusitis, with Aspergillus spp. being the aetiological agent in more than 90% of cases.7 It affects immunocompetent people, is more prevalent in middle-aged women and is associated with dental surgery.7
In the cases described here, one of the patients was an older adult with no history of dental surgery. However, the other patient had suffered nasal trauma. As trauma is one of the most common risk factors for suffering a rhino-orbital-cerebral infection by Syncephalastrum spp., it may have played a role in the formation of the fungus ball.6,11 Fungus balls are found mainly in one sinus, the maxilla being the most common.7–9 However, in case 2 they were found in the sphenoid and ethmoid sinuses.
The benign nature of this condition, in our case, was beneficial as, among the pathogenic Mucorales, those of the genus Syncephalastrum are considered the least pathogenic.5,12 As is usual in these conditions, only ESS was required, and it was not necessary to administer antifungals.7,8 The fact that so few cases of Syncephalastrum spp. fungus ball are detected is perhaps due to the difficulty in determining their aetiology through cultures; in one previous study only 32.1% of cultures performed on sinus fungus balls were positive.13 Nor can we rule out publication bias. For diagnostic purposes, CT and histopathology are more worthwhile,7,14 even if the causative species is not identified.
Although the sequencing of the ITS region shows inconsistent results, the literature describes the difficulties with ITS in the genus Syncephalastrum.6,15 In the literature there is a lack of consensus on the morphological description of S. monosporum.3,6 This, combined with the inconclusive results of the sequencing, means that it has only been possible to identify the isolates at the genus level. Despite the good score obtained in the MALDI-TOF, it could be another different species of Syncephalastrum which is phylogenetically close to it.3,6
In conclusion, Syncephalastrum spp. is a filamentous fungus to take into account as the aetiology of sinus fungus balls.
FundingNone.
Conflict of interestNone.