To analyze the efficacy of Baby-Led Weaning (BLW), the risk of choking, iron and zinc deficiency, growth faltering related to BLW, and knowledge about BLW in mothers and health professionals.
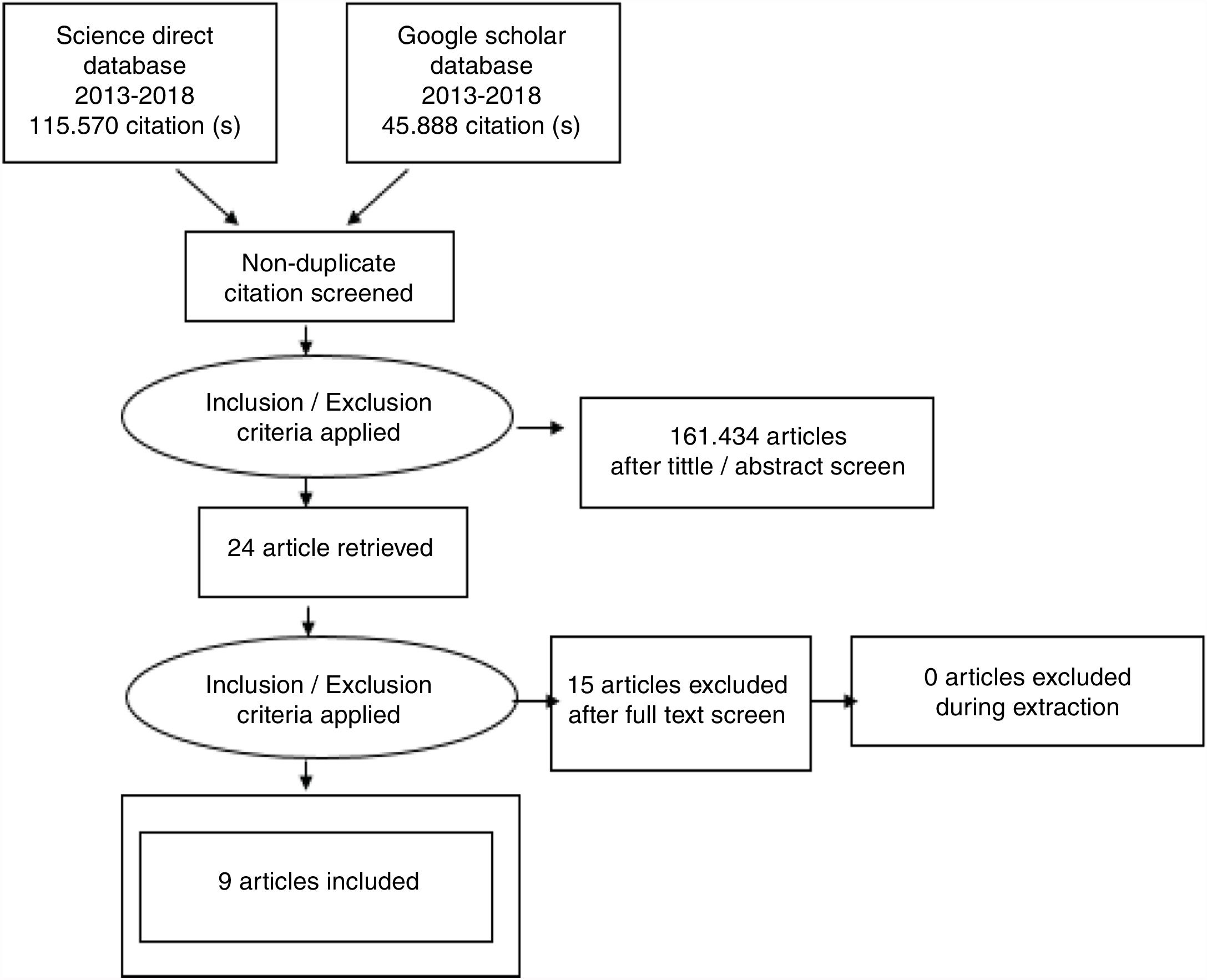
MethodThe search strategy involved the Science Direct and Google Scholar databases in 2013–2018. Nine articles related to research on BLW were analyzed.
ResultsThe evidence in these articles shows that BLW is good for self-regulation in the infant; the risk of choking, iron and zinc deficiency, and growth faltering is low in BLW with the Baby-Led Introduction to SolidS (BLISS) program, and mothers prefer to listen to another mother who practices BLW rather than health professionals.
ConclusionBLW is useful for making infants independent using a self-feeding process. The long-term longitudinal study is needed to explore more about BLW according to its nutrition adequacy, intake, eating patterns, food preference, safety, and growth trend.
When infants reach six months of age, it is important to give them complementary foods because breast milk can no longer support the nutrition and energy that infants need.1,2 Introducing complementary foods can solve this changing of nutritional needs that escalates as the child develops in age.3 Traditionally, parents begin by giving pureed foods to their children, then slowly changing the texture to mashed and chopped foods until they reach 12 months old. Then, children will adapt to the same food as other family members.4
Six-month-old infants are developing the motoric skills that help them self-feed instead of being spoon-fed by adults. Self-feeding can foster better self-regulation in infants’ eating habits.1,5 Giving infants complementary foods is essential in this period, as there is a progressive reduction of breast milk or milk formula. Food introducing leads infants to train their dietary pattern to that of adult's within the second year of life.2
Besides the Traditional Spoon-Feeding (TSF) approach, there is another approach of giving complimentary food to infants. This approach is Baby-Led Weaning (BLW).6 BLW, or Auto Weaning, has been growing more popular with parents, especially in the UK, New Zealand, and some countries in Europe, since Gill Rapley introduced BLW in 2001.2,7 In BLW, children are encouraged to feed themselves. As parents tend to give family meals to children, BLW children have more diverse food.6 This method also encourages children to eat finger foods.3 BLW puts trust in infants to know what they need, when and how fast to eat, and how much food they want in the eating process. The BLW approach also facilitates infants’ knowledge of real foods in terms of the appearance, texture and flavor of the food. For example, pureed potatoes which is given to an infant at their beginning eating period does not have the real shape and texture of potato. In addition, the flavor may also alter due to added ingredients.7
Since BLW enthusiasm started to increase in 2015, health professionals began to demonstrate their concerns about the advantages and disadvantages of BLW.4 Easy access to information on giving complementary foods made parents start to debate between BLW and TSF methods. The aim of this review is to analyze the efficacy of BLW, the risk of choking, iron and zinc deficiency, and growth faltering related to BLW, and the knowledge of BLW in mothers and health professionals.
MethodSearch strategyTo answer the key questions, research articles dated between 2013 until August 2018 were found in the Science Direct and Google Scholar database. Search terms included baby-led weaning and feeding in the infant. The inclusion criteria were randomized controlled trials, and observational studies that compare the outcomes of nutritional status, choking risk, and deficiency in iron and zinc in BLW infants. After the inclusion/exclusion process (Fig. 1), we included nine articles consisting of five randomized controlled trials and four observed cross-sectional articles.
ResultsNine quantitative articles from Canada, New Zealand, Turkey, and United Kingdom had been described (Table 1) analyzed. The samples ranged between 65 until 1151 respondents, consisted of mothers, infants, or mother-infant dyad. Several themes are explained in the following section: 1) the way mothers apply BLW; 2) BLW improves good nutritional status in infants; 3) BLW has a low choking risk; and 4) BLW related to lower intake in iron and zinc.
The quantitative article.
| Author/s | Type of study | Type of data collection | Number of subjects | Comparison | Intervention | Outcomes measures |
|---|---|---|---|---|---|---|
| Daniels et al. | Two arms randomized controlled trial. | Demographic data, anthropometric (weight) measures, and questionnaires. | 200 families. | BLISS vs. Traditional Spoon-Feeding. | Control group: received standard Well Child.Intervention/BLISS group: received standard Well Child and additional parent contact to support and educate on BLISS. | BMI, energy self-regulation, iron, and zinc intake and status, diet quality, choking, growth faltering and parents’ acceptability.BLISS that applied in 200 families able to prevent iron deficiency, minimize choking risk and growth faltering. |
| D’andrea et al. | Observational (comparative cross-sectional). | Online questionnaire. | 65 mothers who were practicing BLW and 33 HCPs (18 registered dietitians, eight nurses, three lactation consultants, two physicians, one occupational therapist, and one physiotherapist). | Compare knowledge and perception about BLW in mothers who practicing BLW and HCPs. | – | Concern about BLW in mothers and HCPs and source of knowledge about BLW that mothers obtain from. Mothers in BLW described BLW according to the shape and consistency of foods. HCPs more concern about the possible disadvantages of BLW. Mothers were more likely to search information from social media. |
| Morison et al. | Observational (comparative cross-sectional) | Demographic questionnaire, feeding questionnaire, and Weighed Diet Record (WDR). | 51 mothers and 51 infants. | BLW vs. TSF. | – | Food and nutrient intake, self-feed vs. parent-fed infants, and infant involvement in family meals.BLW infants consume more energy and saturated fat than TSF. In contrast, BLW less consume of iron, zinc, and vitamin B12 than TSF. |
| Brown, A. | Observational (comparative cross-sectional). | Demographic background data and questionnaire. | 1.151 mothers. | Choking in BLW vs. TSF. | – | Choking frequency among infants with BLW and TSF approach.TSF infants were more often to have choking incidents due to finger and lumpy foods than strict or loose BLW. |
| Daniels et al. | Randomized controlled trial. | Maternal demographic data and biochemical data (venous blood sample). | 206 mothers. | Iron status in infants with BLISS and control group (TSF). | The control group (TSF group) get standard midwifery and Well Childcare. The intervention group (BLISS) get standard midwifery, Well Childcare, and additional visit for providing education and support on BLISS approach. | Dietary intake and iron status. Difference iron intake between BLISS and TSF is not significant. |
| Daniels et al. | 2 arms randomized controlled trial. | Demographic data, zinc intake, and biochemical data. (plasma zinc concentration). | 206 parents from community-based participant | Zinc status in infants with BLISS and control group (TSF). | Control group received standard midwifery and Well Childcare.The intervention group (BLISS) get support and education before birth until nine months of age on following BLISS approach and eight study visits providing training and support regarding BLISS. | Dietary intake and zinc status.The zinc intake between BLISS and TSF group were not significantly different. |
| Erickson et al. | Randomized controlled trial. | Demographic data and 3-days Weighed Diet Records (3DDR). | 206 mothers. | Determine the impact of a modified BLW (BLISS). | Control group get standard Well Childcare.The intervention group (BLISS) get standard Well Childcare, lactation consultant support to 6 months, and educational sessions about BLISS. | Body mass index and analysis of food and nutrient intake.BLISS infants consumed more sodium and fat than TSF infants. On the other side, BLISS infants consumed less saturated fat than TSF infants. |
| Dogan, et al. | Randomized Controlled Trial | Demographic data; adherence to the BLW approach; the number of different iron-containing foods, high-energy foods, and high choking risk; and food that responsible for gagging and choking. | 280 children. | Traditional Spoon Feeding vs. Baby-Led Weaning | Traditional spoon feeding (control group) received free well-child visit, recommendation to continue breastfeeding and giving complementary food according to WHO guidelines.Baby-Led Weaning group (intervention group) received free well-child visit, recommendation to continue breastfeeding and giving complementary food according to WHO guidelines, BLW training from the team (dietitian, pediatrician, lactation consultant, pediatric nurse), BLW recipe books, BLW food list. | Infant growth, hematologic parameter, and iron intakes.Infants with TSF have higher weight than BLW. There is no significant differences in iron intake and choking incident between these two groups. |
| Cameron, et al. | Cross-Sectional | The online survey (Starting complementary foods; BLW; Attitudes toward, and experiences of, feeding the infants; and demographic information) | 199 mothers. | Parent-led weaning vs. baby-led weaning. | – | Infants in Adherent BLW group consumed more family foods and less instant baby-food. Both of BLW groups (Adherent and Self Identified BLW) prefer to share family foods than the Parent-Led Weaning group. Infants in Adherent group are not offered for consuming iron-fortified cereal. |
An infant already has well-developed digestive organs and kidneys, which support infants in eating complementary foods at 6 months of age.1 Determining whether an infant is ready to eat food can be shown by indicators such as being able to open the mouth more often, putting hands inside the mouth, and starting to grab parents’ foods or cutlery while eating.3,8 Strict BLW does not allow children to be assisted (spoon-fed) by an adult during the eating process.9 BLW encourages infants to control how much food they want to eat—a process they have already learned while they were breastfeeding.4 One positive of BLW is that BLW children can taste and distinguish their foods one by one, while TSF children cannot distinguish different tastes because their foods are mixed.2
In the TSF approach, finger foods are seldom given to infants until they reach 8–9 months of age.1 The World Health Organization (WHO) suggests the complementary foods must be safe, given at the right time, and adequate.2 The WHO also suggests that when infants begin to get familiar with complimentary foods, they should be given in small, semi-solid portions that vary in consistency as the child develops.9
The BLW approach requires some essential elements for infants. Since they consume both milk and baby-led family food at mealtimes, BLW infants must keep receiving milk (breast milk or milk formula) according to their needs. Pureed food is not given to BLW infants because the texture makes it difficult to feed themselves, and feeding will be different if a parent gives foods like yogurt and pudding that need a spoon to eat them. The foods are also family meals, and infants will eat with other family members at mealtime.1,8
A study by Morison et al.4 compared the giving patterns for complementary foods between BLW and TSF. It was found that more children with BLW exclusively received breast milk longer than TSF children—for eight months, receiving their first foods three later. After receiving their first food, BLW infants did not receive any milk formula, in contrast with almost half of TSF infants who received breast milk mixed with milk formula.
The first food introduced to BLW infants was finger food, and infants in the BLW group tended to self-feed, in contrast with TSF infants who received pureed or mashed foods as their first foods and were assisted in spoon-feeding by their parents or another adult. While most of the BLW infants self-fed, one-third of the participants in the BLW group received pureed or mashed foods as first foods and were spoon-fed by their parents. This situation can be defined as partial BLW.4,8
In the Full BLW group, infants were more likely to eat family meals and sit with other family members during mealtime than the TSF group. Mothers in the BLW group liked to serve the same meals to infants and other family members, according to the ingredients and preparation style of those meals.4 Family foods are not always suitable for infants. It is possible that a family meal could contain high sugar and salt. Thus, family food that is also given to an infant must also be suitable for infants because it is essential to build proper health outcomes in adulthood.1
Cameron categorized the BLW group into two types: the Adherent BLW and Self-Identified BLW. An infant who self-fed at 6–7 months old was classified into the Adherent group. Infants in the Adherent BLW group preferred to eat family foods. Parents in this group were less likely to offer commercial baby foods to their infants. Both Adherent and Self-Identified BLW were more like to share their foods with family than the Parent-Led Weaning group. Parents in Self-Identified BLW consist of mothers who classified their infant's feeding way by themselves into BLW terms. On the other hand, Parents-Led Weaning is likely to have similar definition as Spoon-Feeding method which parents who has control on eating activities of their infants. If the infant was offered pureed food like pureed mince on toast, they were still classified to the BLW group because this was determined by the way of feeding not the kind of foods.10
BLW improves good nutritional status in infantsBLW children tend to have a lower Body Mass Index (BMI) than TSF children, which makes BLW children less at risk for obesity. They are lighter (86%) but still normal in weight status, with only 5% having an underweight status, while 8% are overweight. Mothers who are doing BLW are reported to be more relaxed during the feeding process. They feel less pressure when feeding their children and do not worry too much about the increase in their children's weight.3,11 There is no difference in fruits, vegetables, and meat consumption in the two groups (BLW and TSF). In the BLW group, infants receive their first iron-fortified cereals for 5.1 weeks longer than the TSF group.4
Infants sometimes cannot feed themselves due to sickness. Some parents also worry about iron intake in BLW infants. So, parents offer iron-fortified cereal to their infants to ensure an appropriate iron intake. This fact shows that BLW and TSF are dichotomous methods. The style of feeding in infants can be suited to the infant's needs at a particular time.10
BLW has a low choking riskChoking can easily happen in an infant who is still learning to eat. The infant is learning how to move, chew, and bite foods in the mouth for the first time. At six months of age, the infant may not have the skill to safely digest whole foods.1,2 Overall in the BLW and TSF groups, two-thirds of parents give foods that can trigger choking in their infants. In the BLW group, the foods that trigger choking are raw vegetables, raw apples, and dried fruits. D’andrea also states that apple chunks have enough of a hard texture to trigger a choking incident.9 Meanwhile, in the TSF group, foods that trigger choking are rusks, small pieces of meat, crackers, and corn kernels.4
Choking is a hazard; in the UK, one infant dies every month due to choking, but infants that reach six months of age already have the ability for chewing. They can chew and swallow their foods even if their teeth are not yet present. They also can use their tongue to move foods inside the mouth. This ability will develop more until approximately nine months of age. Infants who always receive fingers food do not need to change to pureed or mashed foods because they already know what to expect and how to manipulate foods in their mouths. However, if finger foods are rarely given to infants, they can cause a choking incident.12 Infants who follow the TSF approach can also have a high risk of choking because they tend to hold foods inside the mouth and think they do not need to use any power to chew. This can trigger the risk of choking. There is no significant difference in choking incidents between TSF and BLW infants. Choking is more dangerous if it occurs before 12 months of age.3,10,11
Infants start to have a gag reflex when they reach six months of age. The gag reflex is used to protect from swallowing too-large foods. Gagging is common in BLW infants as compared to adults because it is triggered by stimuli closer to the front of the mouth and farther away from airway. At six months, BLW infants learn to keep foods from their airways when those foods are too large.9 The ability to distinguish between gagging and choking is vital for parents. Choking is a complete blockage of the airway due to a thing like food. Infants who are choking will make little sound, as air cannot pass through their airway. The infant will be very distressed, grab their throat, or can turn to blue. This requires intervention from an adult to force the food from the airway and mouth. Otherwise, gagging is a normal reflex that can occur in the infant when they reach six months of age. Gagging is also normal in infants who are learning self-feeding. Gagging happens when foods move to the back of the mouth, and infants cough and splutter then bring the food back to the front of their mouth again. Unlike choking, gagging is usually noisy.12 This fact can mean that mothers with more prominent anxiety during the feeding process will prefer to choose the traditional weaning approach or TSF rather than BLW because they can control their infants’ foods by spoon-feeding.2
BLW related to lower intake in iron and zincIron is an essential micronutrient for children. Children need iron to develop their red blood cells, body immunity, cognitive development, and strengthen their oxygen levels, which is also a signal for hunger. During the neonatal period, 80% of the iron is accumulated and saved since the last third semester in the antenatal period. When the infant is six months of age, iron storage lessens.3 BLW infants tend to have a wide variety of nutrition intake. The intake of total fat, saturated fat, and the percentage of energy from fat and saturated fat in the Full BLW group is higher than in the TSF group. In contrast, the TSF group has a higher intake of iron, zinc, vitamin B12, vitamin C, dietary fiber, and calcium. In the consumption of energy, sugar, or sodium, there are no differences between these two groups.4,8
In infants with BLW, it is common to give fruits and vegetable as a first food. These kind of foods contain less iron. Iron-fortified infant cereals can be offered to infants for their sufficient iron intake, but foods like cereals are hard to give to BLW infants because they are liquid. However, the BLW infant can get iron from another food like red meat served in sliced shapes big enough for an infant to hold. Similar to iron, zinc is also rare in some foods that infants consume in the BLW approach. As we know, poor zinc status can effect growth, motor and cognitive development, and also the immune function in infants.1 One solution for the iron and zinc needed by BLW infants is applying the Baby-Led Introduction to SolidS (BLISS) approach. BLISS is a modified BLW approach that has its own guidelines. Besides providing the necessary iron and zinc, BLISS also can minimize the risk of choking incidents and growth faltering.1
DiscussionParent start introducing BLW to their infants when they reached 5–8 months of age. They choose BLW because it makes sense and feels natural. Most of the parents in the BLW group encouraged their infants to feed themselves when they started to eat for the first time.9 A fundamental aspect of BLW is sharing meals with the family. This act can make parents become role models for their infants while eating. This process teaches infants to learn which foods are safe, to use cutlery by themselves, and to use cups. BLW can also promote speech and language development.7,8 Information about BLW is available from online sources like Facebook. When defining BLW, parents identified two themes: food shapes (solid, whole, appropriate-sized, nonpureed foods) and control over an infant in the feeding process (how much they eat and when).8,9
The primary difference between BLW and TSF is the texture of the food. TSF starts with pureed food, but BLW starts with finger food, such as a slice of fruit, a slice of vegetable cooked until soft, a slice of meat, and a slice of cheese. These foods have a shape that can allow infants to hold them. Foods that require more chewing require a more complex process. Thus, the foods must break easily, easily mix with saliva, and easily transport to the back of the mouth for swallowing. The texture needs to give partly, to facilitate infants’ ability to chew and swallow. Considering the size of the infant's airway is still small, there is a concern for preventing choking incidents.3
BLW is connected with a longer duration of giving breast milk, a later start to introducing the infant's first food, and significant participation in a family meal.4,8 The Strict BLW group introduces solid food later than the Loose BLW and TSF.12 On the nutrition side, BLW infants consume more fat but less iron and zinc than the TSF group. Because BLW infants tend to eat fruits and vegetables that containing less iron,4 the infant's iron intake can come from complementary foods like iron-fortified cereals for infants, which are recommended to solve the iron deficiency problem. Infants with BLW may have a higher risk for iron deficiency because the texture of cereals makes them hard to chew and to feed to BLW infants.
Daniels et al.’s research about zinc status in BLISS is famous as a modified BLW. This study states that, before seven months, the predominant source of zinc for infants comes from breast milk and infant formula in the BLISS and TSF groups. BLISS recommends foods high in iron, so these kinds of foods can be effective in improving iron intake in BLW infants. It is different with unmodified BLW because unmodified BLW is less likely than BLISS to serve red meat, a food high in iron. When solid food starts to be introduced in the BLISS group, BLISS infants get more zinc from bread, cereals, dairy products, red meat, eggs, legumes, nuts, and seeds than the TSF group.11 Daniels’ study shows that BLISS is a solution for parents who want to choose a BLW approach for their infants but still can make zinc status of their infants well.13 Infants with BLISS consume less saturated fat than the control group (TSF infants). BLISS infants also have more energy than TSF infants due to their foods choices.6
Overall, BLISS has a positive impact on an infant. Infants with BLISS have a higher intake of iron, zinc, vitamin C, vitamin B12, and calcium than unmodified BLW infants. But, in terms of sodium, BLISS infants have a higher sodium intake than TSF infants. Sodium levels will higher because they eat family meals. Salty family foods will affect these infants if the parents do not prepare for this. Further, the increased sodium in BLISS infants may occur due to parents. Parents were encouraged to use toast as a vehicle to serve foods such as iron-fortified infant cereal, which infants can pick up by themselves, and gave their infants cheese as an energy-rich and palatable food. This eating style happened because parents want to minimize the risk of growth faltering in their infants. Toast and cheese are high in sodium.6 Because infants are more likely to follow family foods, which are adult foods, this can be an issue. If families serve unhealthy foods, infants are at risk to eat unhealthy food as well.4
Three groups (Full BLW, partial BLW, and TSF group) show the same possibility of choking in infants. The highest incidence of choking happens in Loose/Partial BLW, then in TSF, while less happened in Strict/Full BLW.12 Infants with BLW can be at risk for choking because they are still learning how to feed themselves in their early stages. This can encourage the parent to be more aware of the risk of choking that can occur.6
Specifics foods that can be manipulated can make choking less risky. For example, it is better to give a slice of melon than a chunk of melon that can slip out of hand and get stuck in the infant's throat.12 The traditional way of parents tipping and distracting infants with the airplane trick while eating actually has a negative impact and can trigger a choking incident. This negative impact happened because this feeding style overrides or bypasses the natural constraints such as the ability of gagging reflex that exist during the feeding process.7
Infants’ characteristics can determine the best feeding method for them. Infants who have feeding problems before or have experience in choking when drinking milk are less likely to be successful in BLW. Infants that have bad temperaments are also make using BLW challenging. So, understanding the infant's characteristics is important before the parent chooses a feeding method. Furthermore, mothers’ characteristics also play a role in the feeding process. Higher maternal anxiety can trigger a choking risk, for instance, when mothers accompany their infants at mealtime and cut foods into smaller pieces and encourage the infants’ intake of foods. In Loose BLW, the parent applies the BLW method for their infants but still wants to keep their infants safe by giving pureed and spoiling them in eating process. This can happen due to anxiety, even with parents who already know about the differences between choking and gagging.12
In introducing BLW, Health Care Professionals (HCPs) are often used as a source of information for mothers. HCPs support and play an essential role in encouraging parents to decide an infant's feeding method.9 On the other hand, more parents like to learn about BLW from sources other than HCPs because many HCPs were not supportive and sufficiently knowledgeable about the practice of BLW. HCPs must learn more about BLW, so they can help parents decide and support parents who follow the BLW method.9
To respond to fast-spreading BLW information, HCPs must be concerned about the social media effect in BLW promotion. HCPs must find proper tools for opening consultation about BLW with parents. So far, parents are more likely to know BLW from a social media platform. Thus, HCPs should consider doing consultations through social media platforms to motivate and educate parents.9 Furthermore, parents feel satisfied in applying BLW that have many advantages. Parents who succeed in BLW are likely to share their experience with other parents. However, HCPs are more concerned about the possible disadvantages of BLW.9
BLW is useful for making infants independent using a self-feeding process. They can taste foods better and have better self-regulation control while eating than TSF infants. The risk of choking is not significantly different between BLW infants and TSF infants because, at six months of age, they already have the skill for chewing and swallowing, and they have a gag reflex.
Parents should search more about BLW information in legal platforms. Meanwhile, HCPs must make proper tools to connect with parents in a simple platform, according to the parents’ interest. BLW can be applied properly if parents get information from the right source. The long-term longitudinal study is needed to determine more about BLW according to its nutrition adequacy, intake, eating patterns, food preference, safety, and growth trend.
Conflict of interestsThe authors declare no conflict of interest.
We acknowledge the Directorate of Research and Community Engagement Universitas Indonesia for their support for this publication through Hibah PITTA.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.