To analyse health-related quality of life in a sample of doctors and nurses from 2 intensive care units in the city of Buenos Aires, Argentina.
MethodsAn analytical, cross-sectional and quantitative study. The Spanish version of the SF-36 questionnaire was used, which comprises 8 dimensions grouped into 2 components (physical and mental) and evaluates the health status of respondents on a scale from 0 to 100; the higher the score, the better the perception of health status.
ResultsNinety-five professionals from 2 intensive care units participated, 58% from a private institution and the rest from a public institution. The majority were women (57%), doctors (37%) with an average age of 42 years and with a maximum undergraduate degree and degree (59%). Of the dimensions making up health-related quality of life, the vitality dimension was perceived poorest with an average of 53.3, and physical function was the best evaluated at 87.8. The physical component dimensions were better evaluated than those of the mental component. The variables sex (male), age (> 40 years), presence of chronic diseases, qualification (medical), hourly workload (> 40 h per week) and years of service (> 11 years), seem to have a negative influence on the perception of health-related quality of life.
ConclusionsStrategies need to be implemented to reduce the impact of work activity on the mental and physical health of health professionals. Strategies for health promotion and the prevention of known psychosocial and ergonomic risks are required, and workloads and duration of working hours need to be adjusted to preserve the integrity of health workers.
Analizar la calidad de vida relacionada con la salud en una muestra de médicos y enfermeras de 2 unidades de cuidados intensivos de la Ciudad Autónoma de Buenos Aires, Argentina.
MétodoEstudio analítico, transversal y cuantitativo. Se utilizó el cuestionario SF-36 en su versión en español, el cual está compuesto por 8 dimensiones agrupadas en 2 componentes (físico y mental). Evalúa el estado de salud de los encuestados en una escala que va de 0 a 100, donde una mayor puntuación indica una mejor percepción del estado de la salud.
ResultadosParticiparon 95 profesionales de 2 unidades de cuidados intensivos, siendo de una institución privada el 58% y de una institución pública el resto. La mayoría fueron mujeres (57%), médicos (37%), con una edad media de 42 años y con título máximo de pregrado y grado (59%). De las dimensiones que componen la calidad de vida relacionada con la salud, la de vitalidad fue la peor percibida, con una media de 53,3, y la función física fue la mejor evaluada, con 87,8. Las dimensiones que conforman el componente físico presentaron una mejor evaluación frente a las del componente mental. Las variables sexo (hombre), edad (> 40 años), presencia de enfermedades crónicas, titulación (médico), carga horaria de trabajo (> 40 h semanales) y antigüedad laboral (> 11 años) parecen influir negativamente sobre la percepción de la calidad de vida relacionada con la salud.
ConclusionesEs necesario implementar estrategias tendientes a reducir el impacto de la actividad laboral sobre la salud psíquica y física de los profesionales de la salud, estableciendo estrategias de promoción de la salud y prevención de los riesgos psicosociales y ergonómicos conocidos, y adecuando las cargas y la duración de las jornadas de trabajo para preservar la integridad del trabajador de la salud.
In recent years, the study of workers' health has been given prominence, and aspects of the work environment in closed areas have been described which may have an impact on the health/illness dynamics of professionals. However, the impact of work variables in intensive care units (ICU) on the mental and physical health of healthcare professionals has been little described.
With this study we aimed to make a diagnosis of the health-related quality of life of intensivists in order to design and implement interventions to improve the health of the worker.
Study implicationsThis study is a starting point to determine the effects of work on the health of doctors and nurses working in ICUs, with consideration that deterioration in the health of the professional impacts on the quality of care that they provide for the patients. This leads to increases in ICU morbimortality rates, costs derived from healthcare and from fulfilment of the mission of the profession itself. It is also possible to gain a better understanding of how work impacts the personal, social and family life of the professional.
The concept of health has evolved over time, from the magical-religious conception of primitive cultures,1 to the present day where it is considered as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.2
Within the framework of occupational health, the aim has been to create working environments that are safe for workers, in order to prevent work from damaging their health and to prevent deterioration of their health from influencing their professional performance.3 The impact on health can be measured using a variety of objective and subjective indicators, with health-related quality of life (HRQoL) being an integrative measure of both, generating an indicator of the worker's overall well-being.4
According to Naughton et al., the term HRQoL refers to the way in which the individual assesses the impact of their health status, healthcare received and promotion of their health on their ability to carry out activities which are important to them and which affect their general perceived well-being status.5 HRQoL comprises aspects such as social, physical and cognitive functioning, personal care and emotional well-being.6 In a simpler definition, Trujillo et al. suggest it is “an individual’s satisfaction with the physical, social and psychological aspects of his or her life, insofar as they affect or are affected by his or her health”.7
The incorporation of HRQoL represents one of the most important advances in health evaluation,8 and in recent years has been used as a way of measuring the impact of working conditions (length of working day, workload, polyemployment) on the worker’s health. In the case of health professionals, deterioration in physical and mental health limits their potential to provide quality healthcare, which prompts a weakening of care services and an increase in patient morbimortality.9,10 It also affects extra-occupational issues such as the relationship with a partner and with the family, leisure time and sleeping habits.11–14
With regard to the ICU working environment, dozens of factors have been reported that affect workers’ health and these include high physical workloads and long working days standing up; emotional stress factors derived from deaths, suffering and pain; conflicts with superiors; fear of making a mistake; anxiety in the face of uncertainty; lack of user knowledge of equipment, and even lack of staff for appropriately covering the service.15–19
In Argentina, there is a diversity of professionals working in the ICUs and this includes nurses (nursing technicians -undergraduates- and bachelors in Nursing -graduates-), doctors, biochemists, radiologist technicians, kinesiologists, physiotherapists and nutritionists. This varies and depends on the size and complexity of the unit. This study focused on the largest population groups: doctors and nurses.
Argentina currently has 39.6 doctors and 25.8 nurses (technicians and graduates) for every 10,000 inhabitants, with the latter figure rising to 42.4 if nursing assistants are included and a ratio of .56 nurse/doctor.20,21 However, although the quantity of doctors in Argentina is above the region mean, there is an unequal distribution in national territory. Regarding nursing staff, as mentioned, 48% of them are assistants and aides, with there being a distinct lack of professional nurses and this is all the more evident in professionals who are skilled in critically ill patient care. As a result, there is work overload in terms of professional/patient ratios and weekly hours, which impacts the mental and physical health of the worker.
Due to all of the above, this study was designed with its aim to analyse the HRQoL in a sample of doctors and nurses of 2 ICUs in the autonomous city of Buenos Aires, Argentina.
MethodDesignThis was an analytical, cross-sectional study with a quantitative approach.
Population and environmentData were obtained from a sample of 95 health professionals (doctors and nurses) of two ICUs, one in a public hospital and one in a private hospital in the autonomous city of Buenos Aires, Argentina, in 2019.
We included all doctors and nurses with a minimum of 6 months length of service and who voluntarily agreed to participate in the research study by signing their informed consent. Professionals who were on standby (temporary staff), nursing assistants and workers who were on sick leave and/or on holiday were excluded.
The initial sample was of 103 workers, 4 of whom were excluded because they had less than 6 months seniority, one because they were on sick leave, 2 because they were on holiday and one because they did not wish to participate in the study.
VariablesThe variables of interest for this study included participant sociodemographics and employment and the dimensions of the HRQoL.22 The latter will be explained in more detail below.
Sociodemographics: this included institution (public, private); age (in years); biological gender (man, woman); profession (nursing technician or graduate, doctor); maximum level of education (undergraduate-graduate and postgraduate); presence of chronic disease (yes, no) and which one.
Employment: length of employment (in years); length of employment in that service (in years); daily working schedule (hours of work/normal day, without including extra hours); number of days of work per week.
HRQoL: physical functioning; role-physical; bodily pain; general health; vitality; social function; mental health; role-emotional and transition of health status.
ToolThe SF-36 questionnaire was applied. This is a generic sale which provides a health status profile and is applicable to patients, the general healthy population and workers, and the psychometric properties of which have been assessed in over 400 articles23 and have been validated for the Argentinean population.24
This questionnaire comprises 36 items, grouped into 8 dimensions which make up the HRQoL scale: physical functioning, role-physical, bodily pain, general health, vitality, social function, role-emotional and mental health. It also includes one item of transition of health status, which asks about the change in health status compared with the previous year. It is self-administered and requires between 10 and 15 minutes to fully complete.
The items are responded to on a Likert scale with from 3 to 6 alternatives, depending on the item.
Interpretation of the SF-36 requires following these steps:
1. Homogenisation of responses, using re-coding of the 10 items that require it, guaranteeing that all of them go in the same direction, i.e. the higher the score, the better the perceived health status.
2. Calculation of the sum of the items, as the gross score of the scales.
3. Lineal transformation of the gross scores to obtain scores on a scale between 0 and 100.
The SF-36 scales in their lineal transformation are analysed in the form of indexes with a range from 0 to 100 and are ordered so that the higher the score, the better the health status. Scores above or below 50 indicate better or poorer health status, respectively.
The questionnaire dimensions were defined as follows:
Physical functioning: degree to which health limits physical activities such as self-care, walking, climbing stairs, bending, getting up or lifting heavy objects and moderate and intense efforts. This dimension contains 10 items.
Role -physical: degree to which physical health interferes with work and in other daily activities, including lower performance than desired, limitation in the type of activities performed or difficulty in carrying out activities. This dimension contains 4 items.
Bodily pain: the intensity of pain and its effect in regular work, both outside and inside the home. This dimension contains 2 items.
General health: personal assessment of health, which includes current health, future health outlook and resistance to falling ill. This dimension contains 5 items.
Vitality: feeling of energy and vitality, compared with feeling of tiredness and exhaustion. This dimension contains 4 items.
Social function: degree to which physical or emotional health problems interfere in normal social life. This dimension contains 2 items.
Role-emotional: degree to which emotional problems interfere in work and other daily activities, which includes reduction in time dedicated to these activities, lower performance than desired, and a reduction in care when working. This dimension contains 3 items.
Mental health: general mental health, which includes depression, anxiety, control over behaviour, emotional control, and positive effect in general. This dimension contains 5 items.
Transition of health status: assessment of current health compared with that of one year previously. This dimension contains one item.
Data collectionWith the approval of the institution, the survey was requested to be filled out at the beginning or end of the working day, explaining the study objectives and requesting the respondent to sign the informed consent form. The invitation to participate was made by the principal researcher in charge of the study. The questionnaire was handed out in paper format and was requested to be returned in a closed envelope to the researcher at the beginning of their following shift. 100% of the surveys submitted were collected.
Data analysisAfter collection, data were tabulated in a Microsoft Excel data matrix and analysed using Info Stat v/L statistical software. Normality tests (modified Shapiro-Wilk test) were performed to analyse the behaviour of the variables, finding an abnormal distribution of the variables (dimensions that make up the HRQoL). Therefore, non-parametric tests were applied: the Wilcoxon test for independent samples in variables with dichotomous categories and the Kruskal-Wallis test for variables with 3 or more categories.
Quantitative variables were expressed using the arithmetic mean and standard deviation, and in the case of those who presented with abnormal distribution, the median was used. In the case of variables such as weekly workload and length of service, data were grouped into categories, whilst the dimensions comprising HRQoL were analysed as both indexes (range 0 to 100) and as categories (≤ 50, ≥ 51).
For analysis the sample was divided into groups according to gender (man/woman); institution (public/private); level of training (graduate/postgraduate); profession/qualification (nursing technician/nursing graduate/doctor); weekly workload (< 40 hours/41-60 h/> 61 hours weekly) and length of service (< 10 years/11 to 20 years/> 21 years).
A significance level was fixed at p < .05 and the 95% confidence interval was calculated for variables composing the HRQoL.
Ethical considerationsThe study had the approval of the health research ethics committee, which approved the protocol, the informed consent form and the curriculum of the principal researcher.
Each participant was informed of the objectives and study method, and showed their approval through signing the informed consent form. No personal data were requested nor could any information from the completed questionnanire be linked to the respondent.
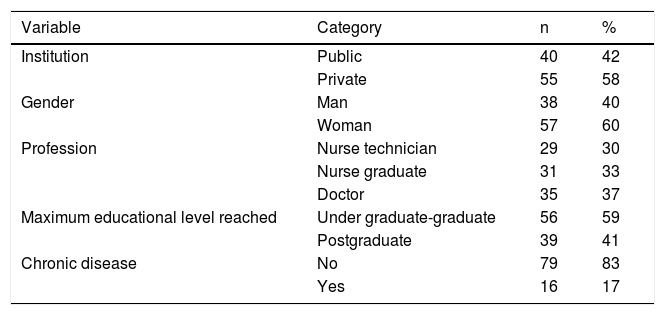
ResultsThe sample consisted of 95 subjects, 58% of whom were workers in a private institution, mostly women (57%) and doctors (37%). Mean age was 42 years (SD 8.42), with a range between 24 and 60 years. Regarding education, 41% reported having a postgraduate degree, distributed between specialists (22%), masters (17%) and doctors (2%). High blood pressure was the most prevalent chronic disease (Table 1).
Regarding employment, the mean length of service in that particular service was 9.6 years (SD 7.3) and average length of service overall was 14.7 years (SD 8.4). It was found that the mean working hours per day was 11 h (SD 5.7), 5 days per week, with a total of 47 h (SD 21.6) average work per week, with a minimum of 18 and a maximum of 102 h work per week (7 subjects reported over 96 h of work per week).
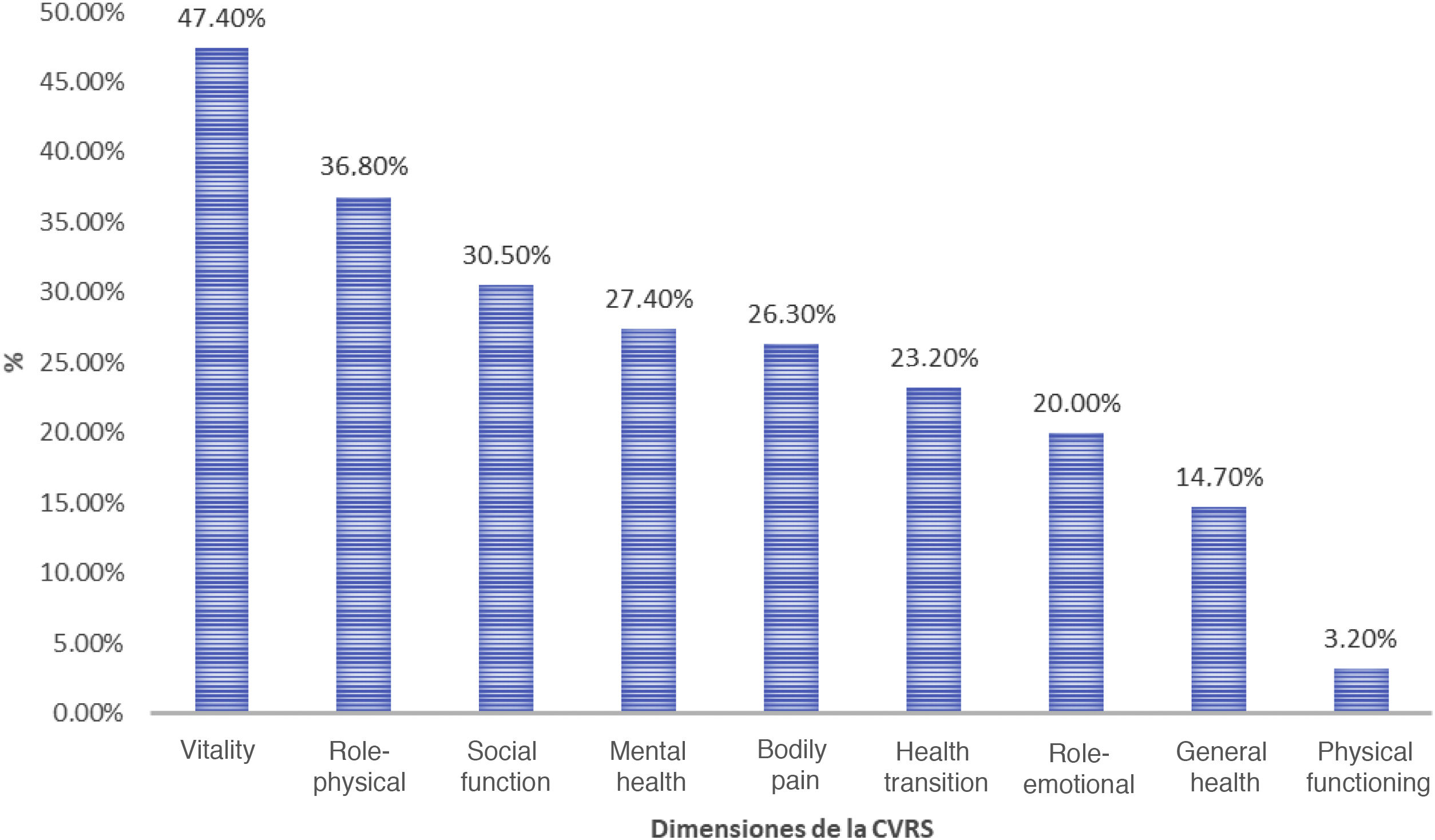
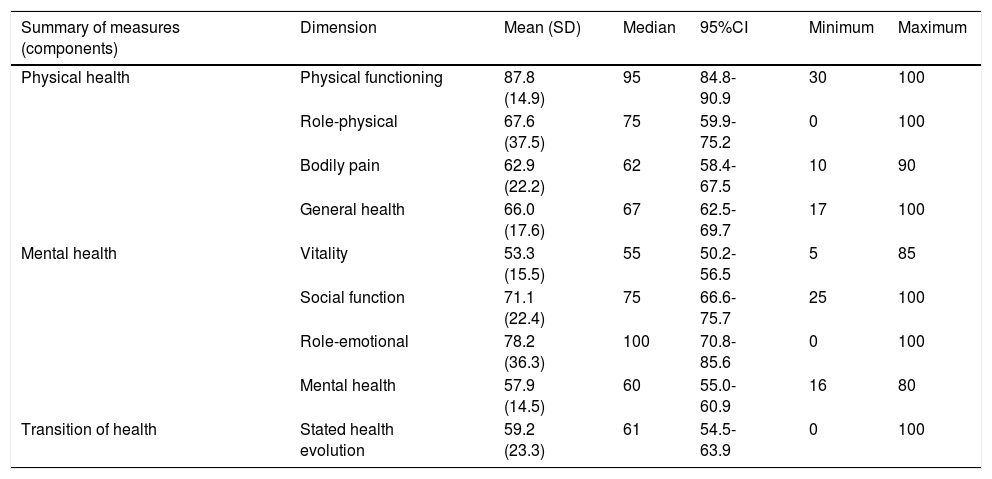
Regarding HRQoL, the dimension vitality was perceived as the poorest, with a mean of 53.3 (SD 15.5; 95%CI: 50.2-56.5), and physical functioning scored the best, with a mean of 87.8 (SD 14.9; 95%CI: 84.8-90.9) (Table 2). The dimensions of vitality, mental health and transition of health showed a mean which categorised them as “at risk” of presenting a low HRQoL (50 ± 10).
Behaviour of the health-related quality of life dimensions.
| Summary of measures (components) | Dimension | Mean (SD) | Median | 95%CI | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Physical health | Physical functioning | 87.8 (14.9) | 95 | 84.8-90.9 | 30 | 100 |
| Role-physical | 67.6 (37.5) | 75 | 59.9-75.2 | 0 | 100 | |
| Bodily pain | 62.9 (22.2) | 62 | 58.4-67.5 | 10 | 90 | |
| General health | 66.0 (17.6) | 67 | 62.5-69.7 | 17 | 100 | |
| Mental health | Vitality | 53.3 (15.5) | 55 | 50.2-56.5 | 5 | 85 |
| Social function | 71.1 (22.4) | 75 | 66.6-75.7 | 25 | 100 | |
| Role-emotional | 78.2 (36.3) | 100 | 70.8-85.6 | 0 | 100 | |
| Mental health | 57.9 (14.5) | 60 | 55.0-60.9 | 16 | 80 | |
| Transition of health | Stated health evolution | 59.2 (23.3) | 61 | 54.5-63.9 | 0 | 100 |
SD: Standard Deviation; 95%CI: 95% Confidence Interval.
Of all participants, 11.57% considered that their health was OK or poor; 7.36% believed that they got more ill than other people and 22% considered that their health was worse now than one year previously. Physical functioning was the dimension with the best general assessment, with 96.8% of participants presenting scores above 50, whilst the dimension of vitality scored the worst, with 47.4% of the sample having scores below 50. The complete data are shown in Fig. 1, Graph I.
On applying the Mann-Whitney-Wilcoxon U test for independent samples, no statistically significant differences were found in any of the dimensions comprising HRQoL, according to the type of hospital, public and private (p > .05). Regarding gender, women had higher means in dimensions such as physical role (57.2 vs. 74.6; p = .05), general health (62.3 vs. 68.6; p = .05) and social function (65.4 vs. 75.0; p = .02). People under 40 years (n = 38) gave a higher score to the physical function dimension (91.1 vs. 85.7; p = .03), and those diagnosed with a chronic disease gave lower scores to physical functioning (78.4 vs. 89.8; p = .007), Role-physical (53.1 vs. 70.5; p = .05), bodily pain (52.0 vs. 61.1; p = .03), general health (52.3 vs. 68.8; p = .001), social function (60.1 vs. 73.4; p = .03) and mental health (51.0 vs. 59.3; p = .02) dimensions.
The Kruskal-Wallis test was applied to identify statistically significant differences in the means of the variables with more than 2 categories, finding with respect to the profession that nursing technicians presented with better general health, with a mean of 72.9, compared with doctors and graduates in nursing, with 62.9 and 63.7, respectively (p = .03).
Regarding work load shedule, in general the higher the workload hours the lower the HRQoL dimension means although these differences were not statistically significant.
Analysing the relationship between length of service and HRQoL in general higher means were found (better HRQoL) in those with under 10 years of service, followed by a decline after 11 years, which later increased. The differences in means were statistically significant in role-physical dimensions (66.3 vs. 60.1 vs. 85.5; p = .05), bodily pain (65.9 vs. 57.3 vs. 70.0; p = .024), vitality (56.6 vs. 46.6 vs. 62.3; p < .001), social function (73.5 vs. 64.5 vs. 81.5; p = .019) and mental health (61.2 vs. 51.6 vs. 66.1; p < .001).
DiscussionThe quality of life and health status of healthcare professionals have been considered highly relevant elements for occupational health departments due to the relationship between carrying out their role as carer and the higher risk of stress, burnout and poor quality of life, which condition professional performance and lead to higher rates of absenteeism.25
The findings of this study differ from studies with healthcare workers, where their health status is better than the population mean. Regarding the above, Burgos-Díez et al. compared the means of the dimensions comprising the HRQoL in a sample of 542 healthcare workers with that of the general population, finding that in all dimensions, except pain, healthcare professionals gave a higher score compared with the general population.4 However, when comparing data with the mean of the general Argentinean population we found that, in all dimensions with the exception of the transition of health status, the population mean was above that of the professionals surveyed.24
A study conducted in Cuba by Trujillo et al., which included a survey of 1,700 workers from different areas, found that the health sector professionals scored the highest in the physical functioning dimension and the lowest in the general health dimension. The emotional role dimension obtained scores below the baseline.7 In contrast, Viltres-Rodríguez et al.conducted an epidemiological, cross-sectional study, which included 157 health professionals of general surgery services and they reported a better assessment of the mental component dimension than the physical one,26 contrasting with this study, where a better evaluation in the physical component was found.
Long working days and heavier workload are related to the mental and physical health of workers, as referred to in other similar studies.26,27
Fernandes-Souza et al., in a study conducted in Brazil, the objective of which was to assess the factors associated with quality of life in a sample of 40 intensivist nurses, found that 22.5% perceived their quality of life to be bad and 27.5% were dissatisfied with their health,28 whilst in our study 11.57% considered that their health was OK or poor and 7.36% believed that they would fall ill more than other people.
One study conducted in Madrid, which included a sample of 52 ICU professionals, found there was a relationship between the high levels in the 3 dimensions comprising burnout (emotional exhaustion, depersonalization and personal fulfilment) and a poor physical/mental health and subjective/psychological well-being.29 This helped to recognize the importance of measuring HRQoL as a means of monitoring and preserving workers’ health, serving as an indicator for generating interventions which would help to improve it.
Among the limitations of this study is that it is cross-sectional in nature, there is no profile of the evolution of the health status of the respondents. Also the limitations of a study based on the completion of surveys must be considered, where questions may be misunderstood or completion may be incomplete. However, the respondents were asked to fill out the surveys fully and we proceeded according to the guidelines of the construct for analysis of missing data. Finally, we would recommend increasing sample size for future studies, incorporating more units of analysis (ICU) and subjects.
ConclusionsAnalysis of the HRQoL profile revealed that the dimension of vitality was the worst perceived and physical function the best. Also, the dimensions comprising the physical component presented with a better evaluation compared with those of the mental component. The variables of gender (man); age (> 40 years); presence of chronic diseases; qualification (doctor); working load hours (> 40 h weekly) and length of service (> 11 years) were associated with the perception of HRQoL. There was a better assessment of the dimensions of the physical component rather than the mental one.
Measuring HRQoL of professionals is important, not just at the beginning of the study but throughout it, in order to perform an analysis of the variations in health status over a period of time.
It is necessary to implement strategies aimed at reducing the impact of work activities on the mental and physical health of health professionals, establishing strategies for health promotion and prevention of known psychosocial and ergonomic risks, and adapting the workload and working days to preserve the integrity of doctors and nurses working in intensive care units.
We would recommend that future studies research into current stress markers in ICUs and how heavily each one is perceived by the workers and also that follow-up be carried out to identify variations in the professionals’ health status and any related factors.
FinancingThis study was financed by funds from the authors.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Canova-Barrios C, Oviedo-Santamaría P. Calidad de vida relacionada con la salud en trabajadores de unidades de cuidados intensivos. Enferm Intensiva. 2021;32:181–188.