To determine the attitude of the nursing professionals of an Intensive Care Unit regarding the effects of open visiting on the daily activities of the patient, their family and professionals, and also to determine their contribution to the current open visiting policy.
MethodA cross-sectional descriptive study was performed, with a non-probabilistic discretionary sampling. The sample comprised nursing professionals of the aforementioned Unit. They were given a questionnaire with 26 items and an open question to evaluate their suggestions.
Results101 nursing professionals took part in the study, of the 120 working in the Unit under study. Seventy-five point two percent state that the nursing team has to postpone or modify their work due to the presence of the family and 89.9% that their presence produces a physical and psychological burden on the staff. Eighty percent think that the visit exhausts the family and 84.2% that the family feels obliged to remain with the patient. Ninety-four percent think that the effect of the presence of the family depends on the patient and the family.
ConclusionsMost of professionals have a negative opinion about the policy of open visits, showing some reluctance when it comes to flexible visiting hours, although they admit that an unrestricted schedule in this type of units implies some benefit for the patient and the family.
Conocer la opinión de los profesionales de enfermería de una Unidad de Cuidados Intensivos Polivalente (UCI) respecto a los efectos de la visita abierta en el paciente, en la familia y en la actividad diaria de los profesionales, así como sus aportaciones a la actual política de visitas abiertas.
MétodoEstudio transversal, descriptivo, mediante muestreo discrecional no probabilístico. La muestra estuvo formada por profesionales de enfermería de la citada Unidad. Se les entregó un cuestionario con 26 ítems, desarrollado y adaptado por Marco et al., además de una pregunta abierta.
ResultadosLa tasa de participación fue del 84% de los profesionales de la unidad (101/120). El 75,2% manifestó que el equipo de enfermería tiene que posponer o modificar su trabajo debido a la presencia de la familia y el 89,9% que su presencia produce una carga física y psíquica al personal. El 80% pensaba que la visita agota a la familia y el 84,2% que la familia se siente obligada a permanecer con el paciente. El 94% opinó que el efecto de la presencia de la familia depende del paciente y de la familia.
ConclusionesLa mayoría de los profesionales han tenido una opinión negativa hacia la política de visitas abiertas, mostrando cierta reticencia a la hora de flexibilizar los horarios de visita; aunque admitieron que un horario sin restricciones en este tipo de unidades supone cierto grado de beneficio para el paciente y la familia.
What is known?
Visiting hours have traditionally been restricted in intensive care units (ICU). Several studies have shown the importance that the needs of relatives are met to improve the quality of care and satisfaction of patients and their families.
What does this paper contribute?
Several studies show that most professionals are resistant to flexible visiting hours and open visiting policies, although they accept that unrestricted visiting in ICU could be beneficial for patients and families.
Implications for practice
We considered this research necessary to determine the obstacles encountered by ICU nursing staff in caring for the critical patient with the continuous presence of patients’ family members within the unit. This would contribute decisively to implementing appropriate care plans for each family, involving them in the care of the patient and tailoring care to both patients and relatives, with benefits for the professionals as well. It is essential to further scientific study into the humanisation of the care provided in the ICU, directing efforts towards training professionals in communication skills that promote closer, more individualised, and humane treatment.
The admission of a patient to an ICU puts family members in a difficult, often unexpected, situation which changes usual relationship patterns and requires adaptation. In addition, the ICU is a hostile environment where alarms, dependence on machines and high numbers of tubes and connections add to the anxiety of patients’ families.1 Historically, ICUs have had restricted visiting hours, based on protecting the patient, as patients receive care in an exclusive and individualised manner. The predominance of a technological, patient-centred culture makes it more difficult to ensure closeness between patients and relatives.2
The desire to visit the patient frequently is one of the main needs identified by relatives3 and positive effects are also observed in both, such as reduced anxiety and an increased sense of wellbeing. Similarly, contact with people they know reduces confusion and agitation and is associated with a lower incidence of delirium in accompanied patients.4 In fact, contact with relatives is considered one of the most effective non-pharmacological interventions in the prevention of delirium and is used as a resource in many units.5
One of the many studies that attempt to reflect the preferences of the patients themselves regarding visits from their relatives,6 concludes that patients express greater satisfaction with a flexible organisation adapted to their own needs and those of their family members. The presence of family members provides emotional support and a sense of security when facing procedures that may cause patients fear.7 These benefits may also have an impact in reducing the length of stay in ICU8 and enable greater communication between staff and relatives.
In relation to these findings, professionals working in intensive care units are starting a change in trend towards encouraging contact with the patient and satisfying these needs of relatives, by implementing reception protocols or introducing flexible visiting hours.5,8–11
These measures make it possible, on the one hand, to include the family in the care of the critically ill patient and, on the other, to turn family members into recipients of care.12 However some unease is observed among nursing professionals regarding caring with relatives and the role they play in the care process.2
In our country, Marco et al.7 analysed the relationship between nurses' beliefs and their attitudes to the effect of the open visiting implemented in their unit on patients, relatives, and nurses. They concluded that the views and attitudes towards the beneficial effect of open visiting on the patient, family and professionals are consistent. In contrast, other studies report an increased workload for ICU workers and some delay in the performance of duties.13 Difficulties in communication between professionals and families may cause distancing, generating uneasiness among professionals and some frustration among relatives.13 More recent studies, such as that of Sánchez-Vallejo et al.,14 show an increase in staff satisfaction, but also indicate that they need to complete their training in psychological aspects such as communication management with families.
Another study by Simon et al.15 which included 201 nurses with the aim of analysing ICU visiting policies, found that official policies were restrictive in 70% of cases. However, 78% of these nurses claimed to be flexible in applying visiting rules and most applied these rules based on their own decisions in assessing the needs of the patient and the nurses themselves. However, there are frequent references by some authors highlighting the important role of nurses in the care of relatives due to their ongoing presence with patients.11,12It is therefore necessary to find a balance between the needs of relatives and those of staff to improve the quality of care provided in ICU.
Visiting policies vary greatly in adult ICUs as they depend on the geographical and cultural area. Sweden has the highest percentage of ICUs with open visiting hours (70%), while in some countries such as Italy it is only 1%.16
The most recent study on open visiting policy in Spain was published in 2015.8 It shows that no major changes have occurred in the last decade, as currently 9.8% of ICUs have open visiting and only 4% have a 24-h open door system.
The aim of the present study was to describe the opinion of ICU nurses in this hospital on the effects of open visiting on patients, family members and the daily activity of professionals. In addition, we sought to obtain qualitative information on the perceptions of ICU nurses regarding the current visiting schedule.
MethodThe present study was conducted in a polyvalent ICU of a hospital in Asturias where there has been an open visiting regime for the last four years, in which relatives may stay at the patient's side for extended periods. We found no studies that assess the perception of nursing staff regarding open visiting in units that have extended visiting.
Study designCross-sectional descriptive observational study carried out in a polyvalent ICU of a hospital in Asturias, using a self-administered questionnaire.
ScopeIn the ICU under study, critical patient care is provided in four units each containing 10 beds, two of which are isolation units with sliding glass doors and only eight of which are staffed by nurses for the admission of patients, who can be fully occupied at times of peak demand. The nurse-patient ratio is 1:2 and 1:4 for auxiliary nursing care technicians (TCAE).
On admission, the family can visit their relative for a few minutes, at which time the doctor informs them of the patient’s current condition. They are given an information leaflet, showing the referring doctor, the bed where the patient has been admitted, and the telephone number for information, if desired, on the patient’s state of health, with a note that this will be discreet to preserve data confidentiality.
Visiting hours are uninterrupted from 12:30 p.m. to 9:00 p.m. Two people are allowed to stay at a time, and they may exchange visits with other family members as many times as they wish. In the event of an emergency or a technical procedure, family members will be moved to the waiting room until notified. Visits by children under the age of eight are not recommended due to psychological impact and possible transmission of infection. However, if the clinical situation of the patient allows, children may make short visits, always accompanied by an adult.
Medical briefings take place from Monday to Friday at 12:30 p.m. and at weekends and holidays at 5:00 p.m., always inside the patient's bay and without the presence of the nurse in charge of the patient. Nursing information is provided at the request of relatives and is limited to basic care and the general condition of the patient.
The nurses work in three shifts: morning, afternoon, and evening. There is another fixed shift in the mornings to reinforce the service during hours of peak workload.
SubjectsThe target population comprised all nursing professionals (TCAE and nurses) working in the ICU in April 2017.
Inclusion criteria followed those found in similar studies: experience in the unit of at least six months and agreeing to participate voluntarily in the study. Staff working a fixed morning shift were excluded from the study, as there is less interaction with the family during this shift.
Data collectionA self-administered questionnaire was used for data collection during the fieldwork phase, given by the principal investigator to the nursing professionals in the intensive medicine department of the hospital. The questionnaire was completed without the presence of the investigator.
The scale used to analyse the opinions of the nursing team was developed and adapted by Marco et al.7 based on the results of the studies by Kirchhoff et al. de 199317 and Simpson et al. de 1996.18 The reliability analysis for this scale resulted in a Cronbach's alpha of .77. The author’s permission was sought to use the questionnaire before the study. A data collection sheet was prepared with six socio-demographic questions and a Likert-type scale with 26 developed items and four possible responses. The questionnaire collected information on the effect of open visiting on patients, relatives, and the nursing team itself. We also wanted to collect information using an open question on the current visiting system to gather options for improvement and explore future lines of research.
After assessing the scale of the nursing professionals’ opinions on open visiting with its different indicators, the abovementioned authors of the validation of the questionnaire proposed inverting the score of the negative questions, to then obtain a mean score for each of the areas. The minimum and maximum score for each of the three areas would be 10 and 40 points for the patient area, 7 and 28 points for the family area, 9 and 36 points for the professional area, with an average of 25, 17.5 and 22.5 points, respectively. The total score of the scale would be between 26 and 104 with a mean of 65 points.
Data analysisFirst, the Kolmogorov-Smirnov test was used to analyse the normality of the variables, and then descriptive statistics were used: frequency measures for the qualitative variables (frequency and relative frequency), measures of central tendency (mean) and dispersion (standard deviation, maximum and minimum) for the quantitative variables. Inferential statistics were then performed to analyse the relationship between the variables of interest, using the Student’s t-test, X2 test and analysis of variance (ANOVA) as appropriate. SPSS (Statistical Pack for Social Sciences) version 24 software was used for the calculations. Statistical tests were considered significant if the critical level observed was less than 5% (p < .05).
Ethical considerationPrior to the fieldwork, the relevant permissions were requested from the Management and Nursing Management of the study hospital and the Research Ethics Committee when they consented the study, which was registered as study no. 71/17. Once granted, the department supervisors were informed, showing the authorisation to undertake the work. The questionnaires were preceded by informed consent to participate.
ResultsSocio-demographic variables of the sample of ICU nurses under studyThe study population comprised 120 nursing professionals. A total of 116 questionnaires were returned, because it was impossible to access the remaining professionals due to their heavy workload. The final sample consisted of 101 questionnaires, a participation rate of 84%. Fig. 1 shows the process followed until the final study sample was set up.
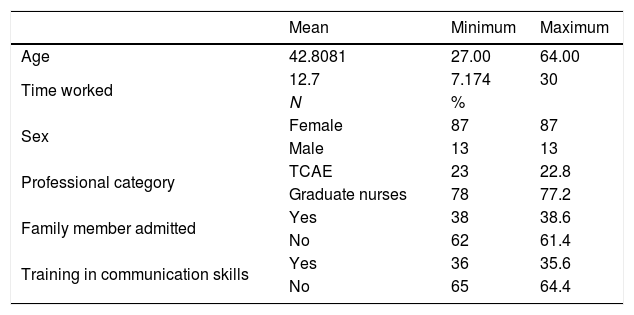
Table 1 shows the socio-demographic data of the professionals surveyed. The mean age of the study sample was 42.8 (standard deviation [SD] 8.4) years and the mean time working in the ICU was 12.7 (SD 7.0) years. At some point, 38.6% had had a family member admitted to intensive care. Thirty-five point six percent reported having received training in communication skills.
Sociodemographic characteristics of the professionals.
| Mean | Minimum | Maximum | |
|---|---|---|---|
| Age | 42.8081 | 27.00 | 64.00 |
| Time worked | 12.7 | 7.174 | 30 |
| N | % | ||
| Sex | Female | 87 | 87 |
| Male | 13 | 13 | |
| Professional category | TCAE | 23 | 22.8 |
| Graduate nurses | 78 | 77.2 | |
| Family member admitted | Yes | 38 | 38.6 |
| No | 62 | 61.4 | |
| Training in communication skills | Yes | 36 | 35.6 |
| No | 65 | 64.4 |
TCAE: auxiliary nursing care technicians.
Distribution by sex was mostly female, 87% were female. By professional category, 77% were nurses and 22.8% were TCAEs.
Descriptive analysis of the opinions of the nursing professionals on open visiting in the ICU under studyThe results were grouped into two groups to simplify the presentation of the data and for correct statistical analysis of the data. Responses including “agree” and “strongly agree” under the statement “agree” and those including “disagree” and “strongly disagree”, under the statement “disagree”, as established by Marco et al..7
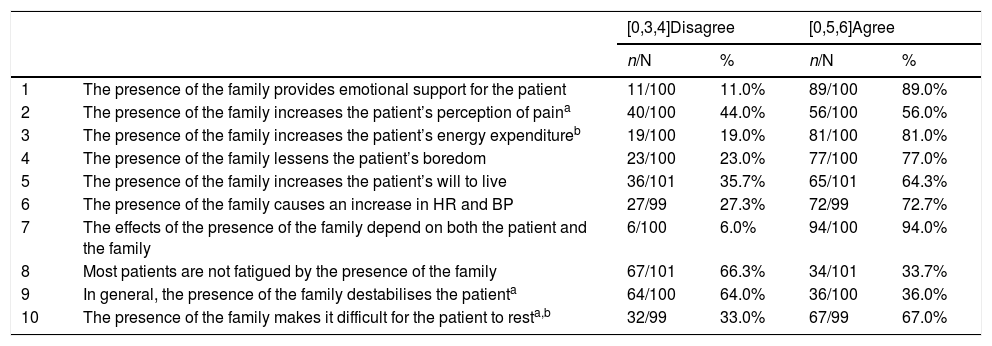
Regarding the perception of the effect of family visiting on the patient, 89% of the professionals agreed that the presence of the family provides emotional support to the patient, and 94% considered that the effect of the family depends on both the patient and the family itself. Fifty-six percent of the professionals agreed that the presence of the family increased the patient's perception of pain, with statistically significant differences (p = .033), and older professionals were more likely to agree with this statement. In addition, the latter were significantly more likely to agree that visiting made the patient unstable (p = .011) and made it difficult for the patient to rest (p = .009).
Table 2 shows the results obtained regarding the perception of the effect of family visiting on the patient.
Perception of staff on the effect of open visiting on patients.
| [0,3,4]Disagree | [0,5,6]Agree | ||||
|---|---|---|---|---|---|
| n/N | % | n/N | % | ||
| 1 | The presence of the family provides emotional support for the patient | 11/100 | 11.0% | 89/100 | 89.0% |
| 2 | The presence of the family increases the patient’s perception of paina | 40/100 | 44.0% | 56/100 | 56.0% |
| 3 | The presence of the family increases the patient’s energy expenditureb | 19/100 | 19.0% | 81/100 | 81.0% |
| 4 | The presence of the family lessens the patient’s boredom | 23/100 | 23.0% | 77/100 | 77.0% |
| 5 | The presence of the family increases the patient’s will to live | 36/101 | 35.7% | 65/101 | 64.3% |
| 6 | The presence of the family causes an increase in HR and BP | 27/99 | 27.3% | 72/99 | 72.7% |
| 7 | The effects of the presence of the family depend on both the patient and the family | 6/100 | 6.0% | 94/100 | 94.0% |
| 8 | Most patients are not fatigued by the presence of the family | 67/101 | 66.3% | 34/101 | 33.7% |
| 9 | In general, the presence of the family destabilises the patienta | 64/100 | 64.0% | 36/100 | 36.0% |
| 10 | The presence of the family makes it difficult for the patient to resta,b | 32/99 | 33.0% | 67/99 | 67.0% |
BP: Blood pressure; HR: Heart rate.
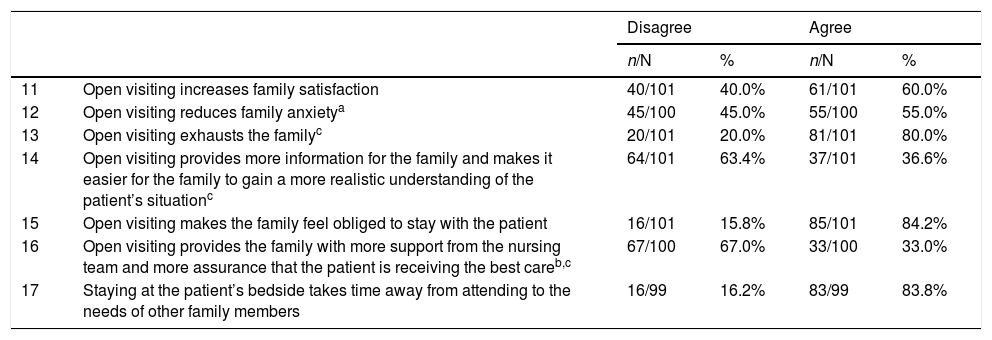
Regarding the perception of the effect of open visiting on the family itself, more than 80% of the professionals considered that open visiting exhausts the family, 84.2% felt that the family feels obliged to stay with the patient and 83.8% said it takes time from attending to the needs of other family members. Professionals who received training in communication skills, 72.2%, disagreed more (p = .009) that open visiting decreases family anxiety. However, a greater percentage of those who were trained in communication skills, 47.2% (p = .023), felt that open visiting provided the family with greater support from the nursing team and greater assurance that the patient was receiving the best care.
Significant differences were found (p = .04) according to professional category, with a higher percentage of the nurses, 84.6%, reporting that visiting exhausts the family compared to 65.2% of the TCAE.
Table 3 shows the results on the perception of the effect of visiting on the family itself.
Perception of staff on the effect of open visiting on the family.
| Disagree | Agree | ||||
|---|---|---|---|---|---|
| n/N | % | n/N | % | ||
| 11 | Open visiting increases family satisfaction | 40/101 | 40.0% | 61/101 | 60.0% |
| 12 | Open visiting reduces family anxietya | 45/100 | 45.0% | 55/100 | 55.0% |
| 13 | Open visiting exhausts the familyc | 20/101 | 20.0% | 81/101 | 80.0% |
| 14 | Open visiting provides more information for the family and makes it easier for the family to gain a more realistic understanding of the patient’s situationc | 64/101 | 63.4% | 37/101 | 36.6% |
| 15 | Open visiting makes the family feel obliged to stay with the patient | 16/101 | 15.8% | 85/101 | 84.2% |
| 16 | Open visiting provides the family with more support from the nursing team and more assurance that the patient is receiving the best careb,c | 67/100 | 67.0% | 33/100 | 33.0% |
| 17 | Staying at the patient’s bedside takes time away from attending to the needs of other family members | 16/99 | 16.2% | 83/99 | 83.8% |
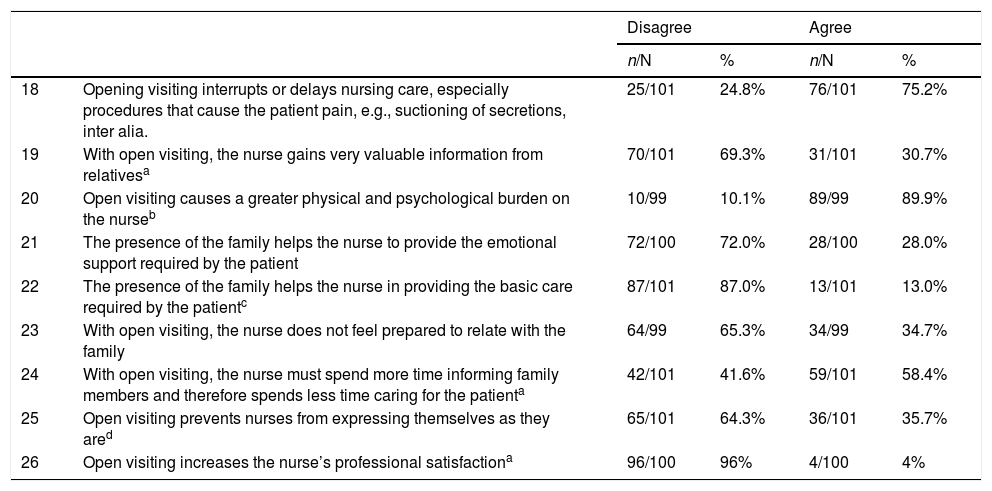
Finally, Table 4 shows the results obtained on the perception of the effect of open visiting on the professionals themselves. Of the participants in the study, 89.9% considered that it puts a greater physical and psychological burden on the nursing staff. Of the professionals with training in communication skills, 52.8% thought that with extended visiting staff obtain valuable information from relatives (p = .001) and 43.1% felt that it increases their professional satisfaction (p = .036). Moreover, 61.1% of the respondents with communication skills training felt that open visiting meant they did not have to devote more time to informing relatives and spend less time on patient care (p = .003).
Perceptions of staff on the effect of open visiting on professionals.
| Disagree | Agree | ||||
|---|---|---|---|---|---|
| n/N | % | n/N | % | ||
| 18 | Opening visiting interrupts or delays nursing care, especially procedures that cause the patient pain, e.g., suctioning of secretions, inter alia. | 25/101 | 24.8% | 76/101 | 75.2% |
| 19 | With open visiting, the nurse gains very valuable information from relativesa | 70/101 | 69.3% | 31/101 | 30.7% |
| 20 | Open visiting causes a greater physical and psychological burden on the nurseb | 10/99 | 10.1% | 89/99 | 89.9% |
| 21 | The presence of the family helps the nurse to provide the emotional support required by the patient | 72/100 | 72.0% | 28/100 | 28.0% |
| 22 | The presence of the family helps the nurse in providing the basic care required by the patientc | 87/101 | 87.0% | 13/101 | 13.0% |
| 23 | With open visiting, the nurse does not feel prepared to relate with the family | 64/99 | 65.3% | 34/99 | 34.7% |
| 24 | With open visiting, the nurse must spend more time informing family members and therefore spends less time caring for the patienta | 42/101 | 41.6% | 59/101 | 58.4% |
| 25 | Open visiting prevents nurses from expressing themselves as they ared | 65/101 | 64.3% | 36/101 | 35.7% |
| 26 | Open visiting increases the nurse’s professional satisfactiona | 96/100 | 96% | 4/100 | 4% |
Regarding open visiting placing a greater physical and psychological burden on the nurse, the professionals with more years of experience agreed significantly more with this statement (p = .012). Furthermore, statistically significant differences were also found according to the gender of the professional (p = .004), with 38.5% of the men agreeing that the presence of the family member helps the nurse in the provision of basic care compared to 9.3% of the women.
No statistically significant differences were found on these issues when comparing professionals who had or had not previously had a family member admitted to an ICU.
The differences found between those with communication skills training and those without were interesting. The professionals with these skills felt that nurses did not have to spend more time with the family and less with the patient, that they obtained valuable information from the relatives and that open visiting gave them greater professional satisfaction.
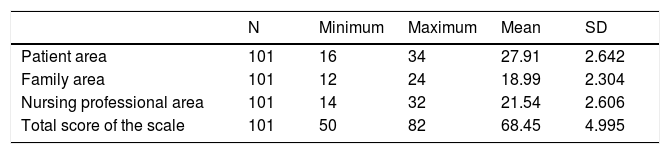
Analysis of the opinion of the nursing professionals on the current open visiting regime in the ICU under study in relation to the three areas of influence studied using the questionnaire. Including the SD showing the meanWhen calculating the mean score for each area of study of the questionnaire, as previously described in the methodology, we obtained a total mean score of 68.45 (SD 4.995) points. In the patient area, a mean value of 27.91 (SD 2.642) points was acquired, in the family area 18.99 (SD 2.304) points and in the professional area 21.54 (SD 2.606) points. A score above the mean would indicate, as discussed in the methodology section, the staff’s positive opinion on open visiting. Accordingly, the means obtained indicated that in general the respondents considered open visiting a positive factor for patients and family, but negative for professionals.
Table 5 shows the mean score for each of the areas making up the scale.
When comparing with the socio-demographic variables, we observed statistically significant differences (p = .018) only between the area of the family and the professional category of the ICU professionals, with the TCAEs obtaining a lower mean score.
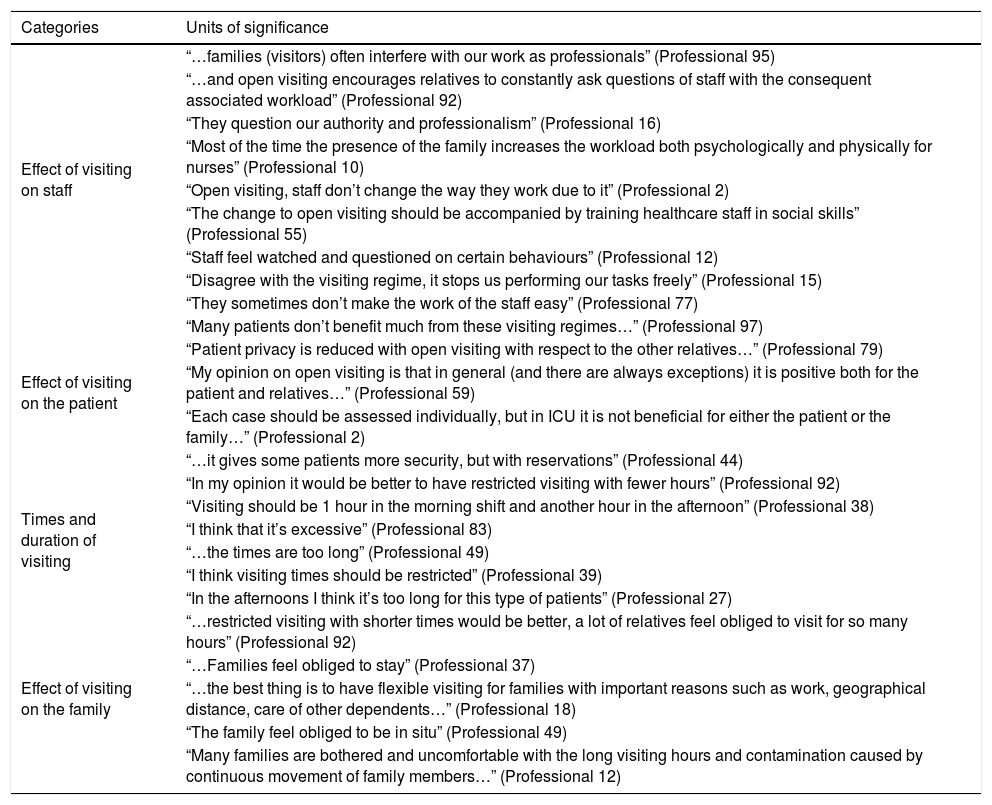
Qualitative analysis of the professionals’ suggestionsOf the 101 respondents, 35.64% (n = 36) completed the open question. The comments were grouped according to the four main categories found: effect of open visiting on the patient, the family, the professionals and times or duration of visits.
The category with the most suggestions related to the effect of visiting on professionals, with a total of 16 comments (44%). In this category, the professionals emphasise the interruption of nursing care, the increase in physical and psychological workload, and the interference of the families in the work of professionals.
There were 12 comments (33%) alluding to opinions on the effect on the patient. One of the most repeated observations regarded adapting visiting hours to the situation of each patient and family. Another aspect that is repeated is the importance of patient privacy, reporting that other relatives, who spend several hours in the units, are aware of the other patients, thus affecting their privacy and intimacy.
Regarding visiting times and duration, 10 comments (27%) were collected where the majority suggested more restricted visiting hours, reducing those during the morning and afternoon shift.
Finally, eight comments (22%) were collected referring to the effect on the family, most of them negative, reflecting that because of the extended visiting hours the family feels obliged to stay with the patient.
Table 6 shows the comments of the professionals.
Qualitative matrix of the opinions expressed by the professionals.
| Categories | Units of significance |
|---|---|
| Effect of visiting on staff | “…families (visitors) often interfere with our work as professionals” (Professional 95) |
| “…and open visiting encourages relatives to constantly ask questions of staff with the consequent associated workload” (Professional 92) | |
| “They question our authority and professionalism” (Professional 16) | |
| “Most of the time the presence of the family increases the workload both psychologically and physically for nurses” (Professional 10) | |
| “Open visiting, staff don’t change the way they work due to it” (Professional 2) | |
| “The change to open visiting should be accompanied by training healthcare staff in social skills” (Professional 55) | |
| “Staff feel watched and questioned on certain behaviours” (Professional 12) | |
| “Disagree with the visiting regime, it stops us performing our tasks freely” (Professional 15) | |
| “They sometimes don’t make the work of the staff easy” (Professional 77) | |
| Effect of visiting on the patient | “Many patients don’t benefit much from these visiting regimes…” (Professional 97) |
| “Patient privacy is reduced with open visiting with respect to the other relatives…” (Professional 79) | |
| “My opinion on open visiting is that in general (and there are always exceptions) it is positive both for the patient and relatives…” (Professional 59) | |
| “Each case should be assessed individually, but in ICU it is not beneficial for either the patient or the family…” (Professional 2) | |
| “…it gives some patients more security, but with reservations” (Professional 44) | |
| Times and duration of visiting | “In my opinion it would be better to have restricted visiting with fewer hours” (Professional 92) |
| “Visiting should be 1 hour in the morning shift and another hour in the afternoon” (Professional 38) | |
| “I think that it’s excessive” (Professional 83) | |
| “…the times are too long” (Professional 49) | |
| “I think visiting times should be restricted” (Professional 39) | |
| “In the afternoons I think it’s too long for this type of patients” (Professional 27) | |
| Effect of visiting on the family | “…restricted visiting with shorter times would be better, a lot of relatives feel obliged to visit for so many hours” (Professional 92) |
| “…Families feel obliged to stay” (Professional 37) | |
| “…the best thing is to have flexible visiting for families with important reasons such as work, geographical distance, care of other dependents…” (Professional 18) | |
| “The family feel obliged to be in situ” (Professional 49) | |
| “Many families are bothered and uncomfortable with the long visiting hours and contamination caused by continuous movement of family members…” (Professional 12) |
From the results obtained, we can deduce that the nursing staff see open visiting as a problem, especially regarding its effect on professionals, as the results suggest they need to reorganise their work to overcome shortcomings in their communication skills. These skills would help them to relate better to the patient’s family, providing emotional support to both the family and the patient. Therefore, it seems clear that it is important to incorporate family care as an objective in care planning, which would help recovery and improvement in the critically ill patient.
DiscussionIn this study, which sought to describe the opinions of the nursing team on the effects of open visiting on the patient, the family, and the professionals themselves, we obtained a high rate of participation, most respondents being women aged between 31 and 50 years. These percentages are very similar to those of the study by Ayllón et al.19
The mean professional experience was 12.7 (SD 7.17) years. Although in the literature consulted, professionals with little experience in ICU had a more positive opinion regarding flexible visiting hours,20 this was not the case in the present study, perhaps due to an ingrained culture of a restricted family visiting policy.
Furthermore, having had a family member admitted to ICU did not change the professionals' opinion of open visiting.
Most of the respondents believe that the presence of the family has beneficial effects on the patient’s emotional wellbeing and that it also increases the patient’s will to live. These results were comparable with those obtained by Simpson et al.,18 apart from the will to live where they found different results to those of our study.
Psychological care should be included in the care of the critically ill patient, since according to the study by Gómez et al.21 patients report emotional disturbances during their stay in ICU such as anxiety, stress, or “intensive care syndrome”. The latter consists of fluctuating levels of consciousness, behavioural abnormalities and memory disturbances,22–25 which can negatively affect26 the patient's recovery and increase the length of their hospital stay.27 Other studies describe that relatives have the resources and information to facilitate this type of emotional care.28 From the results, it seems that the nursing team is aware of this, attaching an important role to the family in providing emotional support to the patient.
Most of the professionals reported that the presence of the family increases the patient's perception of pain and destabilises them. However, studies have shown that interactions of professionals with patients destabilise the patient more than the family.21,23 Therefore, it seems that the perception of this negative influence is not supported by the available evidence, and we should insist on the correct training of the staff in the units that implement this type of open visiting.
If we look at the professional category of the respondents, most of those who thought that the family increased the patient's energy expenditure and made it difficult for them to rest were TCAEs. In this regard, half of the professionals surveyed by Simpson et al.18 also thought that open visiting increased the patient’s energy expenditure and in turn altered their haemodynamics. The differences between categories may again underline the need for specific training in the units to provide a holistic approach to patient and family care.
In terms of the effect of visiting on relatives, many studies highlight the benefits for the patient and for the relatives themselves, as it increases family satisfaction, reduces anxiety, and provides greater information and real knowledge of the patient's situation.23,29,30 In our study, we obtained results similar to those found in the abovementioned studies. However, 84.2% of the professionals felt that family members may feel obliged to stay with the patient for longer, and do not consider, for the most part, that the nursing team provides support to the family. In addition, 94% of the professionals thought that the effects of open visiting depend on the characteristics of the patient and the visitor. Similar results were reported by Santana et al.30 and Whitton et al.,31 who found it important to personalise and individualise the care of the patient and family.
As already explained, the relationship of helping between the nurse and the family is encompassed within the emotional needs described by relatives with a loved one in an ICU.32 Therefore, the nursing professional should also focus their attention on relatives to help them adapt to the new situation and thus contribute to their wellbeing. There are several studies in this regard that propose including welcome protocols for families, and even the development of care plans for them.33–35
Most of the professionals in the study (90%) considered that visiting places a greater physical and psychological burden on nurses. The professionals with more work experience in ICU assessed the presence of the family as a burden, similar results were obtained by Ayllón et al.19 However, only 13% of those surveyed said that the presence of the family helps the nurse to perform basic care, finding significant differences in terms of gender, the men agreed more. In this regard, the involvement of family members in patient care has been shown to reduce their anxiety and help them to understand what is happening in the ICU and is positive for the patient.10
However, the equipment and unfamiliar environment of the ICU may inhibit relatives from contact with the patient, and the nursing staff should encourage them to perform some basic care. Here again, the development of protocols for family care seems necessary and it would be interesting to include family members in this basic care.
In contrast, a high percentage of respondents (75%) felt that the presence of the family interrupts or delays care, results similar to those obtained in the study conducted by Marco et al.7 There are also several studies that show that professionals feel uncomfortable when observed by relatives.24,25 This may lead professionals to reduce the frequency of care or postpone it.
The differences found between the professionals with communication skills and those without are interesting. Those with communication skills felt that the nurse did not have to spend more time with the family and less time with the patient. They felt that they gained valuable information from the family and that open visiting gave them greater professional satisfaction. ICU nurses often lack communication skills, as they are often dealing with patients with whom it is difficult to communicate due to their critical situation.35 There are several skills that favour good communication with the patient or family: listening, empathy, compassion, assertiveness, and emotional support.31,36 Moreover, these communication skills are very important in the relationship with relatives as they perceive it as good quality of care.37
Several studies show that most nurses do not believe they have the necessary knowledge to meet the emotional needs of relatives,38 which, together with the potential lack of knowledge of the medical information provided by doctors, may make nurses avoid contact with families.36 With the exception of the professionals with communication skills as mentioned above, a large proportion of the professionals felt that they did not gain valuable information from families. In other studies, nurses trained in communication skills did obtain information from families that enabled them to better plan care.7,18,20,39
A possible line of research in this regard would be to improve the communication skills of ICU professionals through meetings with the relatives of patients admitted to the unit and specific training in this area. These proposals coincide with the studies by Daly et al.39 and Sargeant et al.40
In this improvement, it might be interesting to suggest to relatives that a family member be delegated as a reference person for the nursing team,5 so that they can participate, if they wish, in the basic care of the patient, and receive information on the patient’s progress. This would also help to meet the emotional needs of the patient and assist the nursing professionals.
ConclusionsThe evidence obtained in our study shows the reluctance of most professionals towards flexible visiting hours and open visiting policies, although they admit that unrestricted visiting in the ICU may be beneficial for the patient and family.
FundingThe authors declare that they received no funding for this research.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank the nursing professionals of ICU 3-4-5-6, who selflessly collaborated with their participation in this study.
Please cite this article as: Alonso-Rodríguez A, Martínez-Villamea S, Sánchez-Vallejo A, Gallego-Lorenzo J, Fernández-Menéndez M. Perspectivas de los profesionales de enfermería de cuidados intensivos sobre las visitas abiertas en una UCI. Enferm Intensiva. 2021;32:62–72.