Neonatal units have undergone major changes as a result of the higher survival of premature babies and the greater complexity of treatments. They have also incorporated care focused on development and the family, improving humanising features and the quality of care. However, all of these changes have not always included a change in the workload of the personnel staffing these units.
In 2004 the Committee of Standards and the Governing board of the Spanish Society of Neonatology (SENeo) determined the care levels and recommendations of minimums for neonatal care,1 with which the care level of each centre could be defined in Spain, together with the technical and healthcare requirements of each level. This text has undergone several reviews, bearing in mind the changes experienced in neonatal care in the last few years.2,3
Among its care recommendations3 the SENeo establishes a minimum number of nurses with experience in neonatal care per patient, with 1:8-10 newborns in basic care, 1:3–4 in intermediate care, 1:2 in intensive care, increasing to 1:1 in the case of high technology (postoperative of high complexity, total exchange transfusion, peritoneal dialysis, hypothermia) and 2:1 in the case of extremely high technology (ECMO, haemofiltration). These recommendations are reflected in the report “Neonatal units. Quality standards and recommendations” published by the Ministry of Health, Social Services and Equality.4
Adequate provision of nurses in neonatal intensive care units (NICU) is highly complicated due to the variability in the number of patients admitted and their complexity, which leads to staff requirements changing over time.5 Flexibility in the number of nurses is a requirement, since inadequate numbers of staff may affect adverse results in our patients, and particularly the most vulnerable – the premature and low birth weight babies, and to poor family care. Numerous studies have demonstrated the association between a shortage of nurses and nursing auxiliaries and a higher risk of nosocomial infections and adverse clinical results.6–8 A shortage of nurses may lead to the non availability of time to dedicate to the newborn and the non completion of care centred upon the development and the family, with the known benefit these have on premature babies.
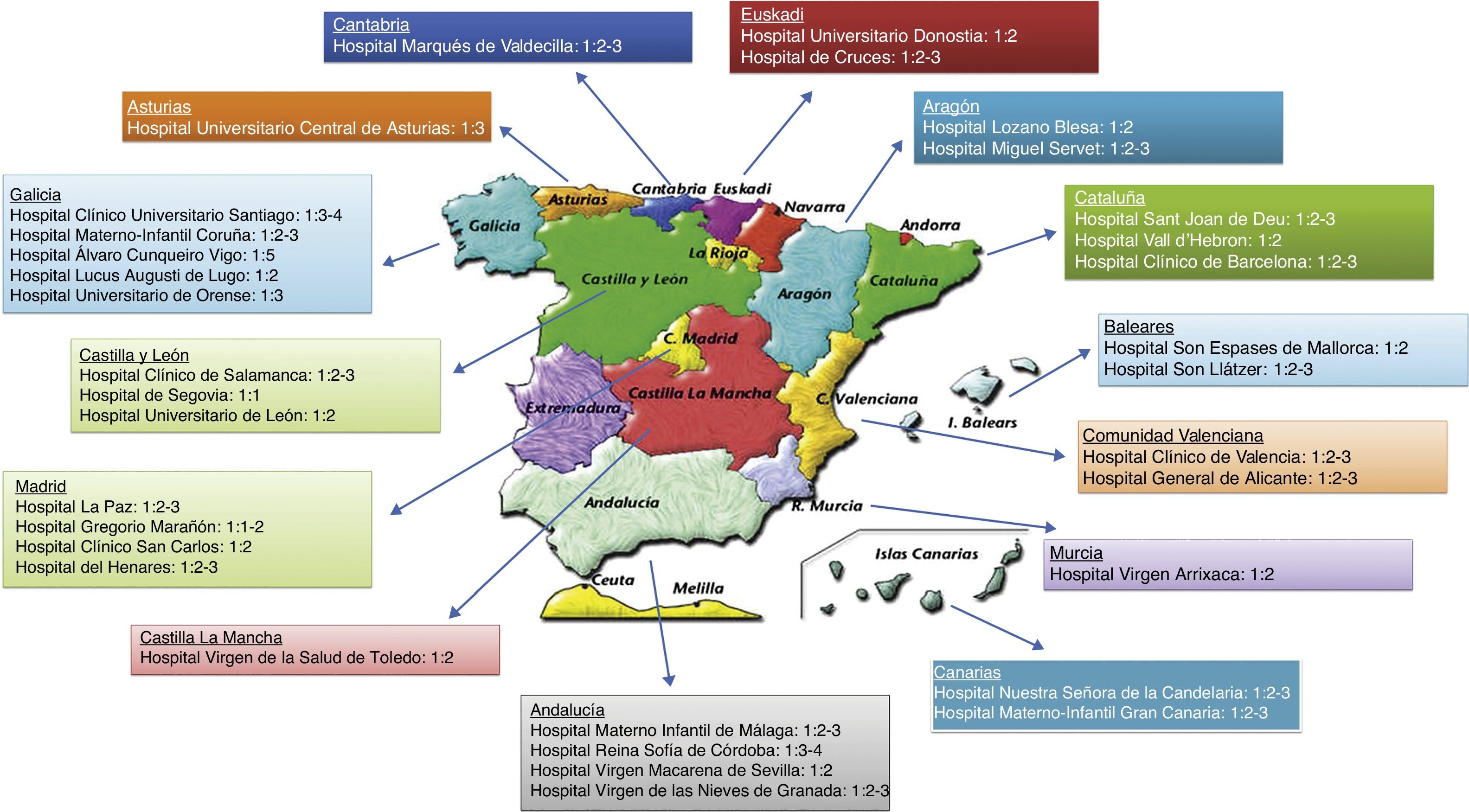
Our commitment to care quality for our patients resulted in designing an online survey to collect the data referring to the nurse-patient ratios in the NICU and intermediate care in Spanish hospitals, thereby discovering its true reality and whether it corresponded to the recommendations of the Ministry of Health, Social Services and Equality. This survey was distributed through the web site of the Spanish Society of Neonatal Nursing (SEEN for its initials in Spanish). High participation was achieved, often in the same hospital, and was undertaken by different nurses, collecting information from 35 hospitals corresponding to 14 autonomous communities, with no response being obtained from Extremadura, Navarra and La Rioja.
The corresponding results to the ratios of the NICU of each hospital are reflected in a map of Spain (Fig. 1). The mean nurse-patient ratio in NICU on a national level is 2.4 patients per nurse. In conditions of high complexity of patients the ratio usually drops to 1:1, as recommended by the Ministry.
Regarding intermediate care, the national level is one nurse for every 6.2 patients, with there being a great variability of results between the different Spanish hospitals, possibly due to the lack of a common term for this area.
We may state that despite the existence of several recommendations by the Ministry of Health, Social Services and Equality, which are well defined regarding nurse-patient ratios in the neonatal services (NICU and intermediate care), there is a fair amount of disparity of data throughout Spain, often due to criteria of financial saving, not based on care quality.
The current trend is towards personalised attention focused on development and the family, which has entailed a change in the type of care.9,10 This all has to be complemented with an increase in human resources to improve the number of patients a nurse is responsible for, guaranteeing more complete care to improve its quality. Care focused on development does not imply less staff, indeed the contrary. Educating parents and having healthcare session with them is also part of our functions as healthcare professionals and this involves having the time to implement this.
Please cite this article as: Fernández-Tuñas MC, Barrio-Tobío L, Couselo-García L, Pérez-Muñuzuri A. Variabilidad en la ratio enfermera-paciente en las unidades de cuidados intensivos neonatales y cuidados intermedios. Enferm Intensiva. 2020;31:46–47.